Fluoroquinolones are a group of broad-spectrum, bactericidal Bactericidal Penicillins antibiotics inhibiting bacterial DNA replication DNA replication The entire DNA of a cell is replicated during the S (synthesis) phase of the cell cycle. The principle of replication is based on complementary nucleotide base pairing: adenine forms hydrogen bonds with thymine (or uracil in RNA) and guanine forms hydrogen bonds with cytosine. DNA Replication. Fluoroquinolones cover gram-negative, anaerobic, and atypical organisms, as well as some gram-positive Gram-Positive Penicillins and multidrug-resistant (MDR) organisms. A new fluoroquinolone, delafloxacin, covers both Pseudomonas aeruginosa Pseudomonas aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas and MRSA MRSA A strain of Staphylococcus aureus that is non-susceptible to the action of methicillin. The mechanism of resistance usually involves modification of normal or the presence of acquired penicillin binding proteins. Staphylococcus. Although fluoroquinolones have a wide spectrum of activity, the use is limited secondary to a number of risks associated with the fluoroquinolone class (i.e. permanent peripheral neuropathy Neuropathy Leprosy and tendon rupture in children). Fluoroquinolones are indicated in complicated urinary, respiratory, intra-abdominal, bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types, joint, and skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. Fluoroquinolones are 2nd-line agents used to treat tuberculosis Tuberculosis Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis complex bacteria. The bacteria usually attack the lungs but can also damage other parts of the body. Approximately 30% of people around the world are infected with this pathogen, with the majority harboring a latent infection. Tuberculosis spreads through the air when a person with active pulmonary infection coughs or sneezes. Tuberculosis and 1st-line agents in a number of less common infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease (e.g., anthrax Anthrax Anthrax is an infection caused by the bacterium Bacillus anthracis, which usually targets the skin, lungs, or intestines. Anthrax is a zoonotic disease and is usually transmitted to humans from animals or through animal products. Symptoms depend on which organ system is affected. Anthrax, plague Plague The plague is a bacterial infection caused by Yersinia pestis (Y. pestis), which primarily infects rodents. The disease is transmitted to humans via a flea bite. Inhalation of infectious droplets and handling infected animals or laboratory specimens are other means of transmission. The plague has 3 forms: bubonic (most common form), septicemic, and pneumonic. Yersinia pestis/Plague, and tularemia).
Last updated: Oct 6, 2022
Fluoroquinolones are a class of broad-spectrum antibiotics. The common medications in the class include:
Fluoroquinolone structures:
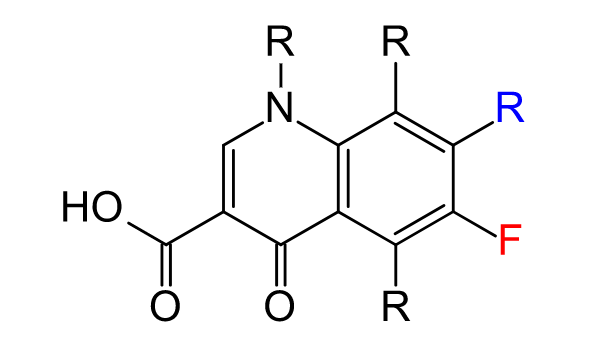
General structure of a fluoroquinolone
Image: “Sites of substitution in second-generation fluoroquinolone antibiotics” by Reubot. License: Public Domain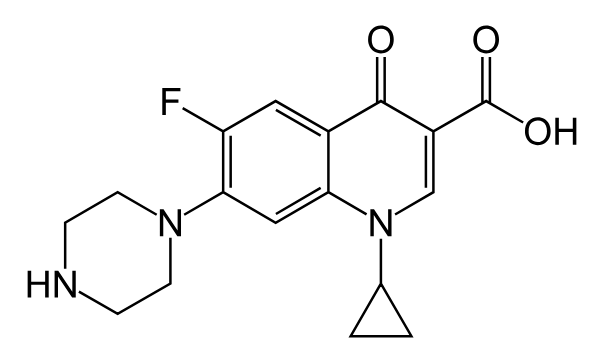
Chemical structure of ciprofloxacin
Image: “Chemical structure of ciprofloxacin” by Fvasconcellos. License: Public Domain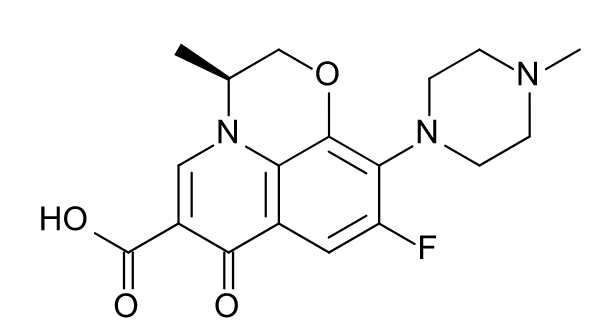
Chemical structure of levofloxacin
Image: “Chemical structure of levofloxacin” by Bryan Derksen. License: Public DomainThe dominant mechanisms of fluoroquinolone resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing:
As resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing to fluoroquinolones becomes more common, fluoroquinolone use may be limited for the following indications:
Fluoroquinolones are considered broad-spectrum antibiotics: Ciprofloxacin covers gram-negative rods the best; Levofloxacin and moxifloxacin provide excellent coverage of most potential respiratory pathogens; Delafloxacin covers both P. aeruginosa P. aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas and MRSA MRSA A strain of Staphylococcus aureus that is non-susceptible to the action of methicillin. The mechanism of resistance usually involves modification of normal or the presence of acquired penicillin binding proteins. Staphylococcus.
Atypical organisms
Anaerobic organisms
Fluoroquinolones are also considered 1st-line options against susceptible infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease caused by:
Compared to other antibiotics, fluoroquinolones are associated with a higher risk of potentially permanent and disabling adverse events. Therefore, fluoroquinolones are generally not used for uncomplicated infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease and should only be used against susceptible bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology.
Fluoroquinolones carry higher risks than many other antibiotics, which limits the use. Although adverse effects are uncommon, some may be permanent or severe.
Antibiotics can be classified in several ways. One way is to classify antibiotics by mechanism of action:
| Mechanism | Classes of antibiotics |
|---|---|
| Bacterial cell wall Cell wall The outermost layer of a cell in most plants; bacteria; fungi; and algae. The cell wall is usually a rigid structure that lies external to the cell membrane, and provides a protective barrier against physical or chemical agents. Cell Types: Eukaryotic versus Prokaryotic synthesis Synthesis Polymerase Chain Reaction (PCR) inhibitors |
|
| Bacterial protein synthesis Synthesis Polymerase Chain Reaction (PCR) inhibitors |
|
| Agents acting against DNA DNA A deoxyribonucleotide polymer that is the primary genetic material of all cells. Eukaryotic and prokaryotic organisms normally contain DNA in a double-stranded state, yet several important biological processes transiently involve single-stranded regions. DNA, which consists of a polysugar-phosphate backbone possessing projections of purines (adenine and guanine) and pyrimidines (thymine and cytosine), forms a double helix that is held together by hydrogen bonds between these purines and pyrimidines (adenine to thymine and guanine to cytosine). DNA Types and Structure and/or folate Folate Folate and vitamin B12 are 2 of the most clinically important water-soluble vitamins. Deficiencies can present with megaloblastic anemia, GI symptoms, neuropsychiatric symptoms, and adverse pregnancy complications, including neural tube defects. Folate and Vitamin B12 |
|
| Antimycobacterial agents Antimycobacterial Agents Antimycobacterial agents represent a diverse group of compounds that have activity against mycobacterial infections, including tuberculosis, leprosy and Mycobacterium avium complex (MAC) disease. The 1st-line agents for tuberculosis are rifampin, isoniazid, pyrazinamide, and ethambutol. Antimycobacterial Drugs |
|
Different antibiotics have varying degrees of activity against different bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology. The table below outlines the antibiotics with activity against 3 important classes of bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology: gram-positive Gram-Positive Penicillins cocci Cocci Bacteriology, gram-negative bacilli Bacilli Shigella, and anaerobes Anaerobes Lincosamides.
