Cardiac mechanics refers to how the heart muscle pumps blood and the factors that affect the heart's pumping function. Stroke volume Stroke volume The amount of blood pumped out of the heart per beat, not to be confused with cardiac output (volume/time). It is calculated as the difference between the end-diastolic volume and the end-systolic volume. Cardiac Cycle (the volume of blood pumped out during each contraction) is affected by 3 key factors: preload, afterload, and inotropy (also known as contractility). Preload is how much the ventricle has stretched by the end of diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle (and thus how much blood has filled the ventricles). Afterload is the pressures in the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy that ventricular contraction must overcome in order to open the aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy and eject blood into the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy. Inotropy is the strength of the muscle contraction itself (independent of the preload), which is primarily related to how much intracellular Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts)2+ is present.
Last updated: Nov 2, 2023
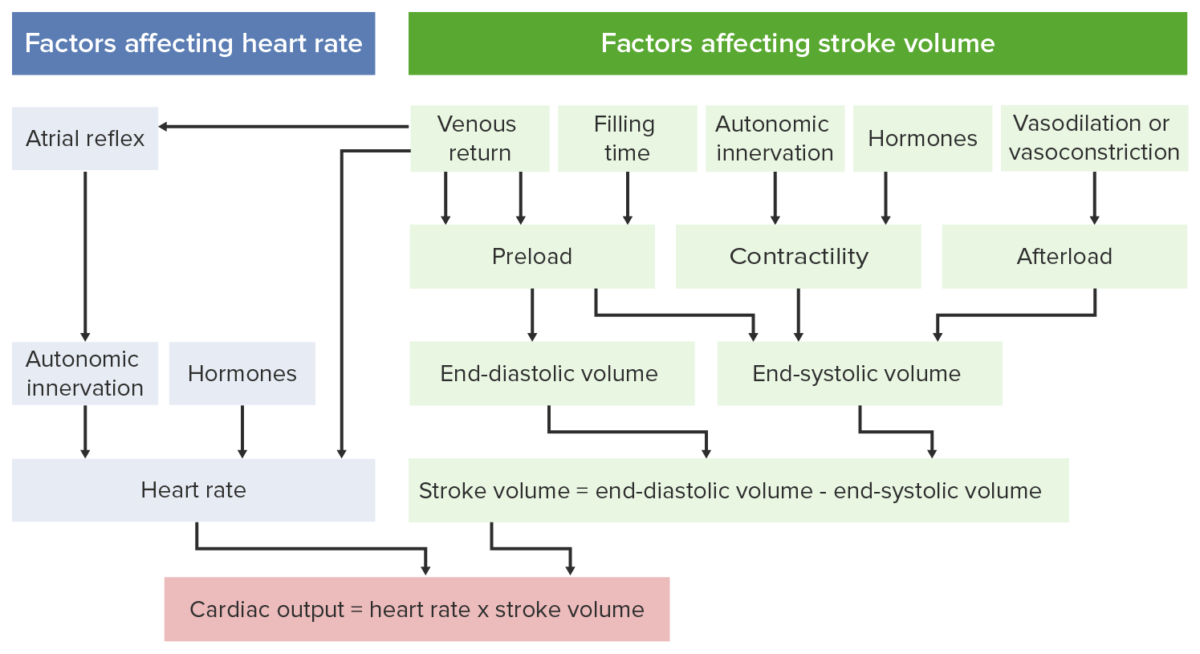
Factors in cardiac output
Image by Lecturio.Overview:
Phases:
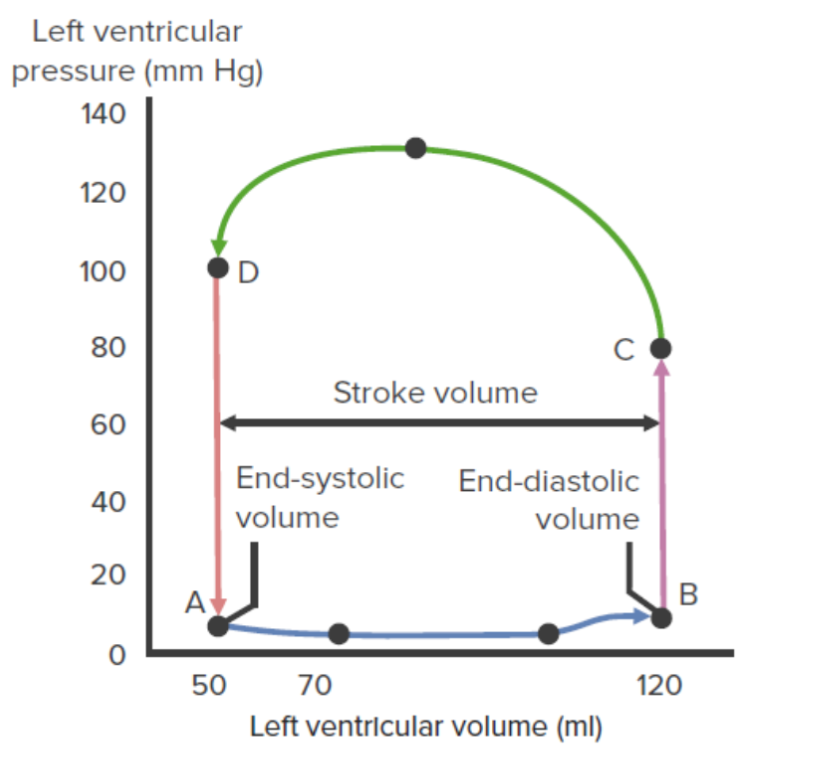
Left ventricular pressure–volume loop:
This diagram illustrates the relationship between left intraventricular pressure and volume throughout the cardiac cycle. The segment from point A to point B represents ventricular filling. The mitral valve opens at A and closes at B. The segment from point B to point C represents isovolumetric contraction. The aortic valve opens at C. The curved line from point C to point D represents ventricular ejection. The aortic valve closes at D. The segment from point D to point A represents isovolumetric relaxation.
Preload is a measure of how much the cardiomyocytes have stretched by the end of diastole Diastole Post-systolic relaxation of the heart, especially the heart ventricles. Cardiac Cycle. The Frank-Starling law is associated with preload effects on SV: ↑ preload = ↑ SV.
