Corneal abrasions, erosions, and ulcers are classified as corneal epithelial defects. These defects are differentiated according to their depth: abrasions are into the corneal surface epithelium Surface epithelium Epithelium is classified according to the cells (squamous, cuboidal, columnar), the number of layers, and other unique characteristics either due to function (transitional epithelium allowing distention) or appearance (pseudostratified epithelium giving a false impression of multiple layers). Surface epithelium has multiple functions, which include protection, secretion, filtration, and sensory reception. Surface Epithelium: Histology, erosions involve the corneal epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology and epithelial basement membrane Basement membrane A darkly stained mat-like extracellular matrix (ecm) that separates cell layers, such as epithelium from endothelium or a layer of connective tissue. The ecm layer that supports an overlying epithelium or endothelium is called basal lamina. Basement membrane (bm) can be formed by the fusion of either two adjacent basal laminae or a basal lamina with an adjacent reticular lamina of connective tissue. Bm, composed mainly of type IV collagen; glycoprotein laminin; and proteoglycan, provides barriers as well as channels between interacting cell layers. Thin Basement Membrane Nephropathy (TBMN), and ulcers extend into the underlying stroma. Corneal defects are commonly caused by injury to the eye by foreign bodies, spontaneous causes such as corneal epithelial dystrophy, or infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. These injuries are diagnosed with proper history taking and physical examination. Slit-lamp examination Slit-Lamp Examination Blepharitis is used for confirmation. Treatment includes use of topical lubricants, analgesics, antibiotics, and an eye patch Patch Nonpalpable lesion > 1 cm in diameter Generalized and Localized Rashes. Minor surgical procedures are used in treating erosions. Complications include infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, loss of vision Vision Ophthalmic Exam, perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis, and irregular astigmatism Astigmatism Unequal curvature of the refractive surfaces of the eye. Thus a point source of light cannot be brought to a point focus on the retina but is spread over a more or less diffuse area. This results from the radius of curvature in one plane being longer or shorter than the radius at right angles to it. . Refractive Errors.
Last updated: Jul 16, 2025
The cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy is a transparent, avascular part of the eye that covers the iris, anterior chamber Anterior chamber The space in the eye, filled with aqueous humor, bounded anteriorly by the cornea and a small portion of the sclera and posteriorly by a small portion of the ciliary body, the iris, and that