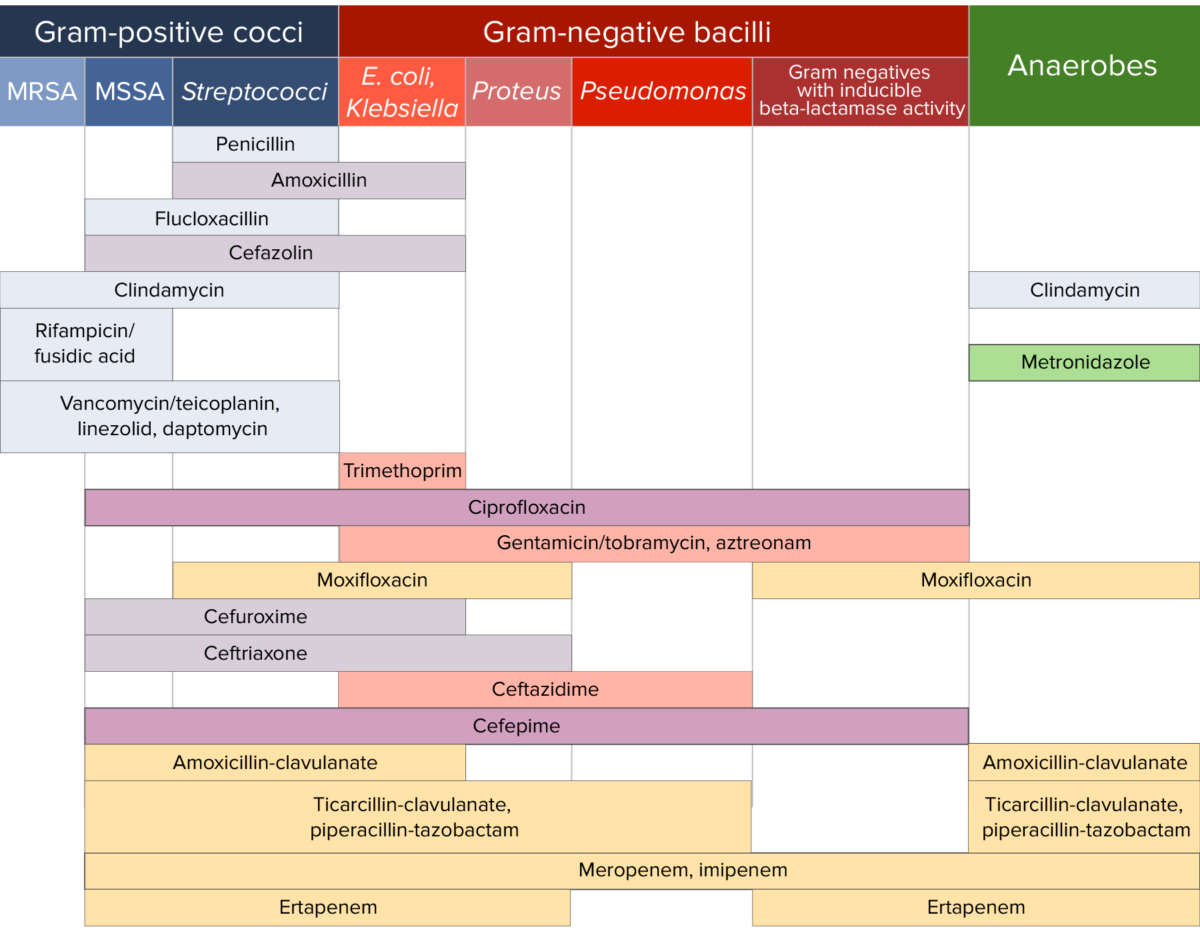
Antibiotic sensitivity:
Chart comparing the microbial coverage of different antibiotics for gram-positive cocci, gram-negative bacilli, and anaerobes.