The length–tension relationship explains how the Frank-Starling law works. This law applies to striated muscle Striated muscle One of two types of muscle in the body, characterized by the array of bands observed under microscope. Striated muscles can be divided into two subtypes: the cardiac muscle and the skeletal muscle. Muscle Tissue: Histology: skeletal and cardiac muscles.
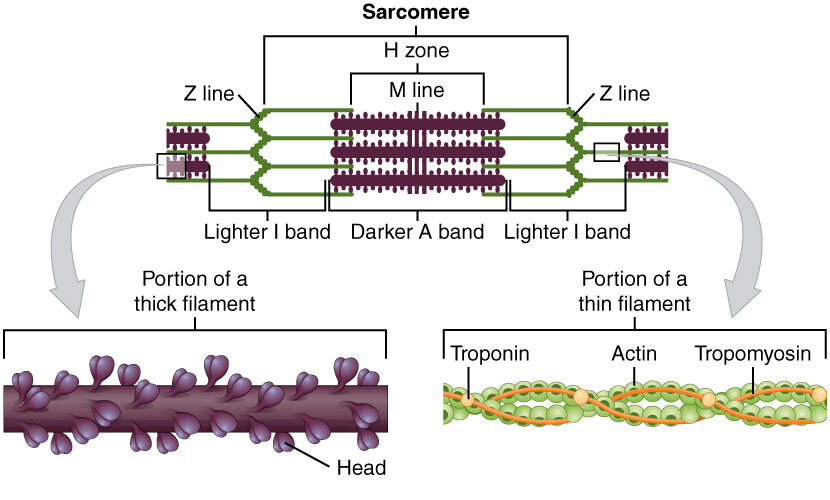
Diagram depicting the microscopic structure of sarcomeres, actin, and myosin
Image: “The sarcomere, the region from one Z-line to the next Z-line, is the functional unit of a skeletal muscle fiber” by OpenStax College. License: CC BY 4.0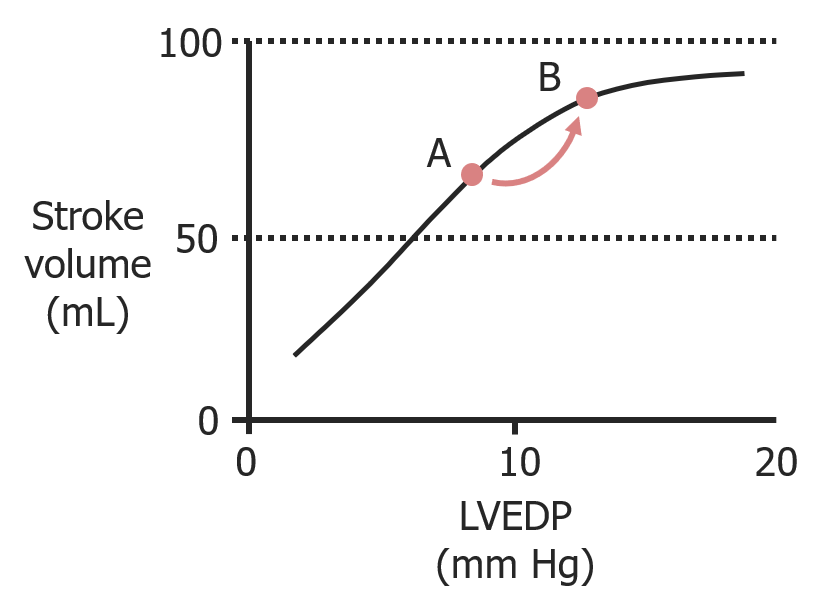
As left ventricular end-diastolic pressure (LVEDP) increases owing to increased filling, stroke volume increases as well.
Image by Lecturio.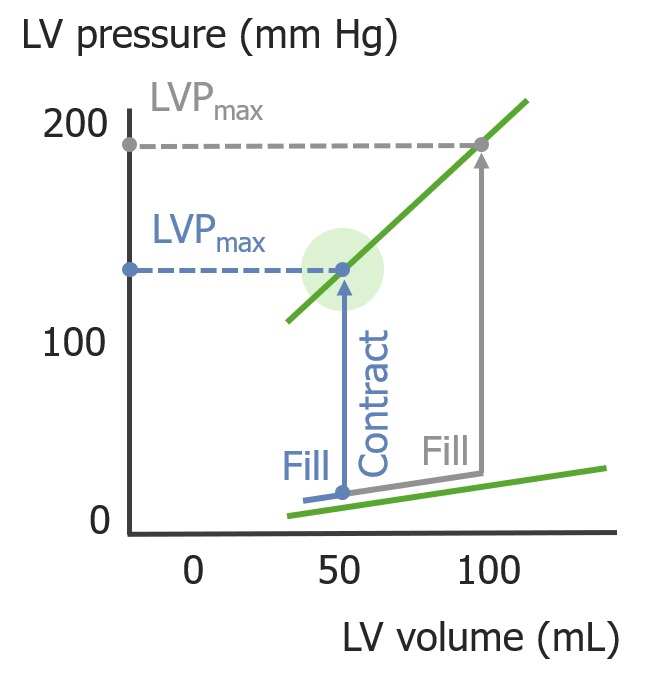
As the left ventricular (LV) volume increases during diastole, the LV pressure (LVP) generated during systole increases.
Image by Lecturio.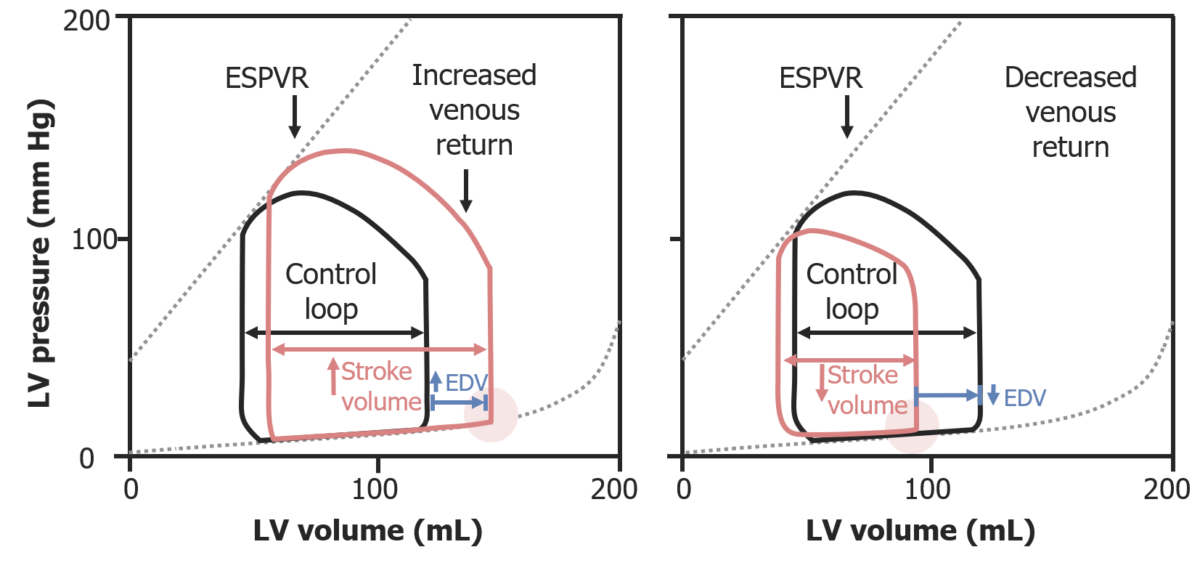
Pressure–volume loops illustrating the Frank-Starling law:
On the left, increased preload from increased venous return results in a greater EDV, which increases stroke volume. On the right, preload is reduced, and therefore, stroke volume is reduced.
ESPVR: end-systolic pressure–volume relationship
EDV: end-diastolic volume
Afterload is the resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing in the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy that prevents blood from leaving the heart. Afterload represents the pressure the LV needs to overcome to eject blood into the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy.
↑ Afterload:
↓ Afterload:
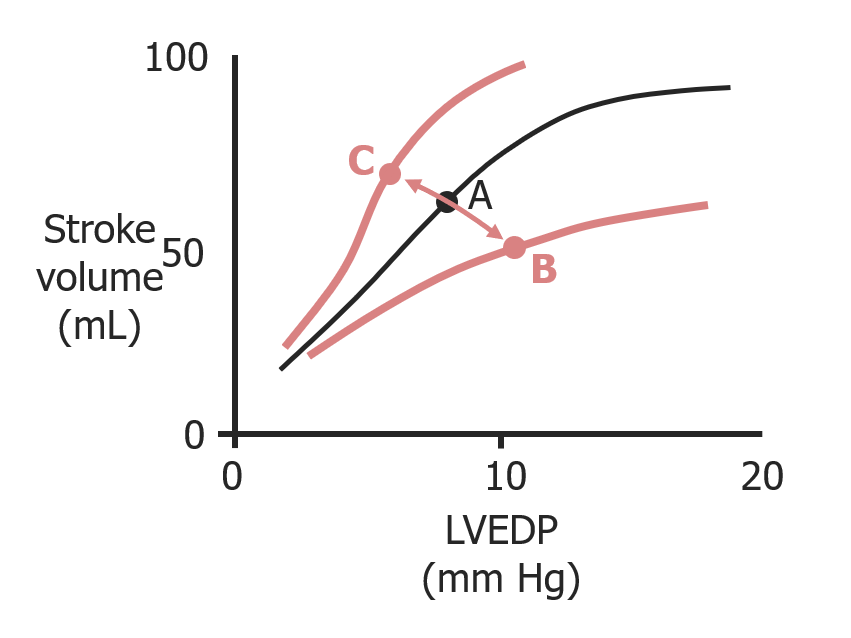
Frank-Starling curves and the effects of afterload on stroke volume and left ventricular end-diastolic pressure (LVEDP):
When afterload increases (A to B), preload increases (↑ LVEDP) but stroke volume decreases.
