Syphilis is a bacterial infection caused by the spirochete Spirochete Treponema is a gram-negative, microaerophilic spirochete. Owing to its very thin structure, it is not easily seen on Gram stain, but can be visualized using dark-field microscopy. This spirochete contains endoflagella, which allow for a characteristic corkscrew movement. Treponema Treponema pallidum Treponema pallidum The causative agent of venereal and non-venereal syphilis as well as yaws. Treponema subspecies pallidum (T. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Primary syphilis begins with a chancre, a painless ulcer on the genitals. Progression to secondary syphilis manifests as a generalized maculopapular Maculopapular Dermatologic Examination rash Rash Rocky Mountain Spotted Fever, which includes the palms and soles. The development of tertiary syphilis can cause severe neurologic (neurosyphilis), cardiovascular, and/or gummatous disease. The diagnosis is through both treponemal and nontreponemal testing. Penicillin Penicillin Rheumatic Fever G is the antibiotic of choice. The duration of management varies based on the stage of the disease.
Last updated: Dec 27, 2025
Syphilis is a multistage disease. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship can present at any stage and infected individuals may not exhibit symptoms for years.

Primary, painless chancre of syphilis (T. pallidum infection)
Image: “Chancres on the penile shaft due to a primary syphilitic infection caused by Treponema pallidum 6803 lores” by M. Rein. License: Public Domain
Diffuse cutaneous lesions on the palms of a patient with secondary syphilis
Image: “Neurosyphilis: An Unresolved Case of Meningitis” by Ahsan S, Burrascano J. License: CC BY 3.0
Generalized maculopapular rash on the trunk of a patient with secondary syphilis
Image: “Early malignant syphilis” by Anais Brasileiros de Dermatologia. License: CC BY 4.0
Condyloma lata in a patient with secondary syphilis
Image: “11257” by Susan Lindsley. License: Public Domain
A gumma on the palate of a patient with tertiary syphilis
Image: “16762” by CDC. License: Public DomainIt is difficult to diagnose syphilis. However, specific labs and the correlation Correlation Determination of whether or not two variables are correlated. This means to study whether an increase or decrease in one variable corresponds to an increase or decrease in the other variable. Causality, Validity, and Reliability of history and examination results can lead to a diagnosis.
Definitive tests using obtained specimens (such as mucosal lesions). However, use is limited since the tests are not routinely available.
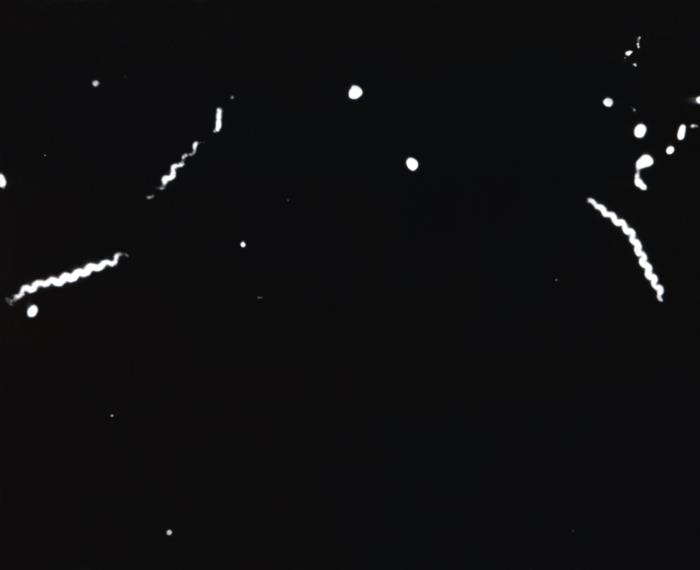
Darkfield microscopy of T. pallidum:
Corkscrew-shaped bacteria are seen.
For primary, secondary, or early-latent syphilis, the following antibiotics can be used:
For late-latent syphilis, tertiary syphilis, or syphilis of unknown duration, the following regimen is used: