Hypernatremia is an elevated serum sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia concentration > 145 mmol/L. Serum sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia is the greatest contributor to plasma osmolality Plasma osmolality Volume Depletion and Dehydration, which is very tightly controlled by the hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus via the thirst mechanism and antidiuretic hormone (ADH) release. Hypernatremia occurs either from a lack of access to water or an excessive intake of sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia. The total volume of water lost (usually via GI or renal routes) is regained through normal oral intake. Therefore, if a patient has access to water and an intact thirst mechanism, many etiologies of hypernatremia may remain hidden. The etiology of hypernatremia is often easily determined by clinical history. Treatment is primarily a replacement of the free water deficit by IV or oral routes.
Last updated: Jun 21, 2025
Water regulation Water Regulation Renal Na+ and water regulation work in tandem to control how fluid is distributed throughout the compartments of the body. Sodium is the body’s dominant extracellular solute, and is responsible for the osmotic force that keeps differing amounts of water in each compartment. Changes in Na+ balance are sensed by the body through changes in blood volume. Renal Sodium and Water Regulation is controlled by the interplay between the osmoreceptors Osmoreceptors Renal Sodium and Water Regulation in the hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus and the response to antidiuretic hormone (ADH) in the kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy, resulting in very tight control of serum sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia and plasma osmolality Plasma osmolality Volume Depletion and Dehydration.
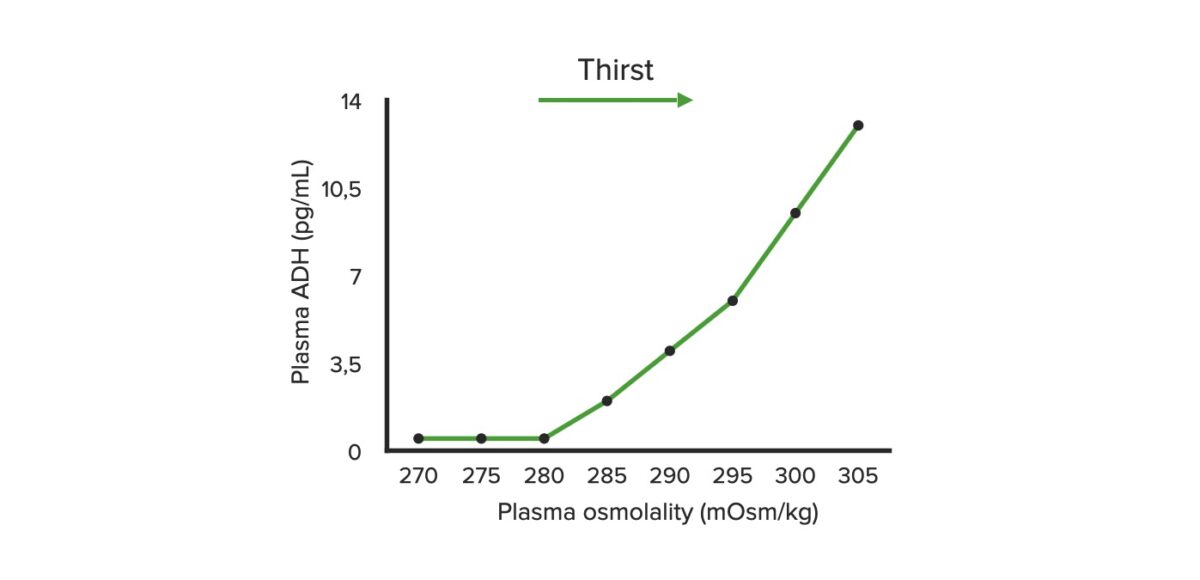
Plasma osmolality and antidiuretic hormone (ADH): graph illustrating the relationship between the plasma osmolality of ADH release
Image by Lecturio.Etiologies of hypernatremia are organized according to volume status Volume Status ACES and RUSH: Resuscitation Ultrasound Protocols.
The primary clinical finding in hypernatremia is thirst. If the patient is unable to ingest enough water to keep their serum sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia from rising significantly, dehydration Dehydration The condition that results from excessive loss of water from a living organism. Volume Depletion and Dehydration and neurologic findings may also occur. The severity of neurologic findings depends on the acuity and magnitude of the hypernatremia.
In most cases, the etiology of hypernatremia will be clear and treatment can be initiated without any further testing. If the diagnosis is not clear, the following steps may be helpful:
Hypernatremia is treated by replacing the free water deficit by giving a hypotonic Hypotonic Solutions that have a lesser osmotic pressure than a reference solution such as blood, plasma, or interstitial fluid. Renal Sodium and Water Regulation solution (i.e., 5% dextrose Dextrose Intravenous Fluids in water IV). Management is generally empirical with frequent monitoring of the serum sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia and adjustment of the fluid rate.
Volume status Volume Status ACES and RUSH: Resuscitation Ultrasound Protocols considerations:
Acute hypernatremia:
Chronic hypernatremia:
An acute rise in tonicity Tonicity Plasma tonicity refers to the concentration of only the osmotically active solutes in blood Renal Sodium and Water Regulation results in abrupt movement of fluid out of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification. A slow rise in tonicity Tonicity Plasma tonicity refers to the concentration of only the osmotically active solutes in blood Renal Sodium and Water Regulation allows the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification to adapt and minimize the effect of fluid shifts. An overly rapid correction of hypernatremia could result in abrupt movement of fluid into the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and cause cerebral edema Cerebral edema Increased intracellular or extracellular fluid in brain tissue. Cytotoxic brain edema (swelling due to increased intracellular fluid) is indicative of a disturbance in cell metabolism, and is commonly associated with hypoxic or ischemic injuries. An increase in extracellular fluid may be caused by increased brain capillary permeability (vasogenic edema), an osmotic gradient, local blockages in interstitial fluid pathways, or by obstruction of CSF flow (e.g., obstructive hydrocephalus). Increased Intracranial Pressure (ICP).