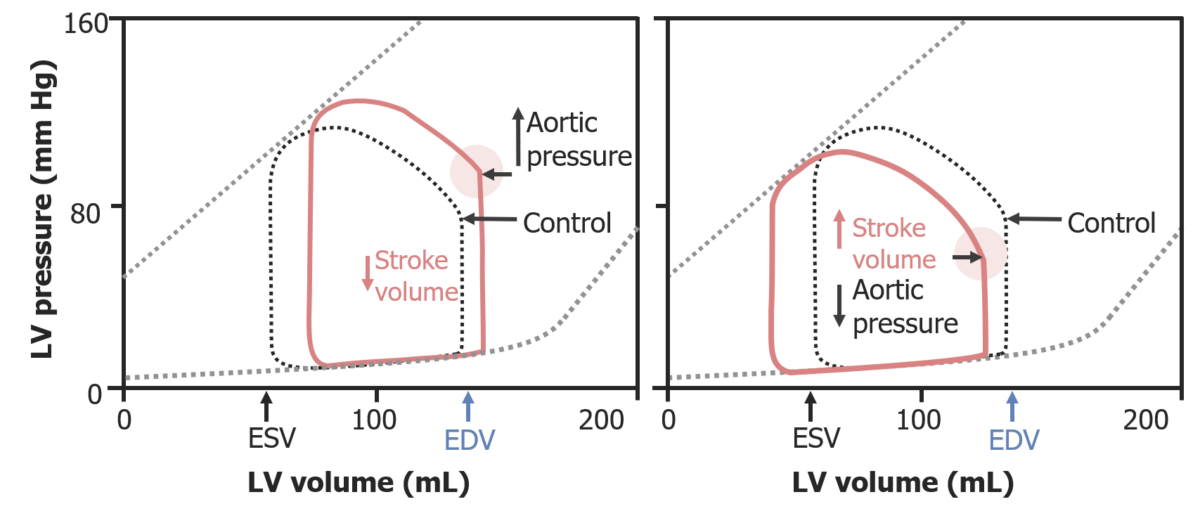
Pressure–volume loops illustrating the effects of afterload:
On the left, an increase in afterload (increased aortic pressure) requires higher pressures to be achieved during isovolumetric contraction; ultimately, this reduces stroke volume. On the right, a decreased afterload lowers the required pressure to open the aortic valve; this results in an increased stroke volume.
ESV: end-systolic volume
EDV: end-diastolic volume
Inotropy is a measure of the force of contraction, independent of changes in preload.
Inotropy is increased as a result of:
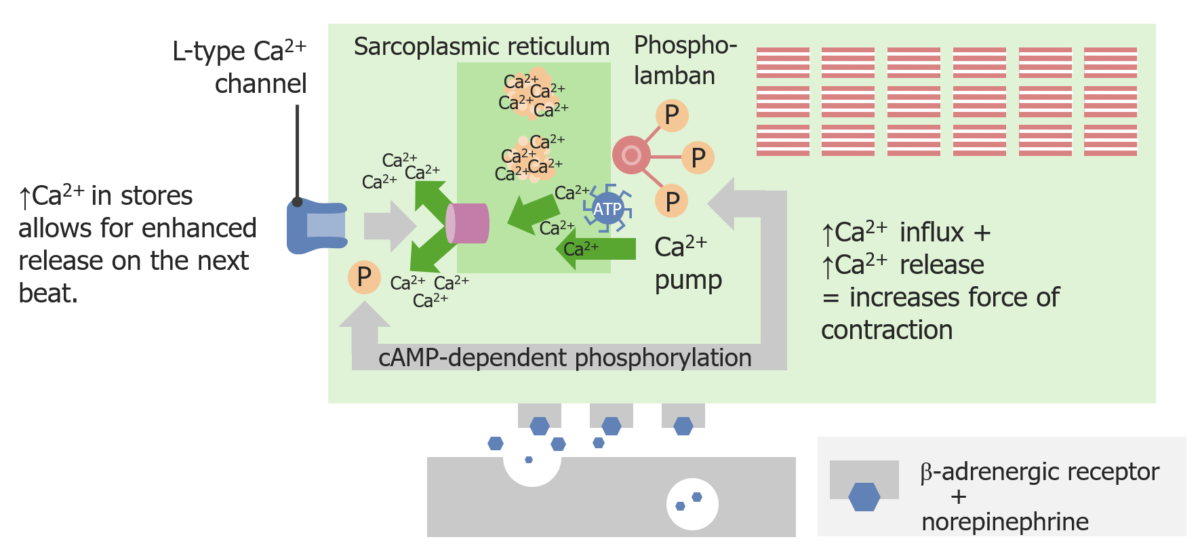
Sympathetic activation increases inotropy:
Norepinephrine binding to a β-adrenergic receptor generates cAMP, which causes the release of Ca2+ from the sarcoplasmic reticulum (SR). This provides more intracellular Ca2+ to bind to more myofilaments, leading to a greater force of contraction.
