Vitiligo is the most common depigmenting disorder and is caused by the destruction of melanocytes Melanocytes Mammalian pigment cells that produce melanins, pigments found mainly in the epidermis, but also in the eyes and the hair, by a process called melanogenesis. Coloration can be altered by the number of melanocytes or the amount of pigment produced and stored in the organelles called melanosomes. The large non-mammalian melanin-containing cells are called melanophores. Skin: Structure and Functions. The etiology is unknown; however, genetic and autoimmune factors may play a role. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with hypo- or depigmented macules or patches which often occur on the face, hands, knees, and/or genitalia. The diagnosis is clinical. Management depends on the severity and can include sun protection, topical or oral steroids Steroids A group of polycyclic compounds closely related biochemically to terpenes. They include cholesterol, numerous hormones, precursors of certain vitamins, bile acids, alcohols (sterols), and certain natural drugs and poisons. Steroids have a common nucleus, a fused, reduced 17-carbon atom ring system, cyclopentanoperhydrophenanthrene. Most steroids also have two methyl groups and an aliphatic side-chain attached to the nucleus. Benign Liver Tumors, topical calcineurin inhibitors Calcineurin Inhibitors Compounds that inhibit or block the phosphatase activity of calcineurin. Immunosuppressants, immunosuppressants Immunosuppressants Immunosuppressants are a class of drugs widely used in the management of autoimmune conditions and organ transplant rejection. The general effect is dampening of the immune response. Immunosuppressants, and phototherapy Phototherapy Treatment of disease by exposure to light, especially by variously concentrated light rays or specific wavelengths. Hyperbilirubinemia of the Newborn.
Last updated: May 17, 2024
Vitiligo is a progressive skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions condition in which there is destruction of melanocytes Melanocytes Mammalian pigment cells that produce melanins, pigments found mainly in the epidermis, but also in the eyes and the hair, by a process called melanogenesis. Coloration can be altered by the number of melanocytes or the amount of pigment produced and stored in the organelles called melanosomes. The large non-mammalian melanin-containing cells are called melanophores. Skin: Structure and Functions resulting in the loss of skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions pigmentation.
The cause of vitiligo is unknown, but is postulated to be a result of multiple factors.
Vitiligo results in hypopigmented or depigmented areas.

Large patches of hypopigmentation in a patient with vitiligo
Image: “Split thickness skin grafting in patients with stable vitiligo” by Sameem F, Sultan SJ, Ahmad QM. License: CC BY 2.0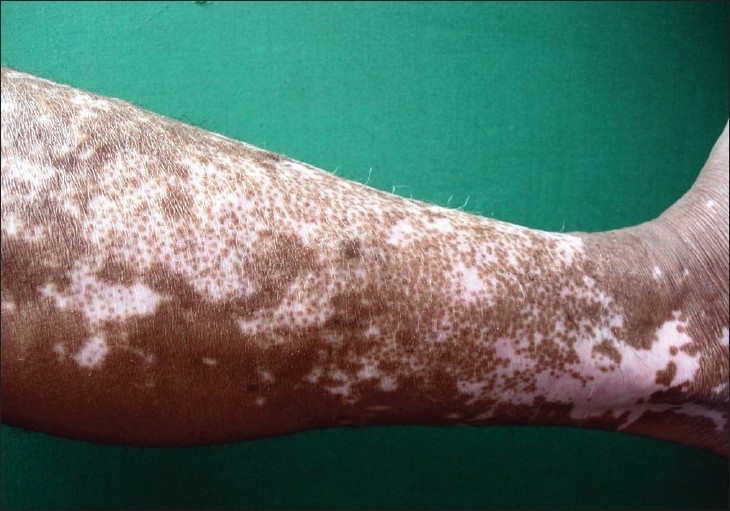
Depigmentation seen in a patient with vitiligo
Image: “Vitiligo and the melanocyte reservoir” by Falabella R. License: CC BY 2.0The diagnosis is usually clinical. However, the following examinations may be used if the diagnosis is unclear:
No cure is currently available. Management generally aims to slow the progression of the disease and address cosmetic issues.