Bacillus are aerobic, spore-forming, gram-positive Gram-Positive Penicillins bacilli Bacilli Shigella. Two pathogenic species are Bacillus anthracis Bacillus anthracis A species of bacteria that causes anthrax in humans and animals. Anthrax (B. anthracis) and B. cereus. Bacillus anthracis Bacillus anthracis A species of bacteria that causes anthrax in humans and animals. Anthrax has a unique polypeptide capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides composed of D-glutamate and is associated with cutaneous, gastrointestinal, and pulmonary anthrax Anthrax Anthrax is an infection caused by the bacterium Bacillus anthracis, which usually targets the skin, lungs, or intestines. Anthrax is a zoonotic disease and is usually transmitted to humans from animals or through animal products. Symptoms depend on which organ system is affected. Anthrax. Importantly, B. anthracis is classified as a bioterrorism Bioterrorism The use of biological agents in terrorism. This includes the malevolent use of bacteria; viruses; or other biological toxins against people, animals; or plants. Anthrax agent. Bacillus cereus is associated with 2 forms of food poisoning Food poisoning Acute illnesses, usually affecting the gastrointestinal tract, brought on by consuming contaminated food or beverages. Most of these diseases are infectious, caused by a variety of bacteria, viruses, or parasites that can be foodborne. Sometimes the diseases are caused by harmful toxins from the microbes or other chemicals present in the food. Especially in the latter case, the condition is often called food poisoning. Clostridia, diarrheal and emetic, both of which are self-limited and require only supportive care.
Last updated: Jan 2, 2024
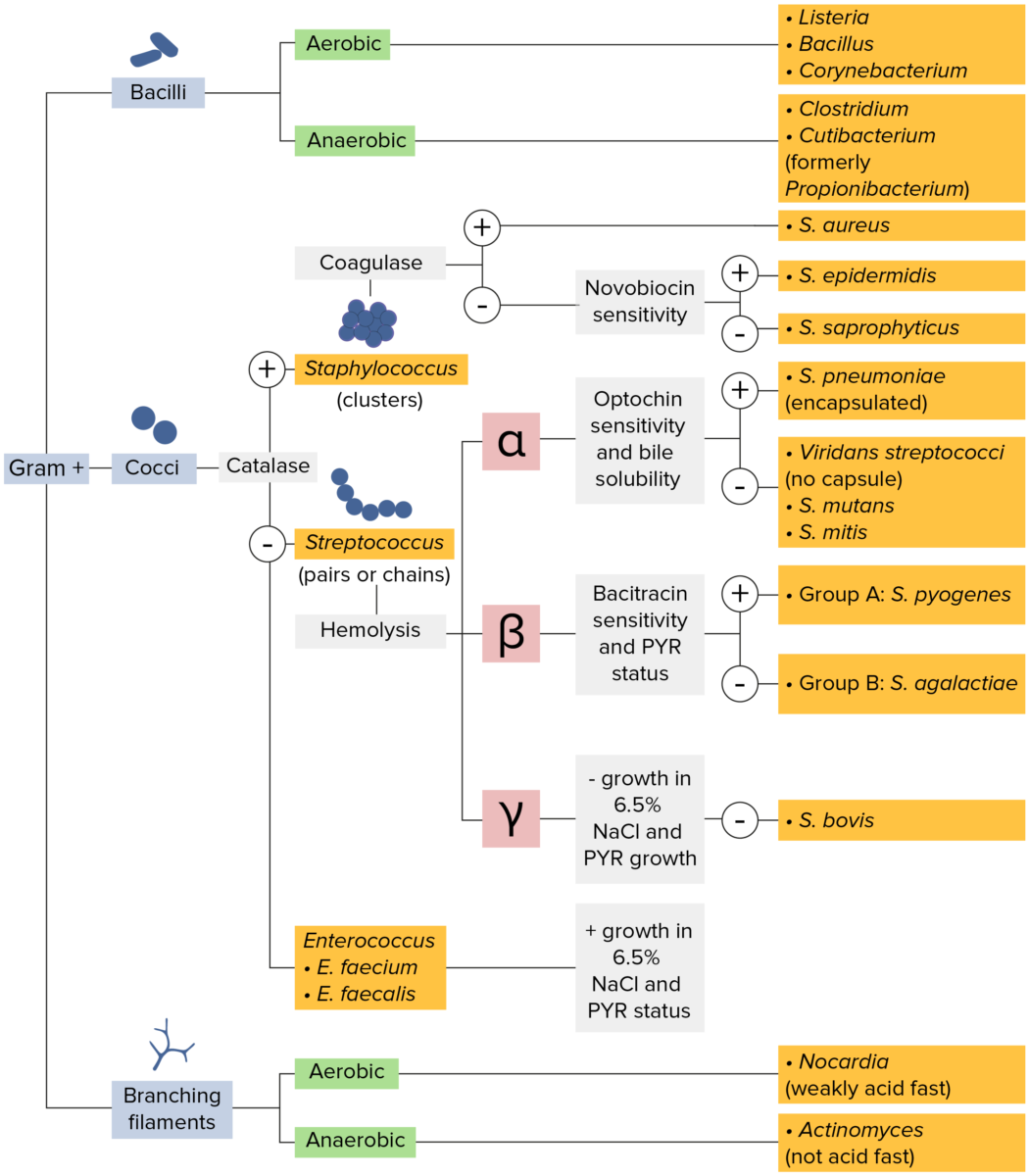
Gram-positive bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thick layer of peptidoglycan retain the crystal violet stain utilized in Gram staining but are not affected by the safranin counterstain. These bacteria appear as purple-blue on the stain, indicating that they are gram positive. The bacteria can be further classified according to morphology (branching filaments, bacilli, and cocci in clusters or chains) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The cocci can also be further identified. Staphylococci can be narrowed down on the basis of the presence of the enzyme coagulase and on their sensitivity to the antibiotic novobiocin. Streptococci are grown on blood agar and classified on the basis of which form of hemolysis they employ (α, β, or γ). Streptococci are further narrowed on the basis of their response to the pyrrolidonyl-β-naphthylamide (PYR) test, their sensitivity to specific antimicrobials (optochin and bacitracin), and their ability to grow on sodium chloride (NaCl) media.
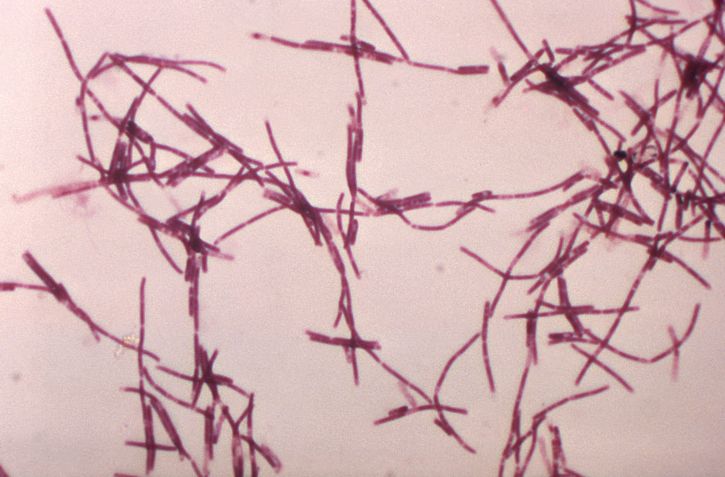
Bacillus anthracis: electron micrograph
Image: “Gramm, Mikrophotographie, zahlreich, Bazillus, anthracis, Bakterien” by Dr. William A. Clark. License: Public domain.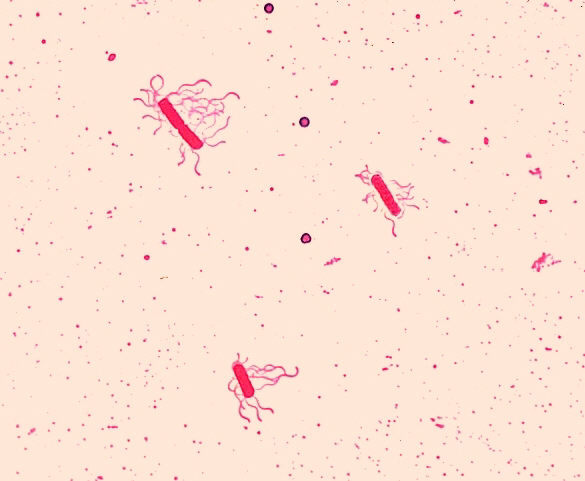
Bacillus cereus: electron micrograph
Image: “Bacillus cereus. Leifson flagella stain” by Dr. William A. Clark. License: Public domain.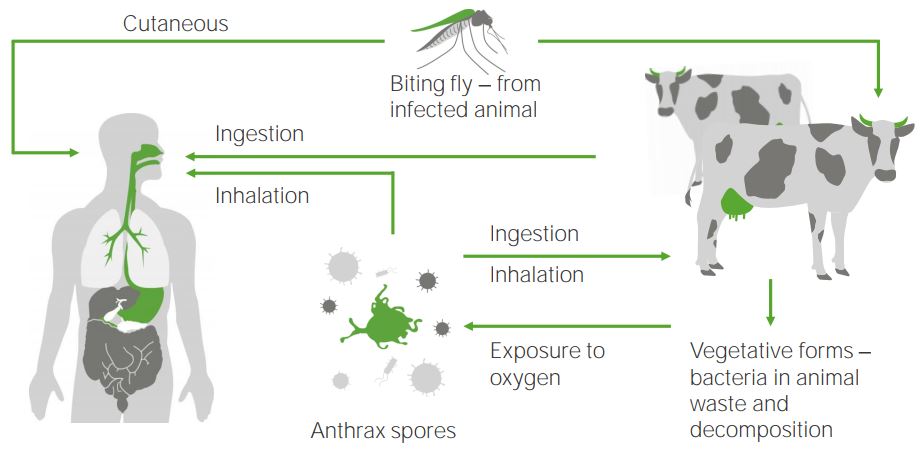
The anthrax cycle
Bacillus anthracis (anthrax spores) infect humans or mammals via different processes: either via ingestion, inhalation, or through cutaneous pathways by bites from an infected insect. Anthrax spores originate from vegetation in excreted waste from cattle, which is exposed to oxygen.
In the United States, 3 clinical manifestations occur.

A skin lesion caused by anthrax; the characteristic black eschar
Image: “Anthrax PHIL 2033” by the CDC/James H. Steele. License: Public domain.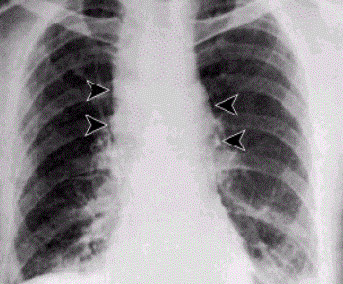
Mediastinal widening, associated with inhalation anthrax
Image: “Anthrax – inhalational” by the CDC. License: Public domain.