part of the crystalline lens which presents through the pupil. Eye: Anatomy, and pupil Pupil The pupil is the space within the eye that permits light to project onto the retina. Anatomically located in front of the lens, the pupil’s size is controlled by the surrounding iris. The pupil provides insight into the function of the central and autonomic nervous systems. Pupil: Physiology and Abnormalities. The corneal layers include:
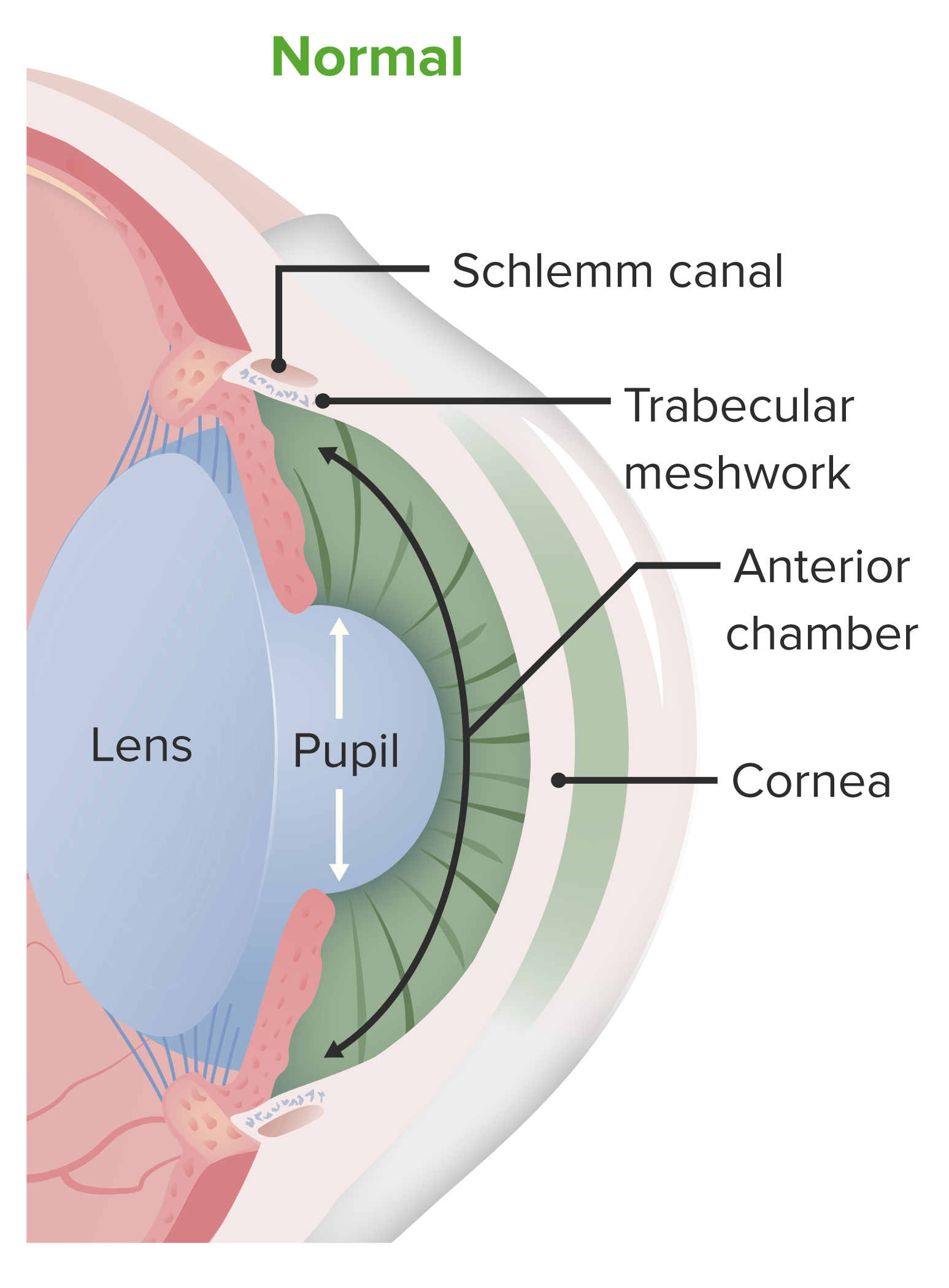
Anatomy of the anterior chamber of the eye:
The cornea is part of the fibrous layer of the eye, and overlies the anterior chamber. It is a protective structure and contributes to the initial refraction of light entering the eye.
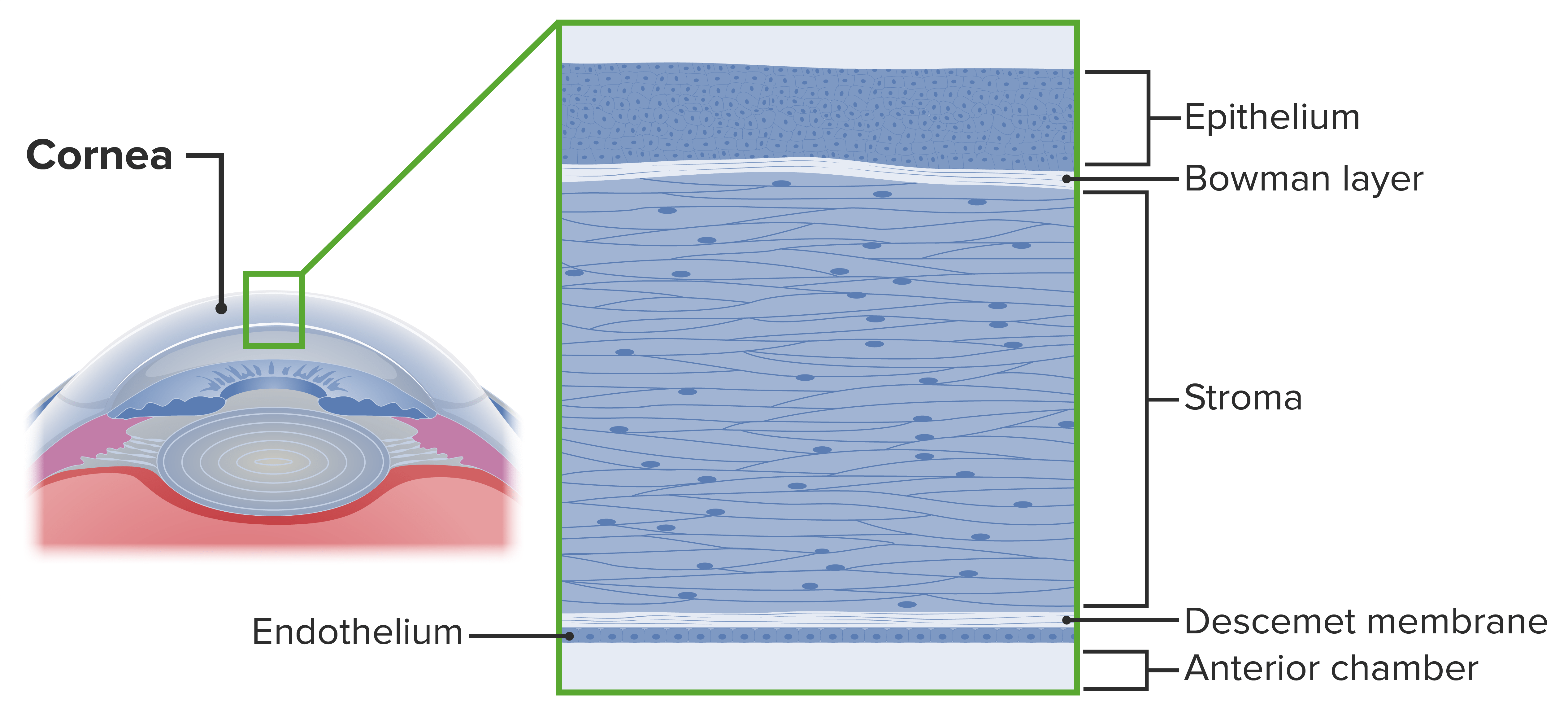
Layers of the cornea
Image by Lecturio.Corneal epithelial defects are conditions that disturb the structural integrity of the cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy. Corneal abrasions, erosions, and ulcers are defects in the corneal epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology and are classified by the depth of involvement of corneal layers:
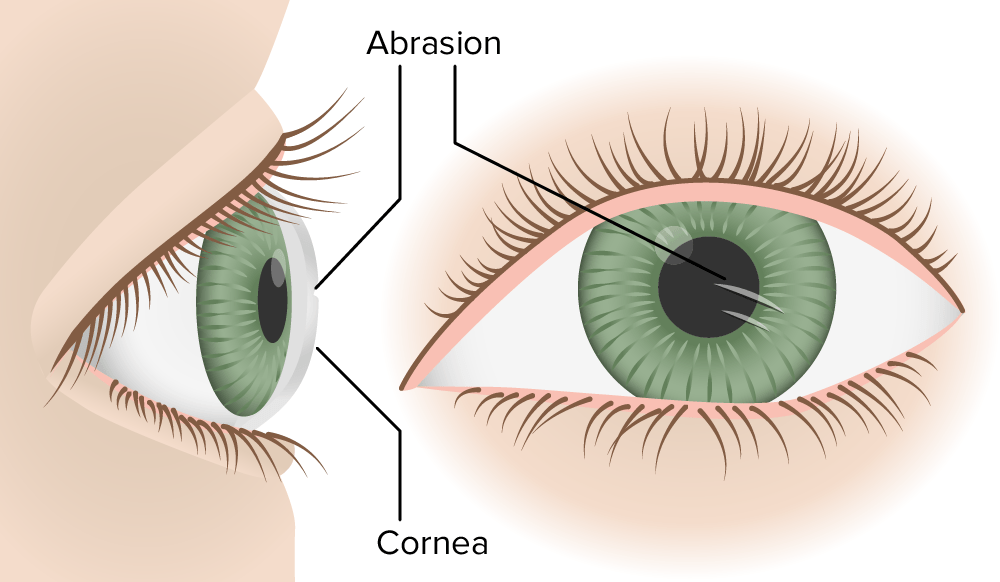
Corneal abrasion
Image by Lecturio.Corneal abrasions:
Corneal erosions:
Corneal ulcers:
Risk factors for corneal ulcers include:
Corneal abrasions and erosions:
Corneal ulcers:
Individuals usually have a history of trauma to the globe, either by foreign body Foreign Body Foreign Body Aspiration or finger.
In addition to the above signs and symptoms:

A case of corneal ulcer
Image: “Corneal ulcer” by Pearson A. License: CC BY 4.0
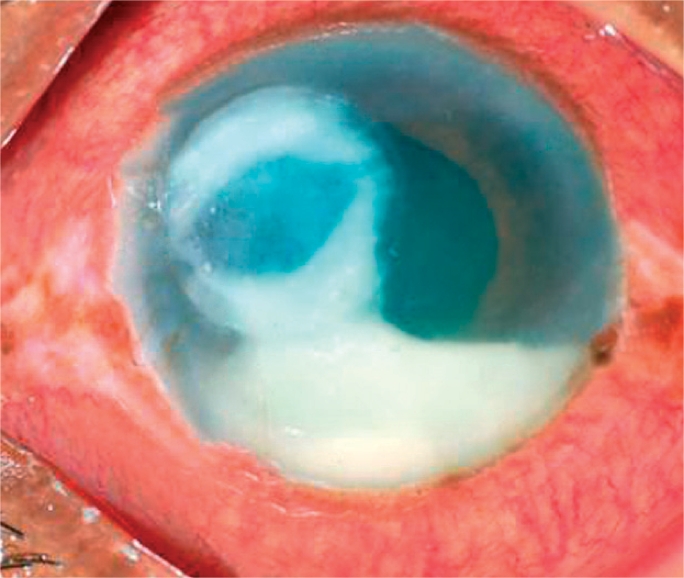
Severe case of suppurative corneal ulcer
Image: “A severe bacterial ulcer caused by Pseudomonas sp.” by Srinivasan M. License: CC BY 2.0History and ophthalmic examination:
Slit-lamp examination Slit-Lamp Examination Blepharitis:
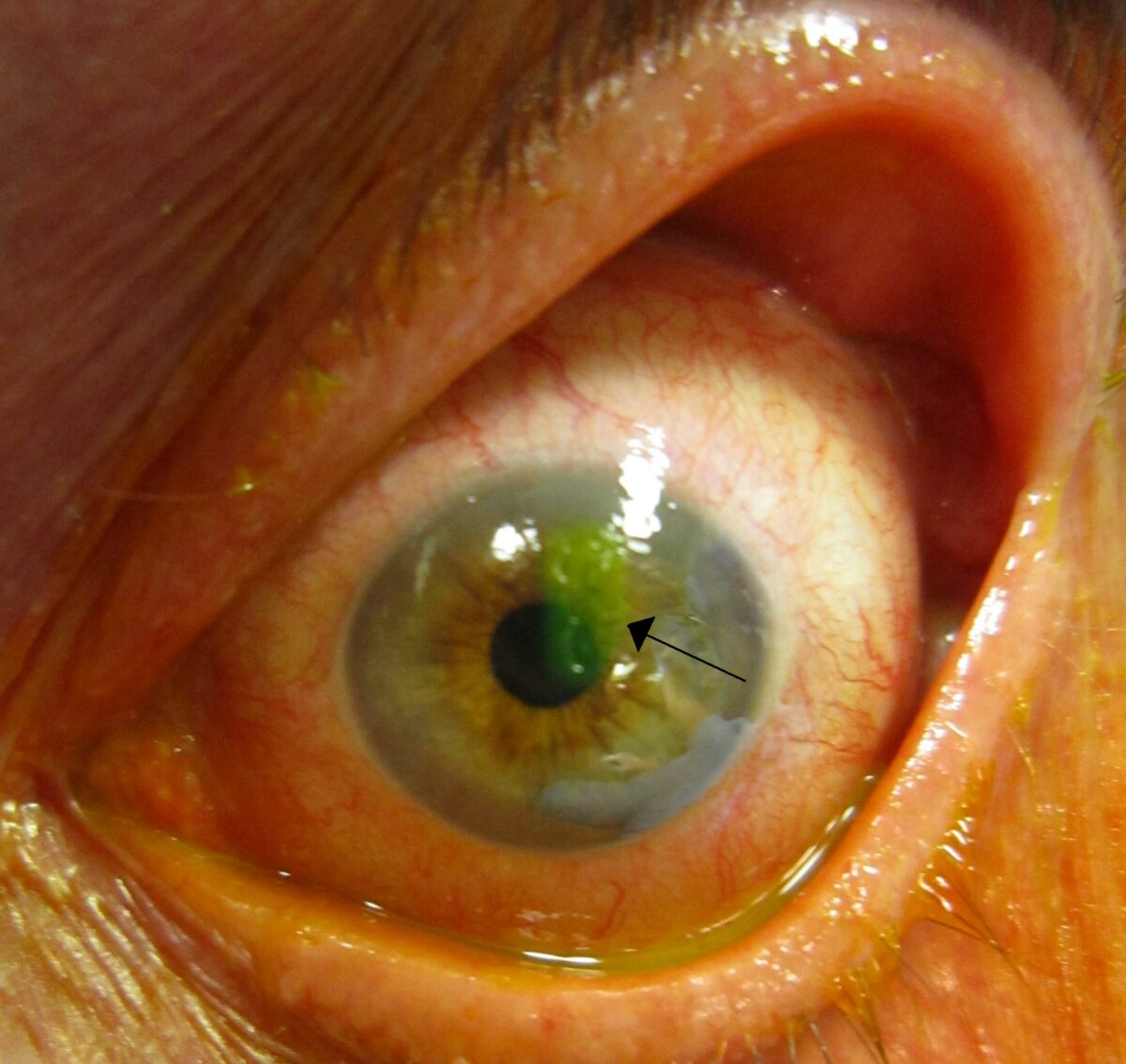
A corneal abrasion after staining with fluorescein (arrow)
