The plague is a bacterial infection caused by Yersinia Yersinia Yersinia is a genus of bacteria characterized as gram-negative bacilli that are facultative anaerobic with bipolar staining. There are 2 enteropathogenic species that cause yersiniosis, Y. enterocolitica and Y. pseudotuberculosis. Infections are manifested as pseudoappendicitis or mesenteric lymphadenitis, and enterocolitis. Yersinia spp./Yersiniosis pestis (Y. pestis), which primarily infects rodents. The disease is transmitted to humans via a fleabite. Inhalation of infectious droplets Droplets Varicella-Zoster Virus/Chickenpox and handling infected animals Animals Unicellular or multicellular, heterotrophic organisms, that have sensation and the power of voluntary movement. Under the older five kingdom paradigm, animalia was one of the kingdoms. Under the modern three domain model, animalia represents one of the many groups in the domain eukaryota. Cell Types: Eukaryotic versus Prokaryotic or laboratory specimens are other means of transmission. The plague has 3 forms: bubonic (most common form), septicemic, and pneumonic. Bubonic plague results in swollen and tender lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 - 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy called buboes Buboes Chancroid in the inguinal area Inguinal area The external junctural region between the lower part of the abdomen and the thigh. Male Genitourinary Examination. Pneumonic and septicemic plague can arise as the primary presentation, but also can result from hematogenous Hematogenous Hepatocellular Carcinoma (HCC) and Liver Metastases spread from the bubonic disease. Diagnosis includes clinical history and findings, culture, polymerase chain reaction Polymerase chain reaction Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) ( PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR)), and serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus. The mortality Mortality All deaths reported in a given population. Measures of Health Status rate is high, so prompt diagnosis and treatment with antibiotics are necessary.
Last updated: Sep 19, 2022
Worldwide cases of the plague:
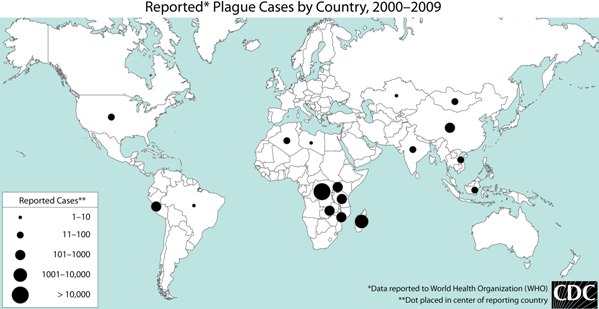
World map of plague cases reported to the World Health Organization (WHO), 2000–2009
Image: “World Plague Map – 2000 to 2009 – CDC” by the CDC. License: Public domain.Plague in the United States:

A flea infected with Y. pestis, shown as a dark mass
The foregut of this flea is blocked by a Y. pestis biofilm, which is a prerequisite for efficient transmission.

A fleabite infected with the bacterium Y. pestis
The image shows a child with a fleabite on the abdomen. The site of inoculation has become ulcerated. A prominent axillary lymph node (bubo) is also noted.
Bubonic plague:
Pneumonic plague:
Septicemic plague:

Bubonic plague: swollen inguinal lymph nodes on a person infected with the bubonic plague
Image: “Plague buboes” by the CDC. License: Public domain.
Septicemic plague: Y. pestis infection resulting in necrotic changes on the right foot
Image: “PlagueTypes” by the CDC. License: Public domain.
Patient with the plague
The image shows gangrene of the fingers, the effect of Y. pestis infection through bioterrorism.
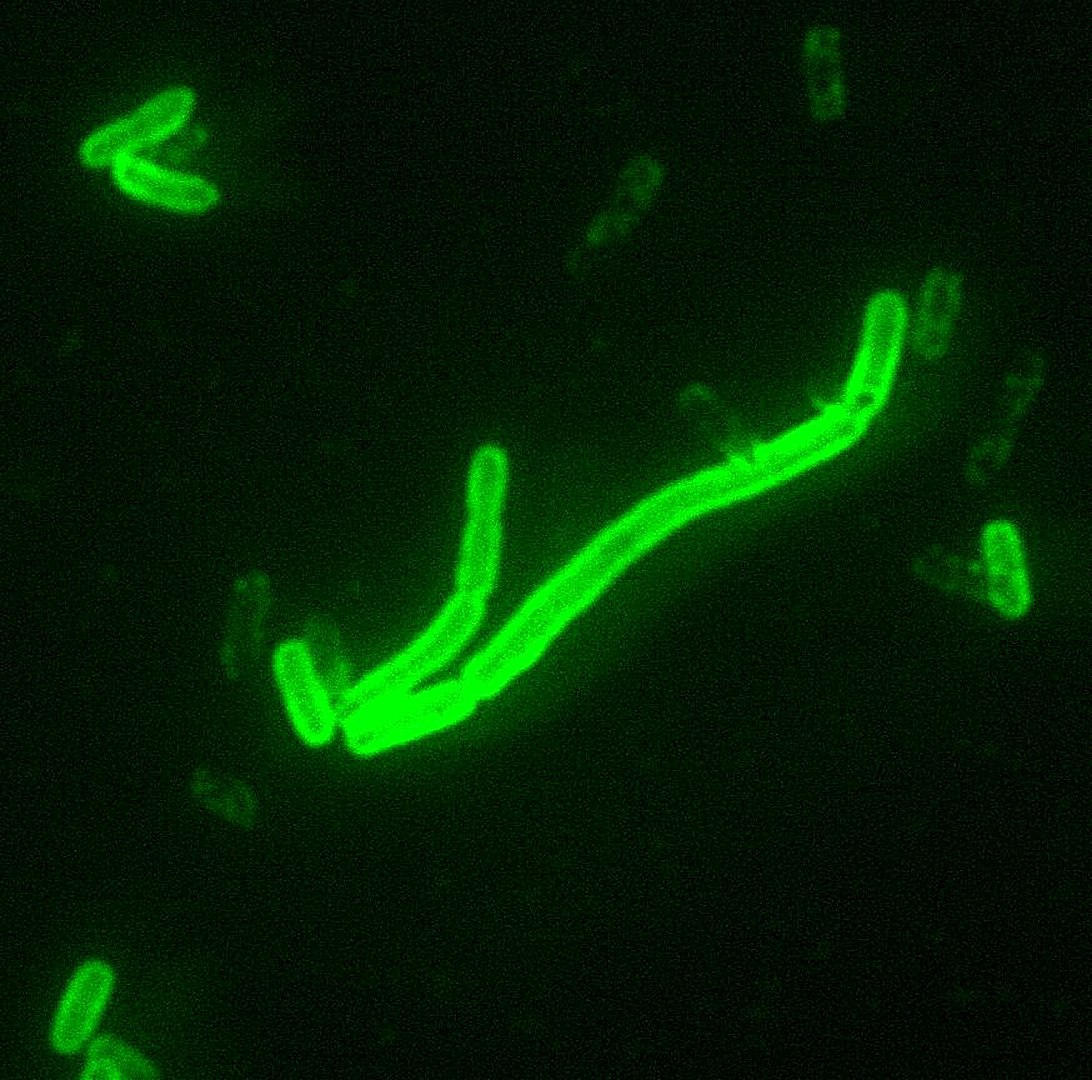
Yersinia pestis: under microscopy, dyed with fluorescent stain
Image: “Yersinia pestis fluorescent” by the CDC/Courtesy of Larry Stauffer, Oregon State Public Health Laboratory. License: Public domain.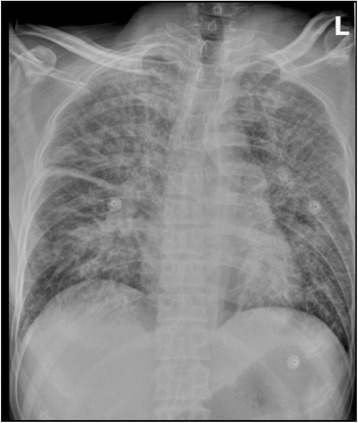
A patient with pneumonic plague
A chest X-ray shows increased pulmonary markings, with thick interlobar pleura in a patient who presented with fever, cough, and dyspnea after exposure to a herding dog.