An anal fissure Fissure A crack or split that extends into the dermis Generalized and Localized Rashes is a painful superficial tear of the epithelial lining (anoderm) of the anal canal. Anal fissures Anal fissures A painful linear tear at the margin of the anus. It appears as a crack or slit in the mucous membrane of the anus and is very painful and difficult to heal. Constipation most often occur secondary to local trauma or irritation from constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation, diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea, anal intercourse Anal intercourse Hemorrhoids, or perineal lacerations during childbirth. Treatment is generally conservative, including stool softeners, bulking agents, sitz baths, and/or topical vasodilators Vasodilators Drugs used to cause dilation of the blood vessels. Thromboangiitis Obliterans (Buerger Disease).
Last updated: May 6, 2025
The “Ds” of anal fissures Anal fissures A painful linear tear at the margin of the anus. It appears as a crack or slit in the mucous membrane of the anus and is very painful and difficult to heal. Constipation:
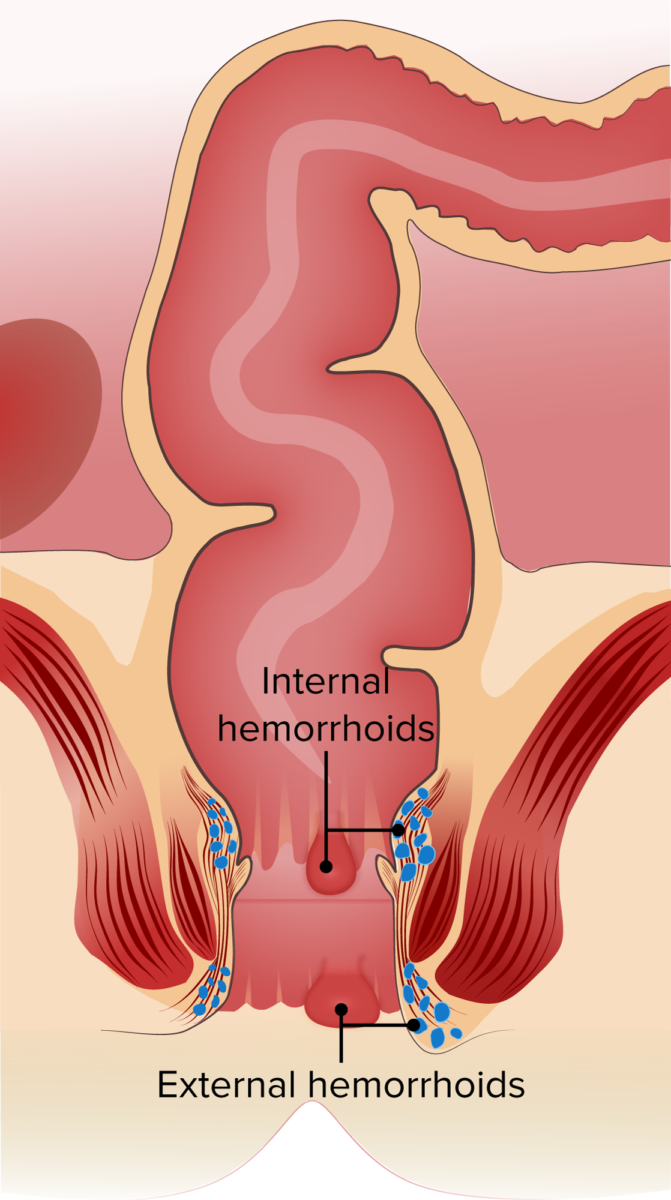
Internal and external hemorrhoids
Image by Lecturio.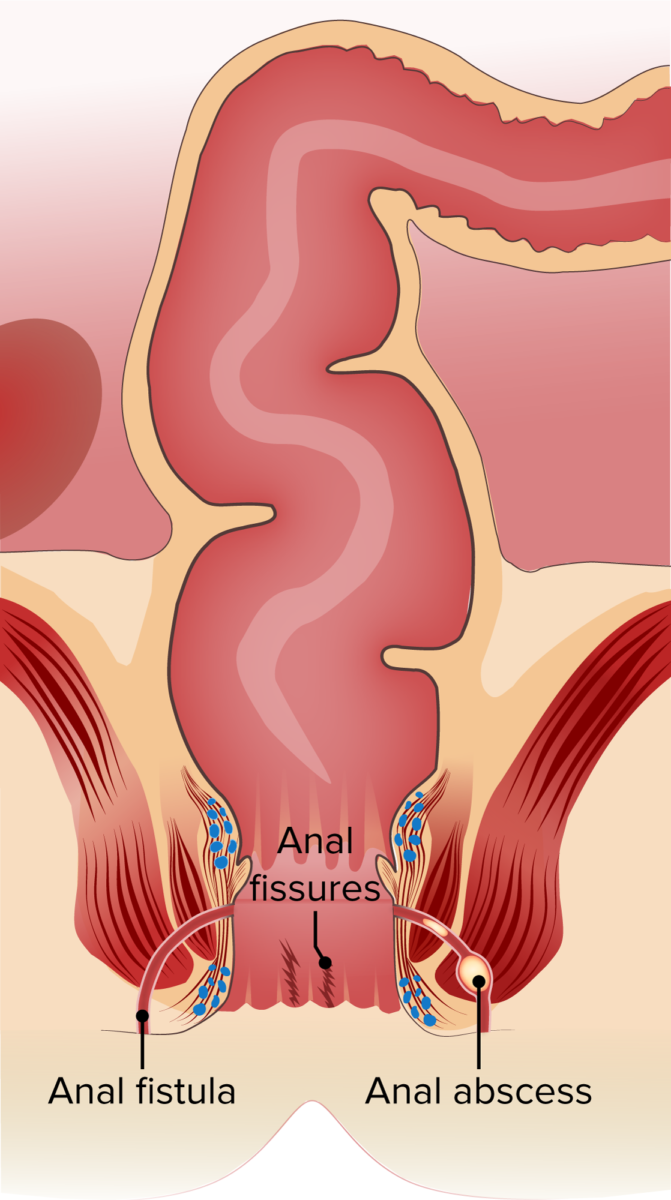
Anal disorders: fistula, fissures and abscess
Image by Lecturio.
Chronic anal fissure and marisca (large kind of haemorrhoid)
Image: “Chronic anal fissure and marisca” by Department of Dermatology and Allergology, Hospital Dresden-Friedrichstadt, Academic Teaching Hospital of the University of Dresden, Friedrichstrasse 41, Dresden, Germany. License: CC BY 2.0