Major neurocognitive disorders (NCDs), also known as dementia, are a group of diseases characterized by decline in a person’s memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment and executive function. These disorders are progressive and persistent diseases that are the leading cause of disability Disability Determination of the degree of a physical, mental, or emotional handicap. The diagnosis is applied to legal qualification for benefits and income under disability insurance and to eligibility for social security and workman's compensation benefits. ABCDE Assessment among elderly people worldwide. There are several distinct etiologies for major NCDs. While there are known risk factors and measures to prevent major NCDs, there are no effective curative treatments.
Last updated: Dec 3, 2024
Most common:
Less common:
Pathophysiology of the most common causes of the major NCDs are shortly described below.
Alzheimer disease:
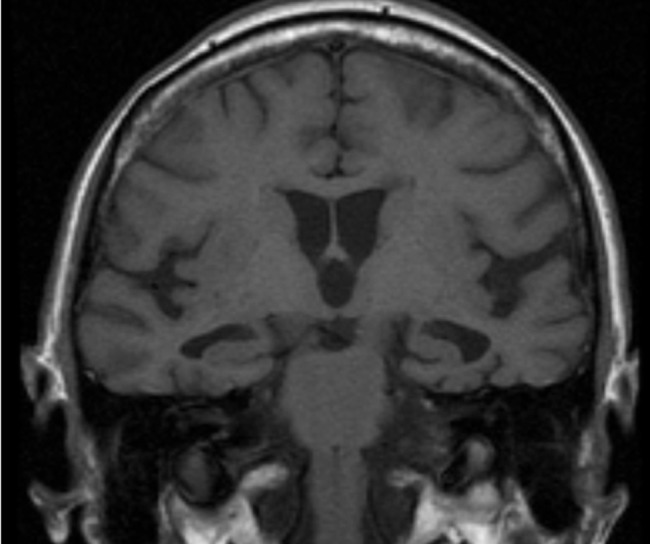
T1-weighted MRI image showing bilateral hippocampal atrophy typical for Alzheimer disease
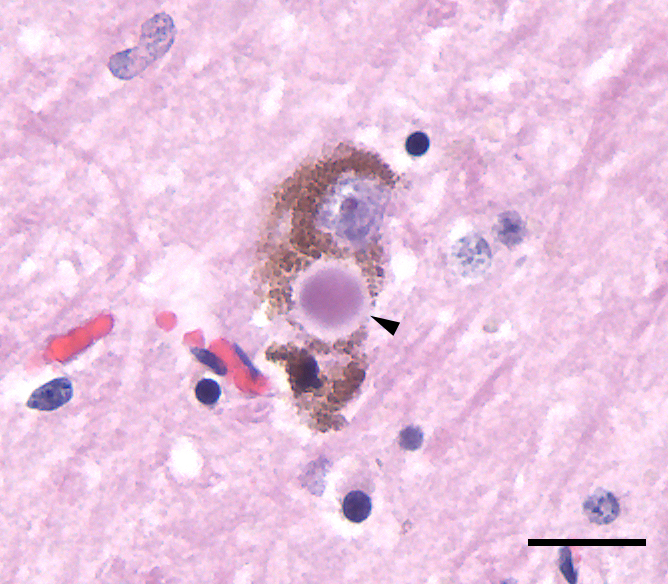
Photomicrograph of a Lewy body (arrowhead) in the cytoplasm of a neuron in the substantia nigra from a person with Parkinson’s disease:
The tissue section was stained with hematoxylin and eosin (purple and pink, respectively). The brown material is neuromelanin, which occurs naturally in neurons of the human substantia nigra.
Significant decline in cognition in the following domains:
Symptoms are not explained by other medical, psychiatric conditions (depression, delirium Delirium Delirium is a medical condition characterized by acute disturbances in attention and awareness. Symptoms may fluctuate during the course of a day and involve memory deficits and disorientation. Delirium).
| Feature | Alzheimer disease Alzheimer disease As the most common cause of dementia, Alzheimer disease affects not only many individuals but also their families. Alzheimer disease is a progressive neurodegenerative disease that causes brain atrophy and presents with a decline in memory, cognition, and social skills. Alzheimer Disease | Vascular dementia | Frontotemporal dementia Frontotemporal dementia Heterogeneous group of neurodegenerative disorders characterized by frontal and temporal lobe atrophy associated with neuronal loss, gliosis, and dementia. Patients exhibit progressive changes in social, behavioral, and/or language function. Multiple subtypes or forms are recognized based on presence or absence of tau protein inclusions. Ftld includes three clinical syndromes: frontotemporal dementia, semantic dementia, and primary progressive nonfluent aphasia. Amyotrophic Lateral Sclerosis | Dementia with Lewy bodies Lewy bodies Intracytoplasmic, eosinophilic, round to elongated inclusions found in vacuoles of injured or fragmented neurons. The presence of lewy bodies is the histological marker of the degenerative changes in lewy body disease and parkinson disease but they may be seen in other neurological conditions. They are typically found in the substantia nigra and locus coeruleus but they are also seen in the basal forebrain, hypothalamic nuclei, and neocortex. Parkinson’s Disease |
|---|---|---|---|---|
| Onset of Symptoms | Insidious | Stepwise progression | Pre-senile onset | Insidious |
| Cognitive symptoms | Decline in memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment and executive function | Decline in executive function | Decline in executive function |
|
| Motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology symptoms | Dyspraxia, apraxia Apraxia A group of cognitive disorders characterized by the inability to perform previously learned skills that cannot be attributed to deficits of motor or sensory function. The two major subtypes of this condition are ideomotor and ideational apraxia, which refers to loss of the ability to mentally formulate the processes involved with performing an action. For example, dressing apraxia may result from an inability to mentally formulate the act of placing clothes on the body. Apraxias are generally associated with lesions of the dominant parietal lobe and supramarginal gyrus. Cranial Nerve Palsies, and myoclonus Myoclonus Involuntary shock-like contractions, irregular in rhythm and amplitude, followed by relaxation, of a muscle or a group of muscles. This condition may be a feature of some central nervous system diseases; (e.g., epilepsy-myoclonic). Nocturnal myoclonus is the principal feature of the nocturnal myoclonus syndrome. Neurological Examination in later stages | Depending on location of lesion | Parkinsonian symptoms in certain cases | Parkinsonian symptoms follow cognitive symptoms |
| Screening Screening Preoperative Care test | Mini-Cog | MMSE | MoCA |
|---|---|---|---|
| Time to administer test | < 5 minutes | 6–10 minutes | About 10 minutes |
| Number of questions | 2 | 20 | 18 |
| Cognitive dimensions tested |
|
|
|
The following are mostly used to differentiate or rule out treatable medical or neurologic conditions that cause a decline in cognition: