As the most common cause of dementia Dementia Major neurocognitive disorders (NCD), also known as dementia, are a group of diseases characterized by decline in a person's memory and executive function. These disorders are progressive and persistent diseases that are the leading cause of disability among elderly people worldwide. Major Neurocognitive Disorders, Alzheimer disease affects not only many individuals but also their families. Alzheimer disease is a progressive neurodegenerative disease that causes brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification atrophy Atrophy Decrease in the size of a cell, tissue, organ, or multiple organs, associated with a variety of pathological conditions such as abnormal cellular changes, ischemia, malnutrition, or hormonal changes. Cellular Adaptation and presents with a decline in memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment, cognition, and social skills. Several genetic defects and risk factors have been described, although there is no clear cause in the majority of cases. The main pathologic features are neuritic plaques, extracellular deposits of amyloid peptides, and neurofibrillary tangles. The clinical features are memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment impairment, loss of executive function and judgment Judgment The process of discovering or asserting an objective or intrinsic relation between two objects or concepts; a faculty or power that enables a person to make judgments; the process of bringing to light and asserting the implicit meaning of a concept; a critical evaluation of a person or situation. Psychiatric Assessment, impaired cognitive function, and behavioral changes. Diagnosis is based on clinical examination, neuropsychiatric testing, and imaging. There is no curative therapy, but symptomatic management with medications may slow progression; these include cholinesterase Cholinesterase Liver Function Tests inhibitors, the N-methyl-D-aspartate (NMDA) receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors antagonist memantine, and a recently approved anti-amyloid monoclonal antibody.
Last updated: May 17, 2024
Alzheimer disease is a progressive neurodegenerative disease that causes brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification atrophy Atrophy Decrease in the size of a cell, tissue, organ, or multiple organs, associated with a variety of pathological conditions such as abnormal cellular changes, ischemia, malnutrition, or hormonal changes. Cellular Adaptation and a decline in cognition, memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment, and social skills.