↑ Inotropy:
↓ Inotropy:
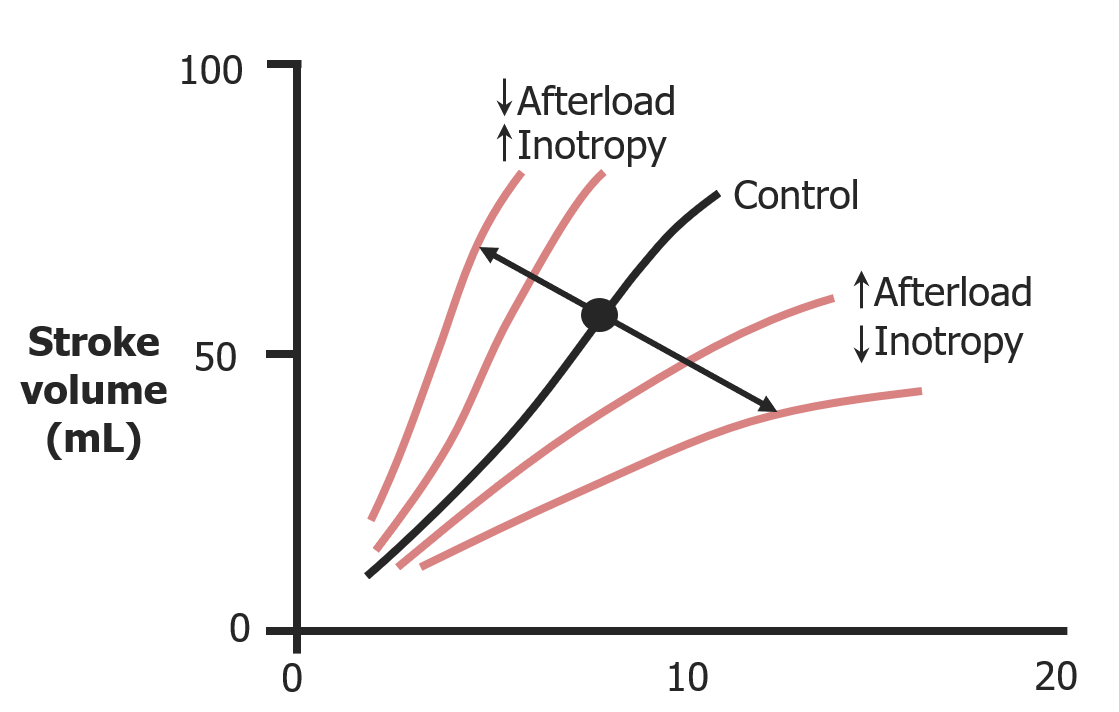
Effects of both inotropy and afterload on stroke volume
Image by Lecturio.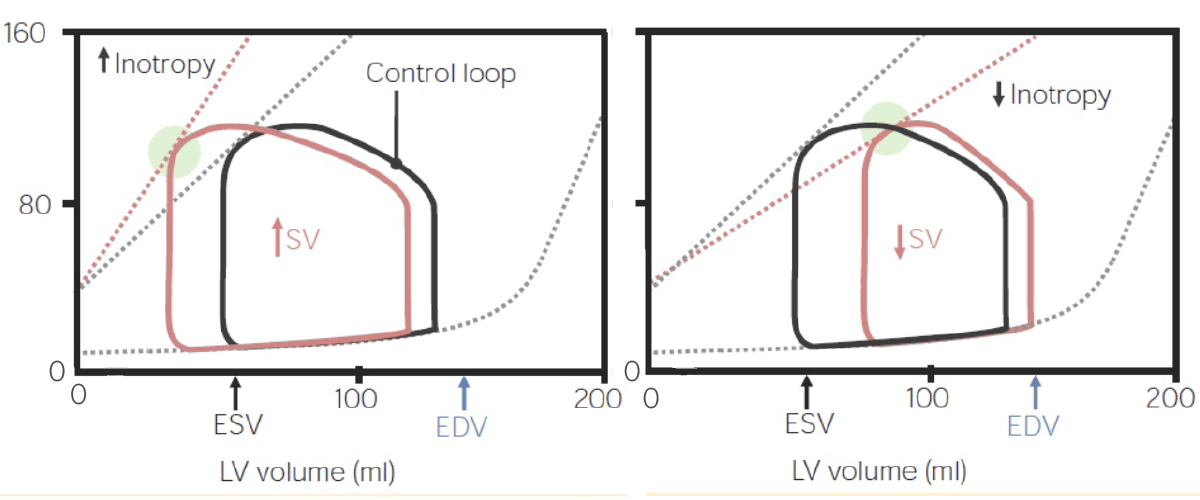
Pressure–volume loops illustrating the effects of inotropy:
On the left, as inotropy increases, so does the stroke volume, leading to a smaller end-systolic volume (ESV). On the right, as inotropy decreases, so does the stroke volume, so there is a larger volume of blood left at the end of systole.
