Shigella is a genus of gram-negative, non-lactose-fermenting facultative intracellular Facultative intracellular Yersinia spp./Yersiniosis bacilli. Infection spreads most commonly via person-to-person contact or through contaminated food and water. Humans are the only known reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli. Because it is resistant to acid, Shigella spp. survive transit through the stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy; thus, only a small amount of inoculum is needed to cause disease. Shigellosis (Shigella dysentery Dysentery Acute inflammation of the intestine associated with infectious diarrhea of various etiologies, generally acquired by eating contaminated food containing toxins, biological derived from bacteria or other microorganisms. Dysentery is characterized initially by watery feces then by bloody mucoid stools. It is often associated with abdominal pain; fever; and dehydration. Gastroenteritis) results in fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, abdominal pain Abdominal Pain Acute Abdomen, and bloody diarrhea Bloody diarrhea Diarrhea, which are effects of the toxins and epithelial-cell invasion of the organism. In the majority of cases, symptoms resolve within a few days. However, complications of dehydration Dehydration The condition that results from excessive loss of water from a living organism. Volume Depletion and Dehydration, hemolytic uremic syndrome Hemolytic uremic syndrome A syndrome that is associated with microvascular diseases of the kidney, such as renal cortical necrosis. It is characterized by hemolytic anemia; thrombocytopenia; and acute renal failure. Hypocoagulable Conditions, toxic megacolon Toxic megacolon An acute form of megacolon, severe pathological dilatation of the colon. It is associated with clinical conditions such as ulcerative colitis; Crohn disease; amebic dysentery; or Clostridium enterocolitis. Megacolon, or reactive arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis can arise. Treatment is primarily using fluid and electrolyte replacement and antibiotics.
Last updated: Sep 8, 2022
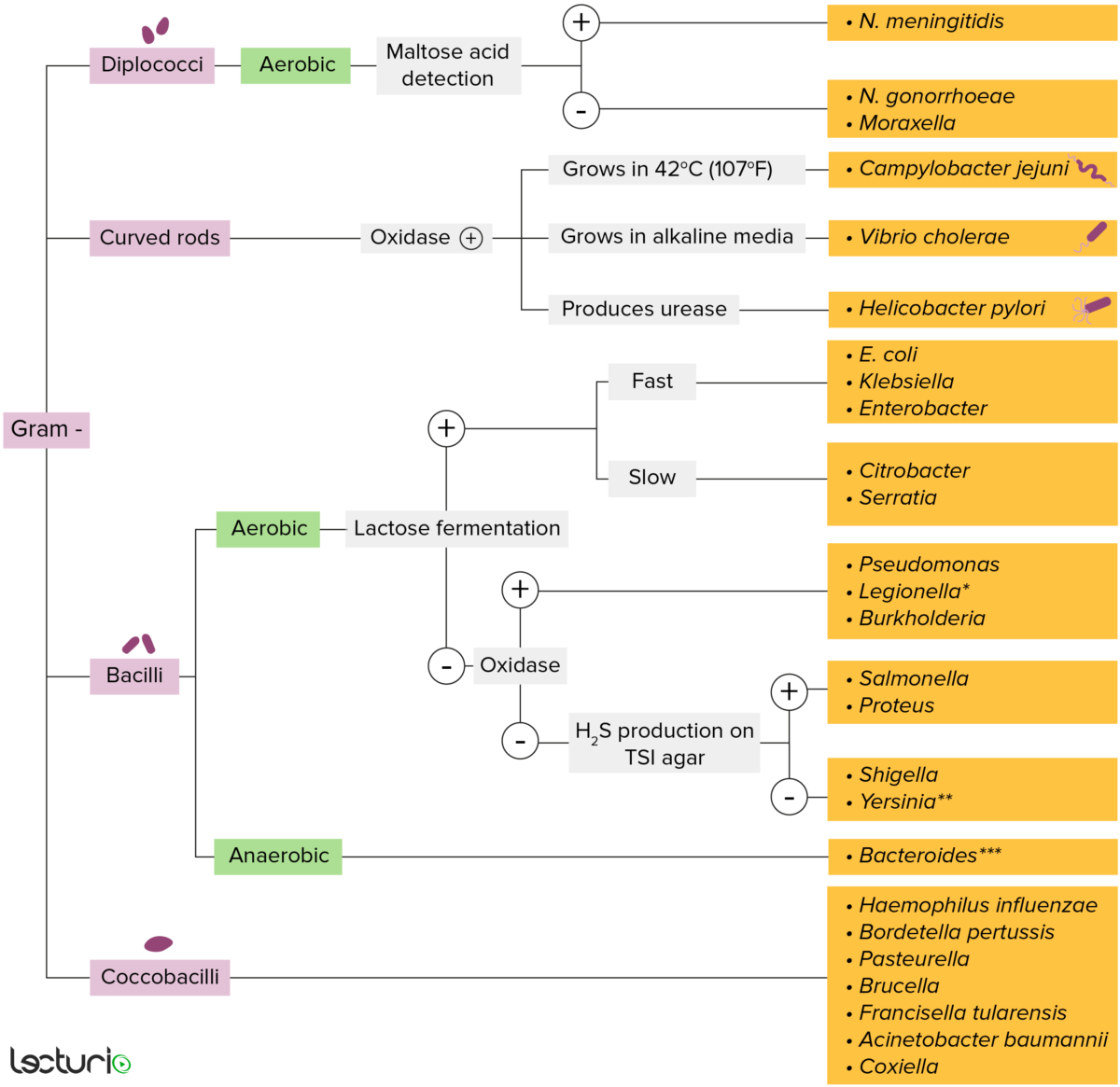
Gram-negative bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thin layer of peptidoglycan do not retain the crystal violet stain utilized in Gram staining. These bacteria do, however, retain the safranin counterstain and thus appear as pinkish-red on the stain, making them gram negative. These bacteria can be further classified according to morphology (diplococci, curved rods, bacilli, and coccobacilli) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The bacteria can be more narrowly identified by growing them on specific media (triple sugar iron (TSI) agar) where their enzymes can be identified (urease, oxidase) and their ability to ferment lactose can be tested.
* Stains poorly on Gram stain
** Pleomorphic rod/coccobacillus
*** Require special transport media
Serogroups defined by specific O antigens:
To help remember the modes of transmission of Shigella, remember the “4 Fs:”
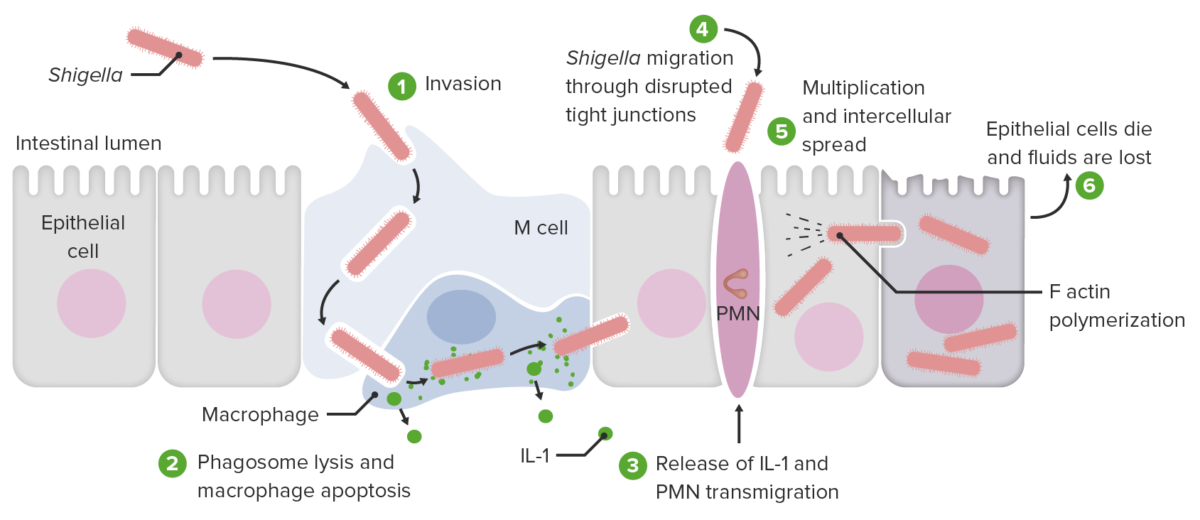
Invasion and cell-to-cell spread by Shigella:
1. Pathogen invades and is engulfed by the M cell (transcytosis).
2. Pathogen reaches subepithelial macrophages and dendritic cells, then induces macrophage apoptosis. Shigella sp. is released along with interleukin-1 (IL-1) and other cytokines. The pathogen is then engulfed into the adjacent epithelial cell in a membrane-bound compartment (epithelial-cell entry).
3. Released interleukins also recruit polymorphonuclear leukocytes (PMNs), which destabilize the cellular junctions. This is another entryway for the pathogen (PMN transmigration).
4. Shigella sp. passes through the disrupted tight junctions and then the pathogen enters the epithelial cell. Once inside, the host cell actin nucleators are hijacked. Actin-based motility (ABM; actin tail) propels the pathogen to reach the plasma membrane, where the infected cell contacts another cell.
5. Multiplication and intercellular spread are facilitated by cellular protrusion (with Shigella) and elongation into the adjacent cell. The protrusion resolves as a double-membrane vacuole. The pathogen lyses the membrane, escapes, and enters the adjacent cell. The adjacent cell is infected and this process is repeated in other cells.
6. As each invaded epithelial cell dies, fluids are lost.
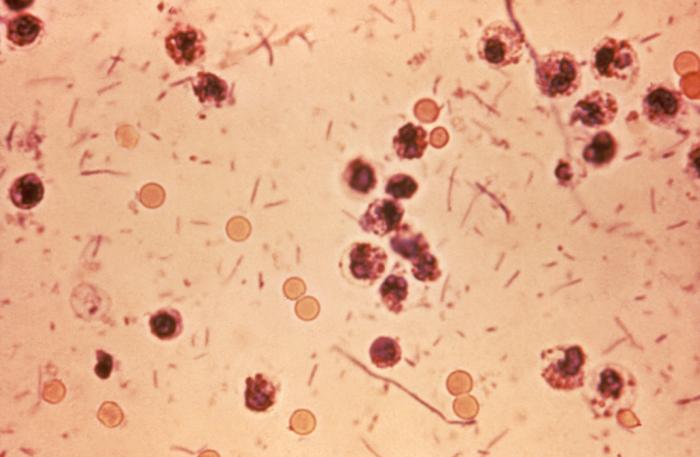
Shigellosis (“Shigella dysentery”): Stool sample from a patient with shigellosis (diarrhea with bloody stools, fever, and abdominal cramps). Shigella seen as rods in the smear
Image: “Shigella stool” by Centers for Disease Control and Prevention Public Health Image Library. License: Public Domain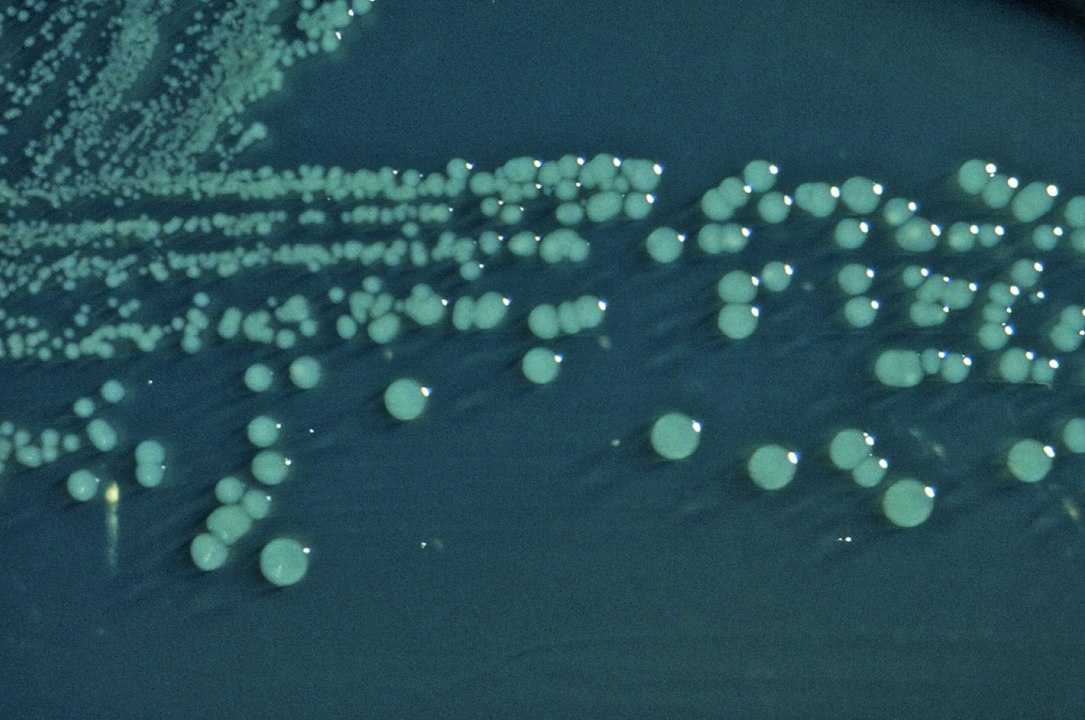
Shigella on Hektoen enteric (HE) agar: Colonies of S. boydii grown on HE agar have a raised, green, and moist appearance.
