Lateral medullary syndrome (also known as Wallenberg syndrome, posterior inferior cerebellar artery Posterior inferior cerebellar artery Cerebrovascular System: Anatomy ( PICA Pica Pica is an eating disorder characterized by a desire or recurrent compulsion to eat substances that are nonnutritive and not food. These compulsions and ingested substances are inappropriate for age or culture. Pica) syndrome, and vertebral artery syndrome) is a neurological constellation of symptoms and signs due to obstruction in vessels supplying the medulla, resulting in brainstem ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage or infarction. The most common cause is atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis in the posterior cerebral circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment, and the most reported symptom is a transient ischemic attack Transient ischemic attack Transient ischemic attack (TIA) is a temporary episode of neurologic dysfunction caused by ischemia without infarction that resolves completely when blood supply is restored. Transient ischemic attack is a neurologic emergency that warrants urgent medical attention. Transient Ischemic Attack (TIA) ( TIA TIA Transient ischemic attack (TIA) is a temporary episode of neurologic dysfunction caused by ischemia without infarction that resolves completely when blood supply is restored. Transient ischemic attack is a neurologic emergency that warrants urgent medical attention. Transient Ischemic Attack (TIA)) with dizziness or vertigo Vertigo Vertigo is defined as the perceived sensation of rotational motion while remaining still. A very common complaint in primary care and the ER, vertigo is more frequently experienced by women and its prevalence increases with age. Vertigo is classified into peripheral or central based on its etiology. Vertigo. With stroke/infarction, patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship also present with nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, loss of balance with gait Gait Manner or style of walking. Neurological Examination, instability, hoarseness Hoarseness An unnaturally deep or rough quality of voice. Parapharyngeal Abscess, and difficulty in swallowing Swallowing The act of taking solids and liquids into the gastrointestinal tract through the mouth and throat. Gastrointestinal Motility. The signs are dependent on the specific nuclei and fibers affected. Diagnosis is made by clinical exam and imaging with CT/MRI. Management is mostly supportive, including speech and occupational therapy Occupational Therapy Skilled treatment that helps individuals achieve independence in all facets of their lives. It assists in the development of skills needed for independent living. Fetal Alcohol Spectrum Disorder after acute intervention, as well as risk factor reduction for future ischemic events.
Last updated: Feb 7, 2023
Lateral medullary infarction (also known as Wallenberg syndrome, posterior inferior cerebellar artery Posterior inferior cerebellar artery Cerebrovascular System: Anatomy ( PICA Pica Pica is an eating disorder characterized by a desire or recurrent compulsion to eat substances that are nonnutritive and not food. These compulsions and ingested substances are inappropriate for age or culture. Pica) syndrome, and vertebral artery syndrome) is a neurological constellation of symptoms and signs due to decreased blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure in vessels supplying the medulla, resulting in brainstem ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage or infarction.
Components of the lateral medulla:
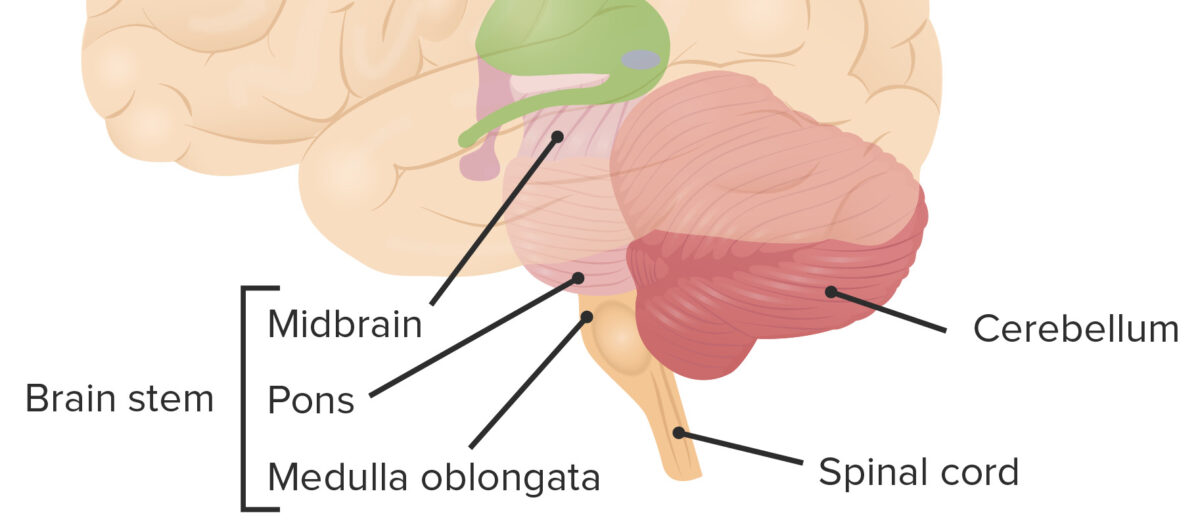
Location of cerebellum in relation to the other brainstem structures
Image by Lecturio.Blood supply:
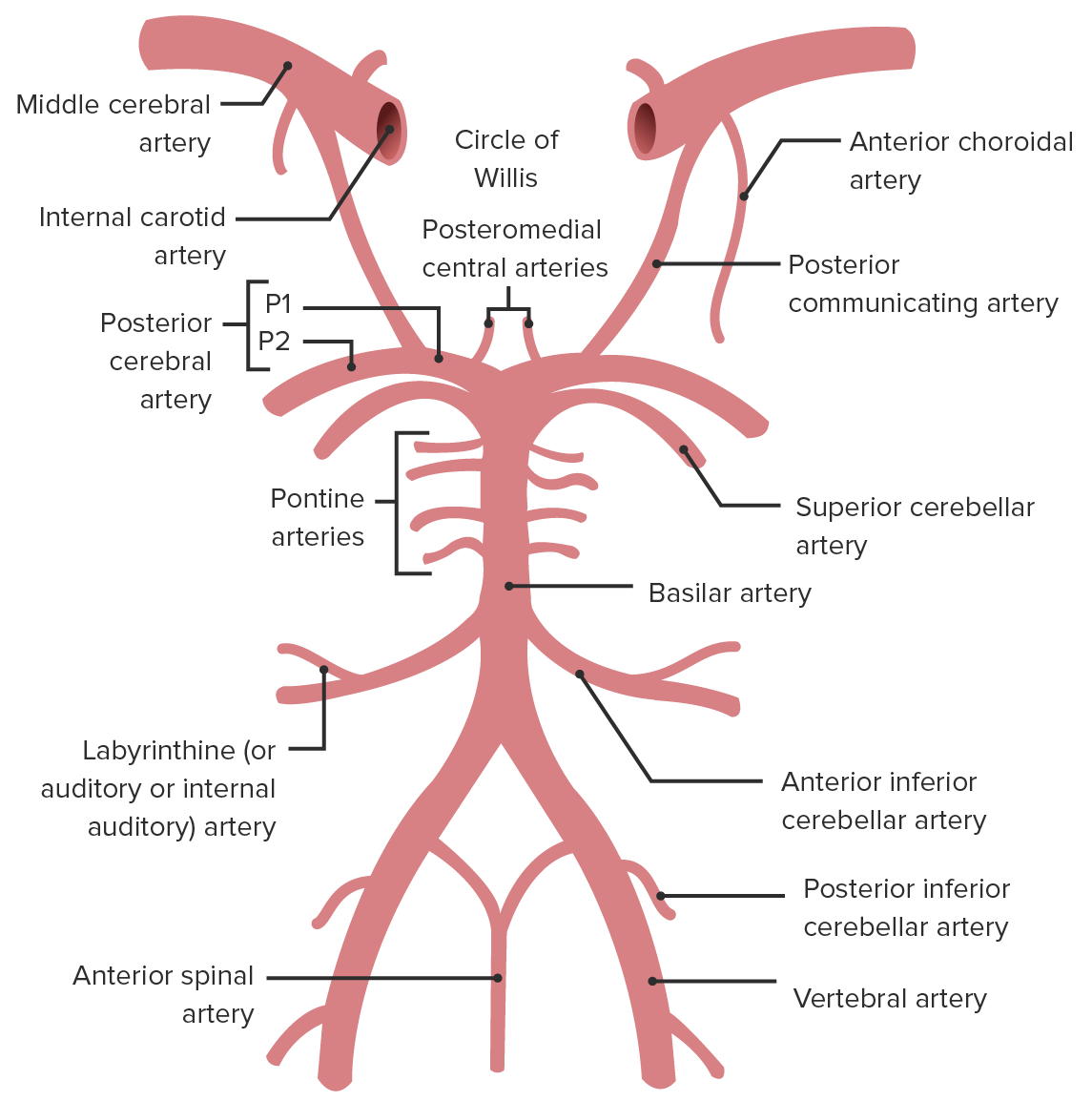
Locations of the vertebral artery, the posterior inferior cerebellar artery (PICA), the middle cerebral artery (MCA), and the basilar artery
Image by Lecturio.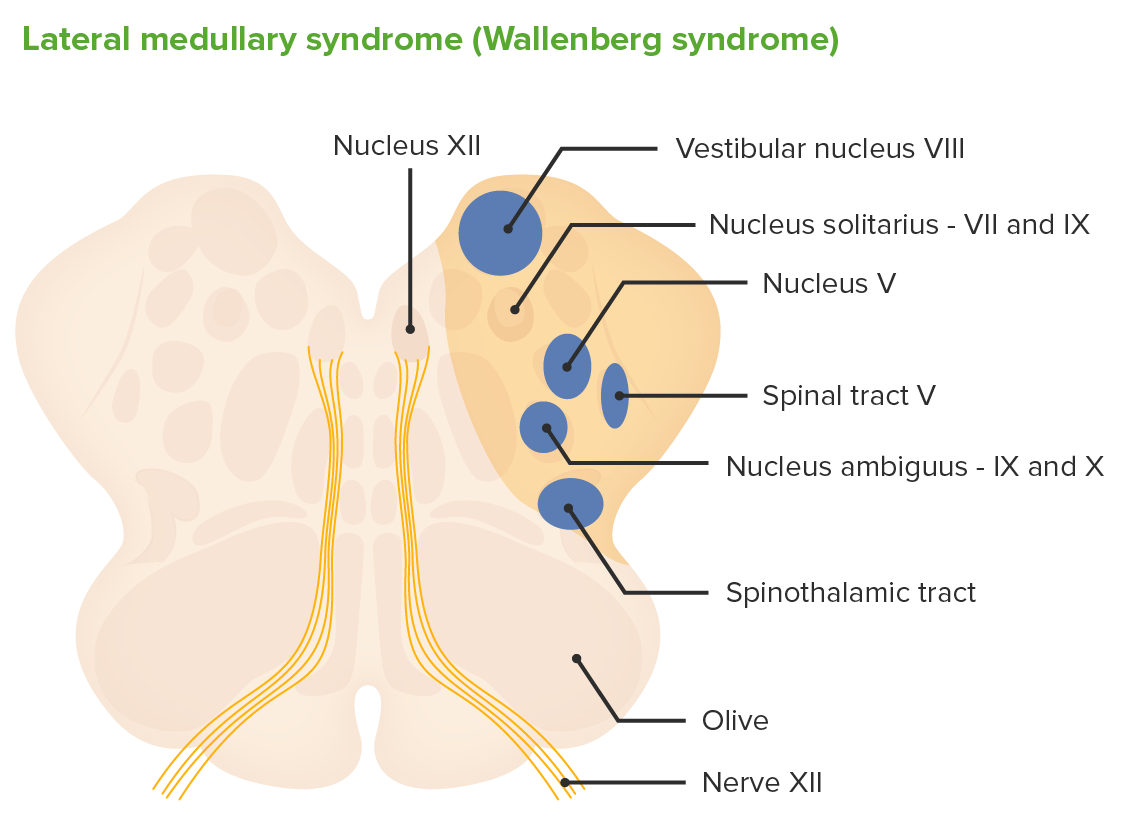
Cross-section through the medulla and structures affected by occlusion of the PICA causing lateral medullary syndrome (Wallenberg syndrome)
Image by Lecturio.A complete reduction in cerebellar blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure involving the PICA Pica Pica is an eating disorder characterized by a desire or recurrent compulsion to eat substances that are nonnutritive and not food. These compulsions and ingested substances are inappropriate for age or culture. Pica results in lateral medullary syndrome.
Wallenberg syndrome causes abnormalities in the vestibulocerebellar, sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology, bulbar, respiratory, and autonomic systems.