Although the cause of Alzheimer disease is unknown, several genetic defects and risk factors have been identified.
The pathogenesis of Alzheimer disease is unclear; however, there is an increase in beta-amyloid peptides and aggregation Aggregation The attachment of platelets to one another. This clumping together can be induced by a number of agents (e.g., thrombin; collagen) and is part of the mechanism leading to the formation of a thrombus. Coagulation Studies of the tau protein.
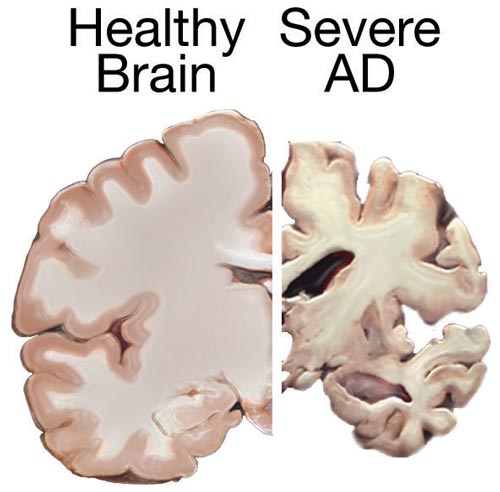
Depiction of the gross pathology seen with Alzheimer disease
Image: “Alzheimers brain” by National Institutes of Health. License: Public Domain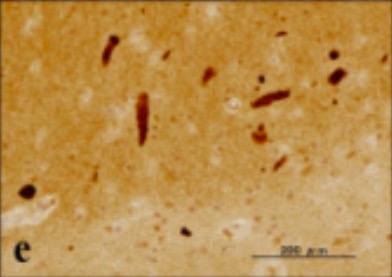
Silver stain showing a neurofibrillary tangle within neuronal cytoplasm
Image: “UBQLN1 single labeling” by Department of Bioinformatics and Molecular Neuropathology, Meiji Pharmaceutical University, 2-522-1 Noshio, Kiyose, Tokyo 204-8588, Japan. License: CC BY 2.0, cropped by Lecturio.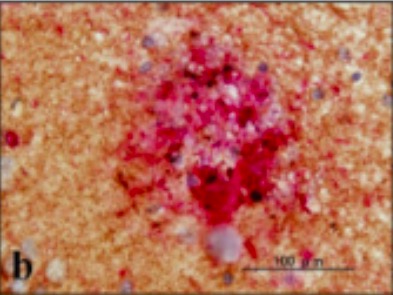
Neuritic plaque with a rim of dystrophic neurites surrounding an amyloid core
Image: “UBQLN1 single labeling” by Department of Bioinformatics and Molecular Neuropathology, Meiji Pharmaceutical University, 2-522-1 Noshio, Kiyose, Tokyo 204-8588, Japan. License: CC BY 2.0, cropped by Lecturio.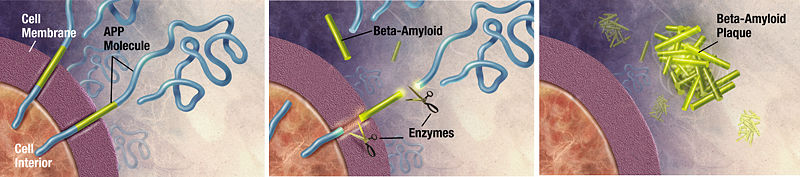
Formation of beta-amyloid plaques:
APP: beta-amyloid precursor protein
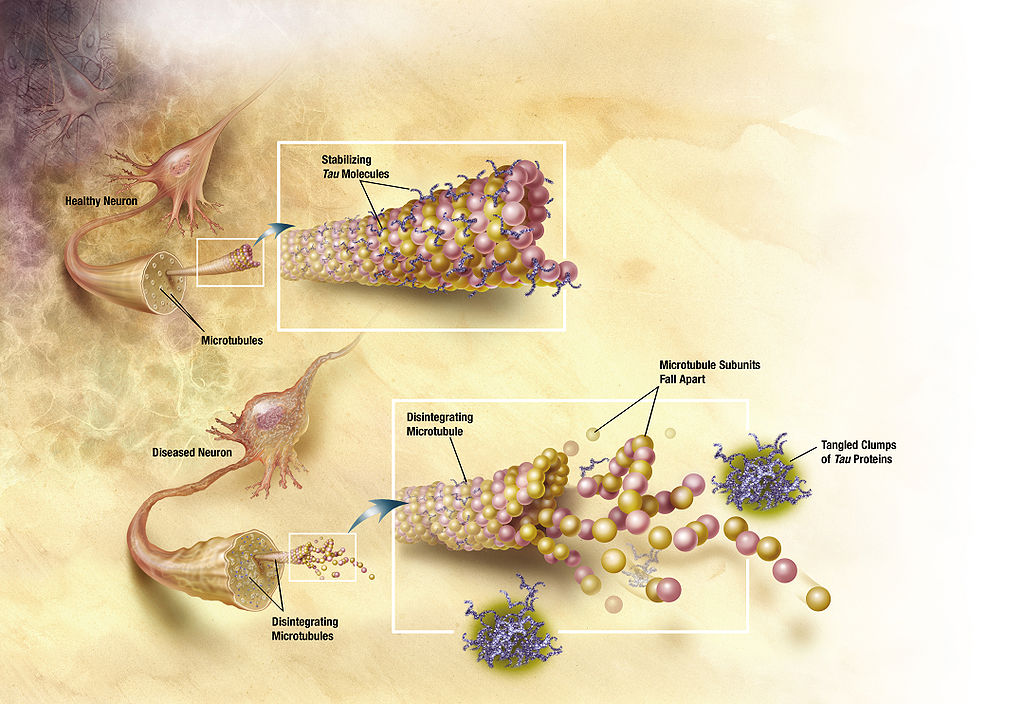
Neurofibrillary tangles as seen in Alzheimer disease
Image: “Diagram of how microtubules desintegrate with Alzheimer’s disease” by ADEAR. License: Public DomainInterviewing family members is essential to obtain a history of cognitive and behavioral changes.
Memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment impairment is the most common early symptom of Alzheimer disease.
The typical duration of symptomatic Alzheimer disease is 8–10 years, but the course ranges from 1 to 25 years.
Alzheimer disease:
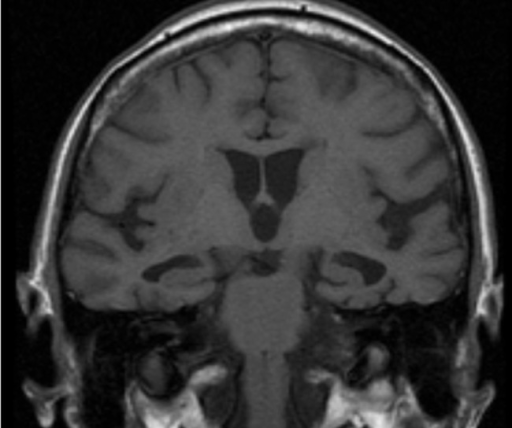
T1-weighted MRI showing bilateral hippocampal atrophy typical of Alzheimer disease
There is no cure for Alzheimer disease, but medications may delay functional decline. Individualized treatment decisions are made in conjunction with individuals and caregivers after discussion of potential benefits, risks, and costs.