Heatstroke is an illness characterized as a core body temperature exceeding 40°C (104°F) with accompanying neurological symptoms including ataxia Ataxia Impairment of the ability to perform smoothly coordinated voluntary movements. This condition may affect the limbs, trunk, eyes, pharynx, larynx, and other structures. Ataxia may result from impaired sensory or motor function. Sensory ataxia may result from posterior column injury or peripheral nerve diseases. Motor ataxia may be associated with cerebellar diseases; cerebral cortex diseases; thalamic diseases; basal ganglia diseases; injury to the red nucleus; and other conditions. Ataxia-telangiectasia, seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures, and/or delirium Delirium Delirium is a medical condition characterized by acute disturbances in attention and awareness. Symptoms may fluctuate during the course of a day and involve memory deficits and disorientation. Delirium. Heatstroke is usually due to the body’s inability to regulate its temperature when challenged with an elevated heat Heat Inflammation load. The illness can be classified as exertional or non-exertional. Management involves emergent stabilization, cooling, and supportive care. Early recognition and intervention are important to prevent complications or organ failure.
Last updated: Apr 27, 2025
Heatstroke is a temperature-related illness caused by the body’s failure to maintain temperature homeostasis Homeostasis The processes whereby the internal environment of an organism tends to remain balanced and stable. Cell Injury and Death. Heatstroke is characterized by body temperatures approaching and exceeding 40ºC (104ºF) and neurological symptoms including seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures, delirium Delirium Delirium is a medical condition characterized by acute disturbances in attention and awareness. Symptoms may fluctuate during the course of a day and involve memory deficits and disorientation. Delirium, and ataxia Ataxia Impairment of the ability to perform smoothly coordinated voluntary movements. This condition may affect the limbs, trunk, eyes, pharynx, larynx, and other structures. Ataxia may result from impaired sensory or motor function. Sensory ataxia may result from posterior column injury or peripheral nerve diseases. Motor ataxia may be associated with cerebellar diseases; cerebral cortex diseases; thalamic diseases; basal ganglia diseases; injury to the red nucleus; and other conditions. Ataxia-telangiectasia.
Incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency in the United States is difficult to determine due to lack of reporting:
Risk factors for heatstroke:
Heatstroke can be divided based on its etiology as classic or exertional.
| Classic heatstroke | Exertional heatstroke | |
|---|---|---|
| Age | Elderly | Young |
| Health status | Debilitated with chronic medical conditions | Healthy |
| Predisposing factors | Medications, poor housing | Athletic competition, training |
| Occurrence | During heatwaves | Sporadic Sporadic Selective IgA Deficiency |
| Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions | Anhidrosis | Diaphoresis |
| Glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance | Normal | Low |
| Lactic acidosis Lactic Acidosis Oxazolidinones | Absent | Often severe |
| Coagulopathy | Mild | Severe, DIC DIC Disseminated intravascular coagulation (DIC) is a condition characterized by systemic bodywide activation of the coagulation cascade. This cascade results in both widespread microvascular thrombi contributing to multiple organ dysfunction and consumption of clotting factors and platelets, leading to hemorrhage. Disseminated Intravascular Coagulation |
| Renal | Oliguria Oliguria Decreased urine output that is below the normal range. Oliguria can be defined as urine output of less than or equal to 0. 5 or 1 ml/kg/hr depending on the age. Renal Potassium Regulation | Acute kidney injury Acute Kidney Injury Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury |
| Rhabdomyolysis Rhabdomyolysis Rhabdomyolysis is characterized by muscle necrosis and the release of toxic intracellular contents, especially myoglobin, into the circulation. Rhabdomyolysis | Absent or mild | Often severe |
Under normal conditions, the body can thermoregulate extremely efficiently (undergoing a 1°C (1.8°F) change in core temperature for every 25–30°C (45–54°F) change in environmental temperature). Heatstroke is the product of a failure to thermoregulate.
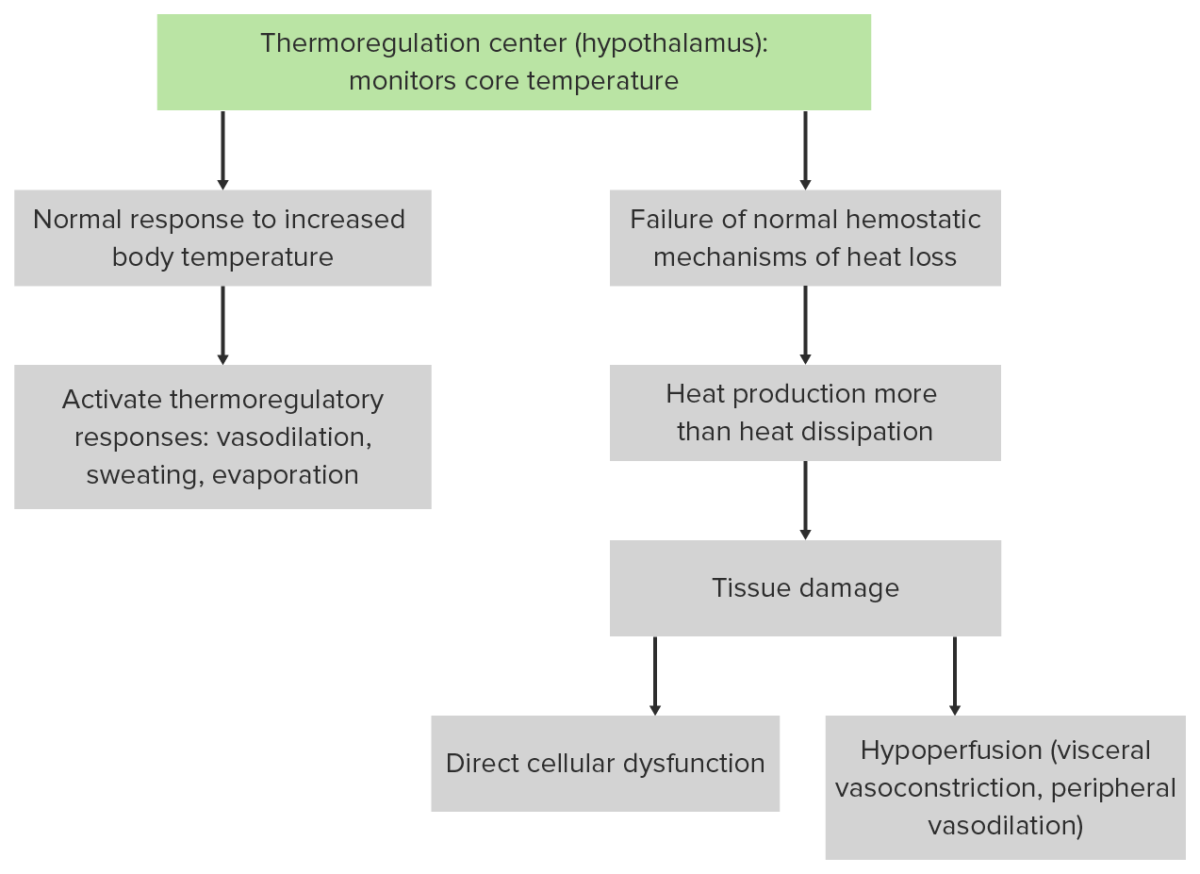
Pathophysiology of heatstroke
Image by Lecturio.Lab testing is for monitoring of progression of symptoms and cure.
Morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status and mortality Mortality All deaths reported in a given population. Measures of Health Status are directly related to the duration of core temperature elevation.