The following are common conditions that affect cardiac mechanics.
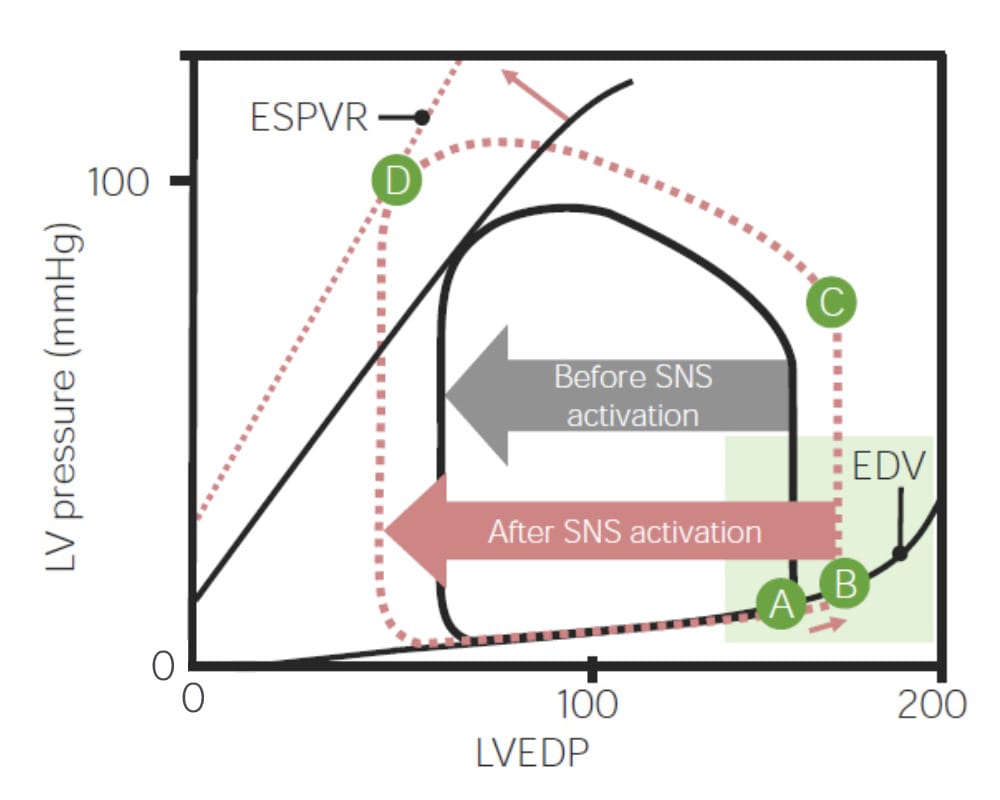
Pressure–volume loop, illustrating the changes that occur during the fight-or-flight response:
The end-systolic pressure-volume relationship (ESPVR) is such that, as end-diastolic volume increases (↑ preload) as result of sympathetic nervous system (SNS) activation, stroke volume increases owing to the Frank-Starling law. The SNS also increases inotropy, which also contributes to an increase in stroke volume.