Psoriasis is a common T-cell–mediated inflammatory skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions condition. The etiology is unknown, but is thought to be due to genetic inheritance and environmental triggers Triggers Hereditary Angioedema (C1 Esterase Inhibitor Deficiency). There are 4 major subtypes, with the most common form being chronic plaque Plaque Primary Skin Lesions psoriasis. Plaques are well-circumscribed and salmon-colored, with silvery scales Scales Dry or greasy masses of keratin that represent thickened stratum corneum. Secondary Skin Lesions. Plaques commonly appear on the scalp and extensor surfaces of the extremities. Diagnosis is clinical. Treatment options are determined by the percentage of body surface area (BSA) affected and include topical corticosteroids Corticosteroids Chorioretinitis, retinoids Retinoids Retinol and derivatives of retinol that play an essential role in metabolic functioning of the retina, the growth of and differentiation of epithelial tissue, the growth of bone, reproduction, and the immune response. Dietary vitamin A is derived from a variety of carotenoids found in plants. It is enriched in the liver, egg yolks, and the fat component of dairy products. Fat-soluble Vitamins and their Deficiencies, calcineurin inhibitors Calcineurin Inhibitors Compounds that inhibit or block the phosphatase activity of calcineurin. Immunosuppressants, disease-modifying antirheumatic drugs Disease-modifying antirheumatic drugs Disease-modifying antirheumatic drugs are antiinflammatory medications used to manage rheumatoid arthritis. The medications slow, but do not cure, the progression of the disease. The medications are classified as either synthetic or biologic agents and each has unique mechanisms of action and side effects. Disease-Modifying Antirheumatic Drugs (DMARDs) ( DMARDs DMARDs Disease-modifying antirheumatic drugs are antiinflammatory medications used to manage rheumatoid arthritis. The medications slow, but do not cure, the progression of the disease. The medications are classified as either synthetic or biologic agents and each has unique mechanisms of action and side effects. Disease-Modifying Antirheumatic Drugs (DMARDs)), biologics, and phototherapy Phototherapy Treatment of disease by exposure to light, especially by variously concentrated light rays or specific wavelengths. Hyperbilirubinemia of the Newborn.
Last updated: May 17, 2024
Psoriasis is a complex disease marked by a deregulated T-cell–mediated inflammatory process, resulting in keratinocyte Keratinocyte Epidermal cells which synthesize keratin and undergo characteristic changes as they move upward from the basal layers of the epidermis to the cornified (horny) layer of the skin. Successive stages of differentiation of the keratinocytes forming the epidermal layers are basal cell, spinous or prickle cell, and the granular cell. Erythema Multiforme proliferation and dysfunctional differentiation.

Psoriatic lesion on the knee
Image: “Psoriatic lesion on the knee” by Department of Neurology, Wakayama Medical University, 811-1 Kimiidera, Wakayama 641-8510, Japan. License: CC BY 2.0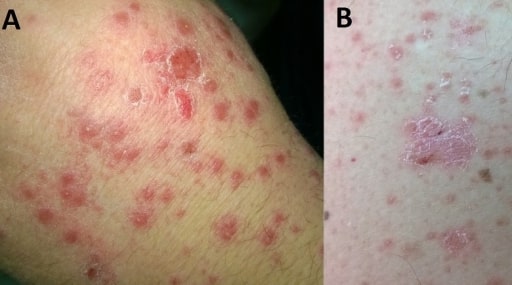
Small, red, drop-like lesions of guttate psoriasis located on a hand (A) and arm (B)
Image: “ F0001” by Department of Internal Medicine, General Hospital of Larissa, Larissa, Greece. License: CC BY 2.0
Erythrodermic psoriasis in a patient treated for acute hepatitis C infection: Generalized erythema, with varying scaling, affecting the entire body surface is characteristic of this subtype of psoriasis.
Image: “Erythrodermic psoriasis at treatment week 10” by Division of Infectious Diseases and Hospital Hygiene, Cantonal Hospital St.Gallen, Rorschacherstrasse 95, 9007, St.Gallen, Switzerland. License: CC BY 4.0
Pustular psoriasis, characterized by the development of annular erythematous plaques with peripheral pustules and scaling: Notice the pinhead-sized sterile pustules that make this subtype of psoriasis distinct.