| Structure affected | Presenting symptoms |
|---|---|
| Spinothalamic tract | Contralateral loss of pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and temperature sensation in the trunk and limbs |
| Spinal trigeminal nucleus Nucleus Within a eukaryotic cell, a membrane-limited body which contains chromosomes and one or more nucleoli (cell nucleolus). The nuclear membrane consists of a double unit-type membrane which is perforated by a number of pores; the outermost membrane is continuous with the endoplasmic reticulum. A cell may contain more than one nucleus. The Cell: Organelles | Ipsilateral loss of pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and temperature in the face |
| Nucleus ambiguus Nucleus ambiguus Brain Stem: Anatomy | Dysphagia Dysphagia Dysphagia is the subjective sensation of difficulty swallowing. Symptoms can range from a complete inability to swallow, to the sensation of solids or liquids becoming “stuck.” Dysphagia is classified as either oropharyngeal or esophageal, with esophageal dysphagia having 2 sub-types: functional and mechanical. Dysphagia, dysphonia Dysphonia Difficulty and/or pain in phonation or speaking. Epiglottitis, and diminished gag reflex Gag Reflex Cranial Nerve Palsies (supply to the vagus and glossopharyngeal nerves is affected) |
| Inferior vestibular nucleus Nucleus Within a eukaryotic cell, a membrane-limited body which contains chromosomes and one or more nucleoli (cell nucleolus). The nuclear membrane consists of a double unit-type membrane which is perforated by a number of pores; the outermost membrane is continuous with the endoplasmic reticulum. A cell may contain more than one nucleus. The Cell: Organelles | Vertigo Vertigo Vertigo is defined as the perceived sensation of rotational motion while remaining still. A very common complaint in primary care and the ER, vertigo is more frequently experienced by women and its prevalence increases with age. Vertigo is classified into peripheral or central based on its etiology. Vertigo (same direction as the lesion), diplopia Diplopia A visual symptom in which a single object is perceived by the visual cortex as two objects rather than one. Disorders associated with this condition include refractive errors; strabismus; oculomotor nerve diseases; trochlear nerve diseases; abducens nerve diseases; and diseases of the brain stem and occipital lobe. Myasthenia Gravis, nystagmus Nystagmus Involuntary movements of the eye that are divided into two types, jerk and pendular. Jerk nystagmus has a slow phase in one direction followed by a corrective fast phase in the opposite direction, and is usually caused by central or peripheral vestibular dysfunction. Pendular nystagmus features oscillations that are of equal velocity in both directions and this condition is often associated with visual loss early in life. Albinism, vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia |
| Sympathetic fibers | Horner syndrome Horner syndrome Horner syndrome is a condition resulting from an interruption of the sympathetic innervation of the eyes. The syndrome is usually idiopathic but can be directly caused by head and neck trauma, cerebrovascular disease, or a tumor of the CNS. Horner Syndrome = miosis Miosis Pupil: Physiology and Abnormalities, ptosis Ptosis Cranial Nerve Palsies, anhidrosis |
| Inferior cerebellar peduncle Inferior cerebellar peduncle Cerebellum: Anatomy | Ataxia Ataxia Impairment of the ability to perform smoothly coordinated voluntary movements. This condition may affect the limbs, trunk, eyes, pharynx, larynx, and other structures. Ataxia may result from impaired sensory or motor function. Sensory ataxia may result from posterior column injury or peripheral nerve diseases. Motor ataxia may be associated with cerebellar diseases; cerebral cortex diseases; thalamic diseases; basal ganglia diseases; injury to the red nucleus; and other conditions. Ataxia-telangiectasia, dysmetria Dysmetria Cerebellar Disorders, dysdiadochokinesia Dysdiadochokinesia Difficulty with rapid alternating movements Cerebellar Disorders |
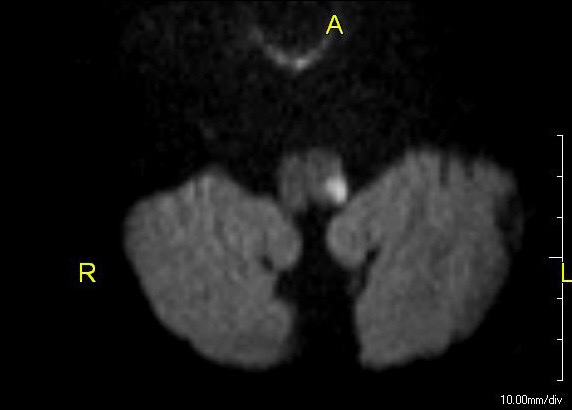
Lateral medullary syndrome: MRI showing an acute infarct in the left dorsolateral medulla
Image: “Lateral medullary syndrome” by John S. To, M.D. License: Public DomainRapid intervention and treatment are necessary to manage Wallenberg syndrome similar to the management of ischemic stroke Ischemic Stroke An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain ischemia; this condition may be due to cerebral blood vessel occlusion by thrombosis or embolism, or rarely due to systemic hypoperfusion. Ischemic Stroke. The goals are to reduce the size of the infarction and prevent medical complications.
Secondary prevention of future strokes with risk factor reduction:
Complications:
Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas depends on the size and location of the area of the stroke (extent of the medulla damaged by the occlusion of the PICA Pica Pica is an eating disorder characterized by a desire or recurrent compulsion to eat substances that are nonnutritive and not food. These compulsions and ingested substances are inappropriate for age or culture. Pica).