Image: “Shigella boydii 01” by CDC. License: Public DomainShigella and Salmonella Salmonella Salmonellae are gram-negative bacilli of the family Enterobacteriaceae. Salmonellae are flagellated, non-lactose-fermenting, and hydrogen sulfide-producing microbes. Salmonella enterica, the most common disease-causing species in humans, is further classified based on serotype as typhoidal (S. typhi and paratyphi) and nontyphoidal (S. enteritidis and typhimurium). Salmonella invade the gastrointestinal tract, causing diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea.
| Shigella | Salmonella Salmonella Salmonellae are gram-negative bacilli of the family Enterobacteriaceae. Salmonellae are flagellated, non-lactose-fermenting, and hydrogen sulfide-producing microbes. Salmonella enterica, the most common disease-causing species in humans, is further classified based on serotype as typhoidal (S. typhi and paratyphi) and nontyphoidal (S. enteritidis and typhimurium). Salmonella | |
|---|---|---|
| Gram stain Gram stain Klebsiella/structure | Gram-negative bacilli | Gram-negative bacilli |
| Lactose fermentation | Non-lactose-fermenting | Non-lactose-fermenting |
| Oxidase Oxidase Neisseria | Negative | Negative |
| H2S production | No | Yes |
| Motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility | No | Yes (with flagella Flagella A whiplike motility appendage present on the surface cells. Prokaryote flagella are composed of a protein called flagellin. Bacteria can have a single flagellum, a tuft at one pole, or multiple flagella covering the entire surface. In eukaryotes, flagella are threadlike protoplasmic extensions used to propel flagellates and sperm. Flagella have the same basic structure as cilia but are longer in proportion to the cell bearing them and present in much smaller numbers. Helicobacter) |
| Virulence factors Virulence factors Those components of an organism that determine its capacity to cause disease but are not required for its viability per se. Two classes have been characterized: toxins, biological and surface adhesion molecules that affect the ability of the microorganism to invade and colonize a host. Haemophilus | Endotoxin Endotoxin Toxins closely associated with the living cytoplasm or cell wall of certain microorganisms, which do not readily diffuse into the culture medium, but are released upon lysis of the cells. Proteus, Shiga toxin Shiga toxin A class of toxins that inhibit protein synthesis by blocking the interaction of ribosomal RNA; with peptide elongation factors. They include shiga toxin which is produced by Shigella dysenteriae and a variety of shiga-like toxins that are produced by pathologic strains of Escherichia coli such as Escherichia coli o157. Diarrheagenic E. coli | Endotoxin Endotoxin Toxins closely associated with the living cytoplasm or cell wall of certain microorganisms, which do not readily diffuse into the culture medium, but are released upon lysis of the cells. Proteus, Vi capsular antigen Antigen Substances that are recognized by the immune system and induce an immune reaction. Vaccination |
| Reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli | Humans | Humans (S. typhi), animals Animals Unicellular or multicellular, heterotrophic organisms, that have sensation and the power of voluntary movement. Under the older five kingdom paradigm, animalia was one of the kingdoms. Under the modern three domain model, animalia represents one of the many groups in the domain eukaryota. Cell Types: Eukaryotic versus Prokaryotic |
| Dose to produce disease | Small inoculum (acid stable) | Large dose (inactivated by acids Acids Chemical compounds which yield hydrogen ions or protons when dissolved in water, whose hydrogen can be replaced by metals or basic radicals, or which react with bases to form salts and water (neutralization). An extension of the term includes substances dissolved in media other than water. Acid-Base Balance) |
| Infection spread | Cell-to-cell (no hematogenous Hematogenous Hepatocellular Carcinoma (HCC) and Liver Metastases spread) | Can spread hematogenously |