Image: “A corneal abrasion after staining with florescine” by James Heilman. License: CC BY-SA 3.0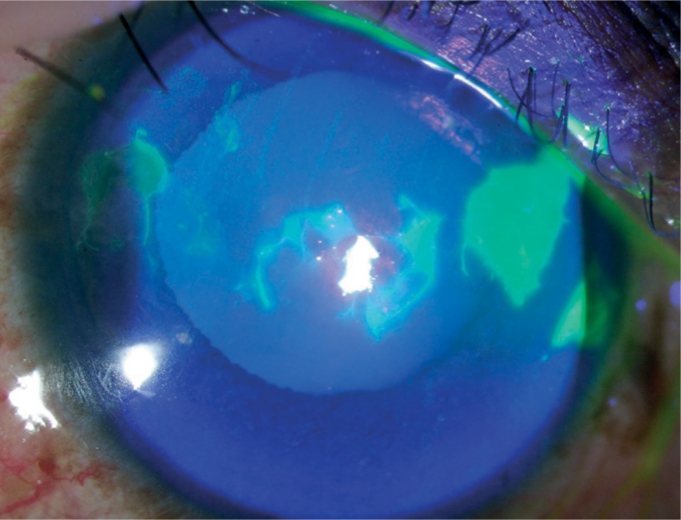
Fluorescein staining:
Brightly green stained areas represent epithelial defects.
Bacterial corneal ulcer, with hypopyon seen in anterior chamber
Image: “A bacterial ulcer. The eye is very red and inflamed. Note the ring infiltrate in the cornea and a large hypopyon in the anterior chamber” by Srinivasan M. License: CC BY 2.0