The identification Identification Defense Mechanisms and classification of a patient's skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions are important steps in the diagnosis of any skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions disorder. Primary lesions represent the initial presentation of the disease process. Secondary lesions develop from irritated or manipulated primary lesions and/or manifestations of disease progression. The key features of skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions include type, morphology, color, shape, arrangement, and distribution. A comprehensive examination of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, appendages, and mucous membranes is done, with the type of procedure performed depending on the suspected diagnosis.
Last updated: Feb 17, 2023
Scales are dry or greasy masses of keratin Keratin A class of fibrous proteins or scleroproteins that represents the principal constituent of epidermis; hair; nails; horny tissues, and the organic matrix of tooth enamel. Two major conformational groups have been characterized, alpha-keratin, whose peptide backbone forms a coiled-coil alpha helical structure consisting of type I keratin and a type II keratin, and beta-keratin, whose backbone forms a zigzag or pleated sheet structure. Alpha-keratins have been classified into at least 20 subtypes. In addition multiple isoforms of subtypes have been found which may be due to gene duplication. Seborrheic Keratosis that represent thickened stratum corneum Stratum corneum Skin: Structure and Functions.
Characteristic types of scales are:

Thickened, “lizard skin” appearance of ichthyosis vulgaris
Image: “In vivo confocal microscopy of pre-Descemet corneal dystrophy associated with X-linked ichthyosis: a case report” by BMC Ophthalmology. License: CC BY 4.0
Crusted, nonbullous impetigo on the upper extremity of a pediatric patient
Image: “Diagnosis of Atopic Dermatitis: Mimics, Overlaps, and Complications” by Siegfried EC, Hebert AA. License: CC BY 4.0
Punched-out erosions with cutaneous herpes simplex virus infection
Image: “Disseminated cutaneous Herpes Simplex Virus-1 in a woman with rheumatoid arthritis receiving infliximab: a case report” by Justice EA, Khan SY, Logan S, Jobanputra P. License: CC BY 2.0Excoriation Excoriation Mastitis is a linear abrasion Abrasion Soft Tissue Abscess produced by mechanical means (scratching, rubbing, or picking) that usually involves only the epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions but can reach the papillary dermis Dermis A layer of vascularized connective tissue underneath the epidermis. The surface of the dermis contains innervated papillae. Embedded in or beneath the dermis are sweat glands; hair follicles; and sebaceous glands. Skin: Structure and Functions.

Excoriation disorder secondary to skin picking
Image: “Derma me” by Boogafreak/Vatadoshu. License: Public Domain
Ulcer from chronic venous stasis
Image: “Interaction between a regenerative matrix and wound bed in nonhealing ulcers: results with 16 cases” by Motolese A, Vignati F, Brambilla R, Cerati M, Passi A. License: CC BY 3.0
Hand eczema with fissure
Image: “Occupational protein contact dermatitis: two case reports” by Rocha J, Pereira T, Sousa-Basto A, Brito C. License: CC BY 3.0
Skin rash and atrophy on an individual’s trunk associated with dermatomyositis
Image: “Fig6: Typical skin rash, with atrophic areas on the trunk” by Leonardo Pires Novais Dias et al. License: CC BY 4.0
Lichenification of the wrist in atopic dermatitis
Image by Jeremy Greer, MD (Lecturio).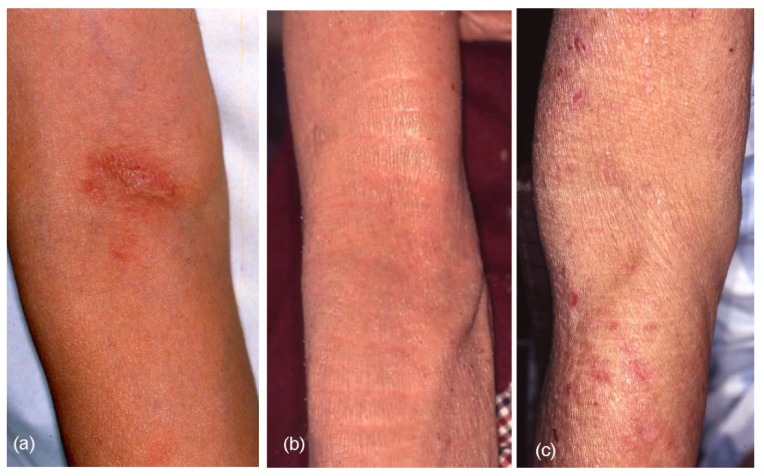
Lichenification (lichenified eczema) in the antecubital areas of elderly patients with atopic eczema.
(a): Localized lichenified eczema in the elbow fold
(b): Diffuse lichenified eczema in the elbow fold and flexure site of the arm
(c): Lichenified eczema around the scarcely involved elbow fold (reverse sign)
A general physical examination as well as a focused dermatologic examination Dermatologic examination Examination of the skin is a fundamental part of the standard physical exam. This exam consists of a thorough inspection of the skin of the entire body. The assessment focuses on identifying abnormal signs on the skin, such as the scalp, orifices, nails, and mucosal surfaces. Dermatologic Examination should be performed:
Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions features and commonly associated skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions conditions and/or lesions to consider:
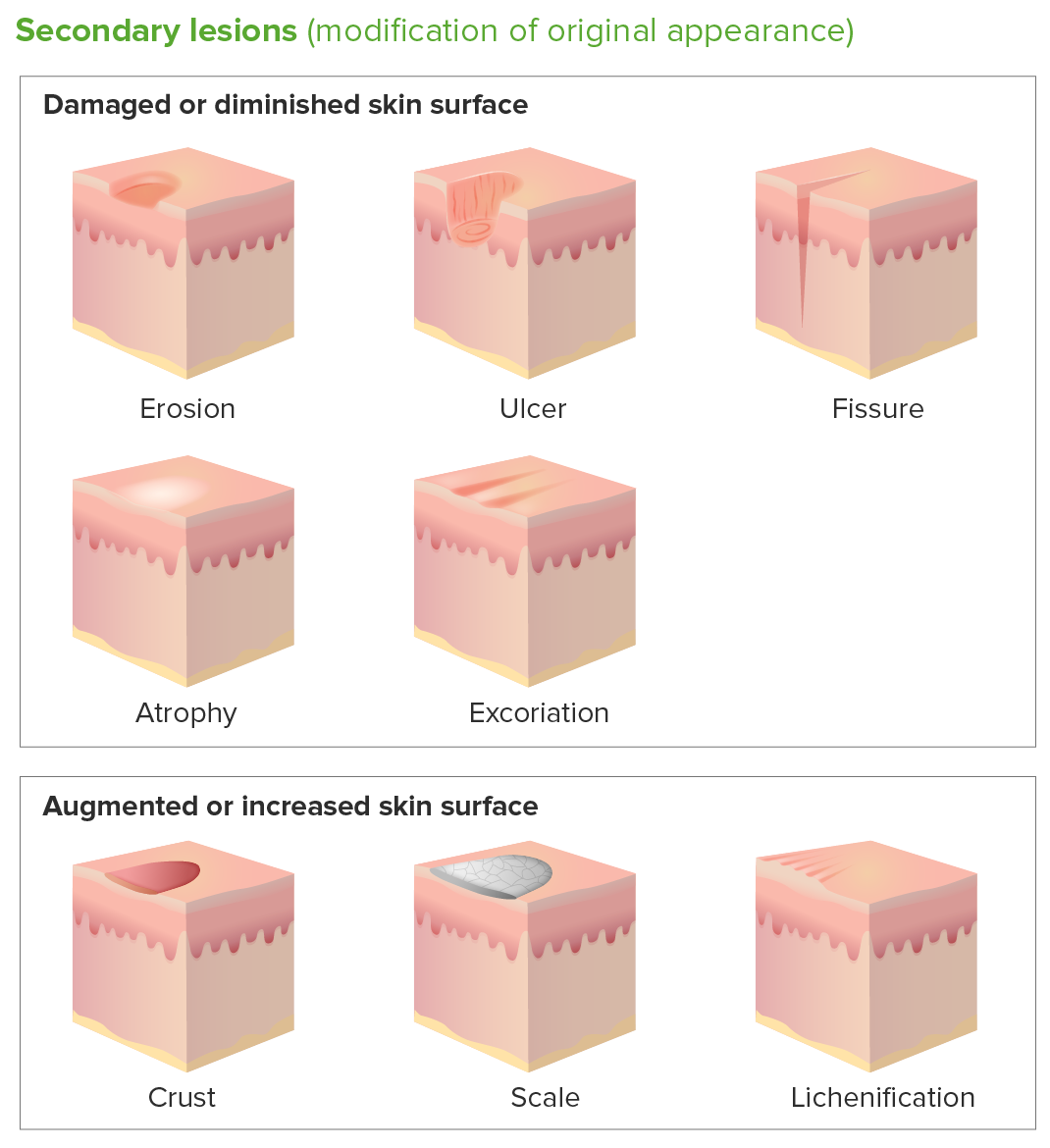
Secondary skin lesions:
Erosion: discontinuity of the skin with incomplete loss of the epidermis without penetration below the dermal–epidermal junction
Ulcer: complete loss of the epidermis and portions of the dermis and subcutaneous fat resulting in a scar
Fissure: narrow linear crack/split in the skin, extending through the epidermis into the dermis
Atrophy: loss of tissue that can be epidermal, dermal, or subcutaneous with appearance of thin, translucent, and/or wrinkled skin surface
Excoriation: linear abrasion produced by mechanical means (scratching, rubbing, or picking)
Crust: dried exudate of body fluids (blood, pus, or sebum) on an area of damaged skin
Scale: dry or greasy masses of keratin representing thickened stratum corneum
Lichenification: thickening and hyperpigmentation of the skin resulting from repeated rubbing