Image: “bjd14003-fig-0001” by Institute of Genetic Medicine, Newcastle University, Newcastle upon Tyne, NE1 3BZ, U.K. License: CC BY 4.0, edited by Lecturio.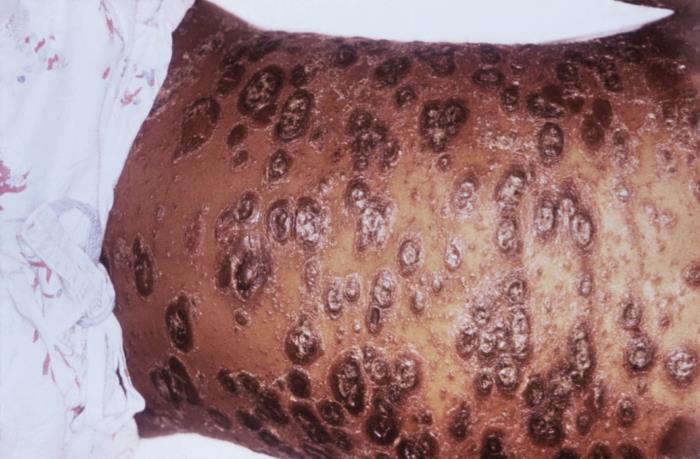
Chronic plaque psoriasis of the abdomen: Notice the numerous raised, red lesions surrounded by scaling. This subtype can range from a few patches to multiple plaques covering large areas, such as the one shown here.
Image: “ 5503” by CDC/ Gavin Hart. License: Public Domain
Inverse (intertriginous) psoriasis of the gluteal cleft: This location is not typical of psoriasis, which is why it is known as inverse psoriasis. Notice the symmetric, smooth, shiny, erythematous plaques characteristic of this form of psoriasis. There is no scaling due to the moistness of the area.
Image: “ 4049” by CDC/ Dr. Gavin Hart. License: Public Domain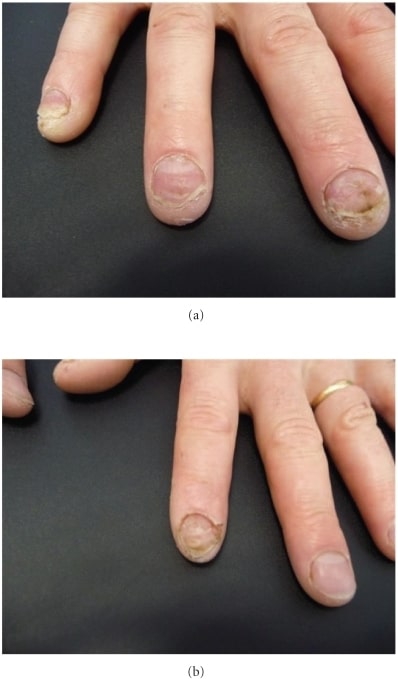
Nail psoriasis presenting with characteristic features of subungual hyperkeratosis, pitting, and onycholysis of right-hand fingernails 3, 4, and 5
Image: “Subungual hyperkeratosis” by Department of Dermatology, Centre Hospitalier de Saint-Brieuc, 10, rue Marcel Proust, 22000 Saint-Brieuc, France. License: CC BY 3.0
Palmoplantar psoriasis involves the palms and/or soles only: The characteristic findings of this special site include erythematous and hyperkeratotic plaques. Painful fissures may also be present.
Image: “ F0001” by Dermatology Department, Bir Usta Milad Hospital, Tripoli, Libya. License: CC BY 2.0
Psoriatic arthritis presenting as symmetric polyarthritis affecting the proximal interphalangeal joints of the fingers. Psoriatic nail changes are also evident in this photo.
Image: “ fig1” by Rheumatology Department, Southport and Ormskirk Hospital NHS Trust, Liverpool University, PR8 6PN, UK. License: CC BY 3.0
Arthritis mutilans is a common late finding of psoriatic arthritis.
Image: “A patient with arthritis mutilans with digital shortening” by Department of Molecular Medicine and Pathology, University of Auckland, Park Road, Auckland 1010, New Zealand. License: CC BY 2.0Diagnosis is established by the clinical history and physical examination findings.
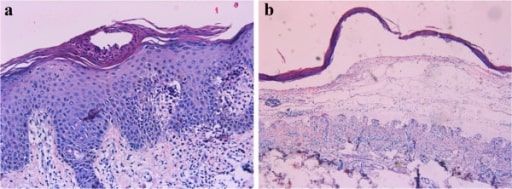
Histopathology from a punch biopsy showing characteristic findings of psoriasis: (a) Munro’s microabscesses, hyperkeratosis, hypogranulosis, parakeratosis, acanthosis with an elongation of rete ridges, and dilated blood vessels; (b) subepidermal blister filled with serous exudate.
Image: “Characteristics of skin histopathology” by Department of Dermatology, Qianfoshan Hospital, Shandong University, Jinan 250014, China. License: CC BY 2.0Treatment is based on severity, lesion distribution, type, comorbidities Comorbidities The presence of co-existing or additional diseases with reference to an initial diagnosis or with reference to the index condition that is the subject of study. Comorbidity may affect the ability of affected individuals to function and also their survival; it may be used as a prognostic indicator for length of hospital stay, cost factors, and outcome or survival. St. Louis Encephalitis Virus, and response.