Mastitis is inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the breast tissue with or without infection. The most common form of mastitis is associated with lactation Lactation The processes of milk secretion by the maternal mammary glands after parturition. The proliferation of the mammary glandular tissue, milk synthesis, and milk expulsion or let down are regulated by the interactions of several hormones including estradiol; progesterone; prolactin; and oxytocin. Breastfeeding in the first few weeks after birth. Non-lactational mastitis includes periductal mastitis and idiopathic Idiopathic Dermatomyositis granulomatous mastitis ( IGM IgM A class of immunoglobulin bearing mu chains (immunoglobulin mu-chains). Igm can fix complement. The name comes from its high molecular weight and originally being called a macroglobulin. Immunoglobulins: Types and Functions). Lactational mastitis is most commonly caused by Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess that is introduced into the breast milk during breastfeeding Breastfeeding Breastfeeding is often the primary source of nutrition for the newborn. During pregnancy, hormonal stimulation causes the number and size of mammary glands in the breast to significantly increase. After delivery, prolactin stimulates milk production, while oxytocin stimulates milk expulsion through the lactiferous ducts, where it is sucked out through the nipple by the infant. Breastfeeding. The etiology of non-lactational mastitis is poorly understood, but periductal mastitis is commonly associated with smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, and IGM IgM A class of immunoglobulin bearing mu chains (immunoglobulin mu-chains). Igm can fix complement. The name comes from its high molecular weight and originally being called a macroglobulin. Immunoglobulins: Types and Functions is frequently associated with Corynebacterium Corynebacterium Corynebacteria are gram-positive, club-shaped bacilli. Corynebacteria are commonly isolated on tellurite or Loeffler's media and have characteristic metachromatic granules. The major pathogenic species is Corynebacterium diphtheriae, which causes a severe respiratory infection called diphtheria. Corynebacterium. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema, erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion, tenderness, and, possibly, a mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast in the breast. Diagnosis is usually clinical, although ultrasound, cultures, and biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma may be required in some cases. Management involves antibiotics, analgesics, drainage of any abscesses, and surgical duct excision for periductal mastitis.
Last updated: Mar 28, 2025
Mastitis refers to inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the breast that may or may not be associated with infection.
Periductal mastitis:
IGM IgM A class of immunoglobulin bearing mu chains (immunoglobulin mu-chains). Igm can fix complement. The name comes from its high molecular weight and originally being called a macroglobulin. Immunoglobulins: Types and Functions:
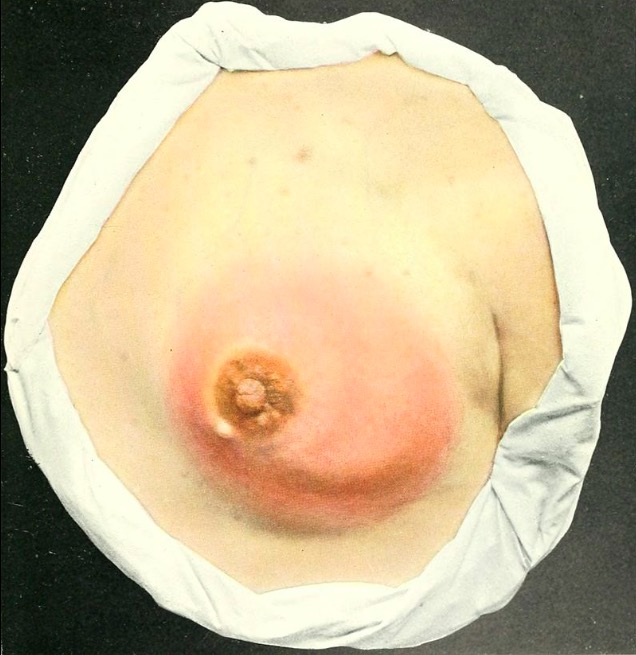
Lactational mastitis presents as an edematous and erythematous breast.
Image: “atlasofclinicals00bock” by Internet Archive Book Images. License: Public Domain
Idiopathic granulomatous mastitis (status post-incisional breast biopsy)
Image: “IGM of the right breast” by Dept. of Radiation Oncology, Johns Hopkins University School of Medicine, Baltimore, MD 21231, USA. License: CC BY 2.0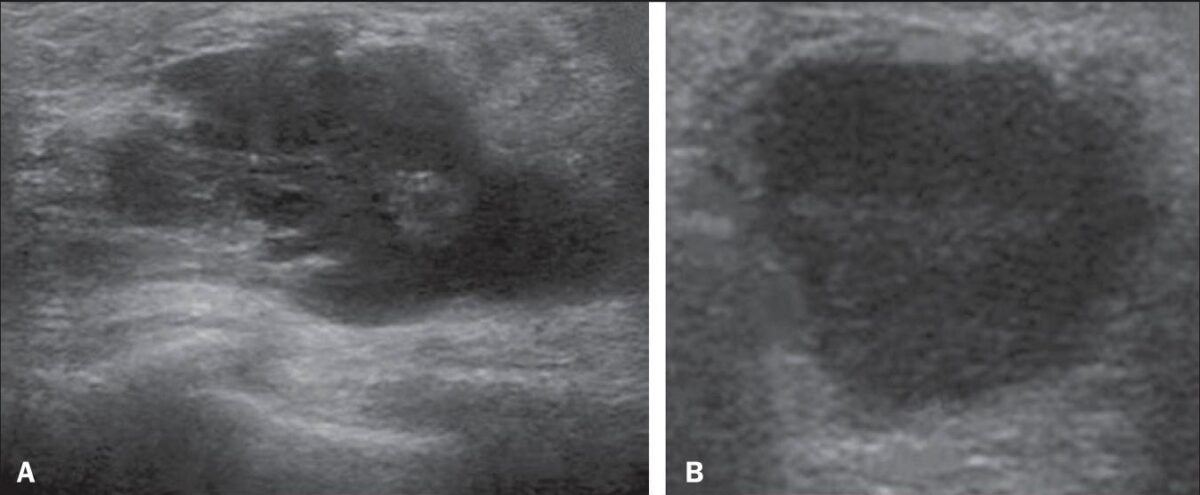
Ultrasound imaging of a breast abscess:
A: complex, with ill-defined borders
B: homogeneous in appearance with well-defined borders
Periductal mastitis:
IGM IgM A class of immunoglobulin bearing mu chains (immunoglobulin mu-chains). Igm can fix complement. The name comes from its high molecular weight and originally being called a macroglobulin. Immunoglobulins: Types and Functions:
Periductal mastitis:
IGM IgM A class of immunoglobulin bearing mu chains (immunoglobulin mu-chains). Igm can fix complement. The name comes from its high molecular weight and originally being called a macroglobulin. Immunoglobulins: Types and Functions: