The breasts are paired organs on the anterior thoracic wall and consist of mammary glands surrounded by connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology. The mammary glands are modified apocrine sweat glands Sweat glands Sweat-producing structures that are embedded in the dermis. Each gland consists of a single tube, a coiled body, and a superficial duct. Soft Tissue Abscess arranged into lobules and ducts that produce milk, which serves as nutrition for infants. Breasts are rudimentary and usually nonfunctioning in men. The shape and size of the breasts change during a woman’s life and menstrual cycles. Breasts are supplied by the axillary, internal thoracic, and intercostal arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology, and they are innervated by branches of the cervical plexus Cervical Plexus A network of nerve fibers originating in the upper four cervical spinal cord segments. The cervical plexus distributes cutaneous nerves to parts of the neck, shoulders, and back of the head. It also distributes motor fibers to muscles of the cervical spinal column, infrahyoid muscles, and the diaphragm. Peripheral Nerve Injuries in the Cervicothoracic Region.
Last updated: Nov 19, 2024
The breasts are paired organs on the anterior chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy and are composed of modified apocrine sweat glands Sweat glands Sweat-producing structures that are embedded in the dermis. Each gland consists of a single tube, a coiled body, and a superficial duct. Soft Tissue Abscess arranged into lobules and ducts.
Location:
Structure:
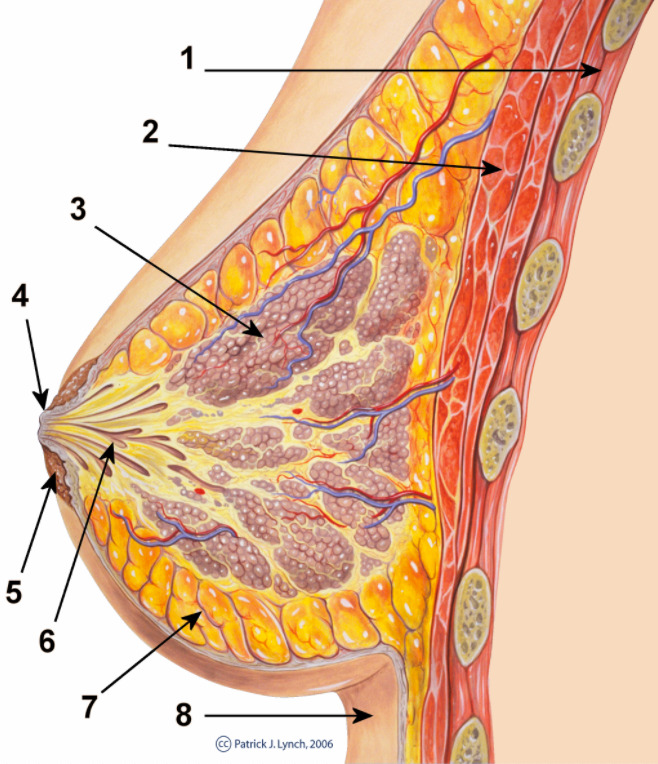
Lateral view of the breast, highlighting the:
1: Chest wall
2: Pectoralis musculature
3: Lobules
4: Nipple surface
5: Areola
6: Lactiferous ducts
7: Adipose tissue
8: Skin
The mammary gland is composed of modified apocrine sweat glands Sweat glands Sweat-producing structures that are embedded in the dermis. Each gland consists of a single tube, a coiled body, and a superficial duct. Soft Tissue Abscess divided into lobules, which reach the nipple Nipple The conic organs which usually give outlet to milk from the mammary glands. Examination of the Breast via lactiferous ducts. The ducts are composed of epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology surrounded by myoepithelial cells.
The arterial supply to the breast is via branches of the subclavian, axillary, and intercostal arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology with venous drainage into the subclavian, axillary, and azygos veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology. The innervation is from branches of the 2nd–6th intercostal nerves, with hormonal input via prolactin.

Vasculature of the breast
Image by Lecturio.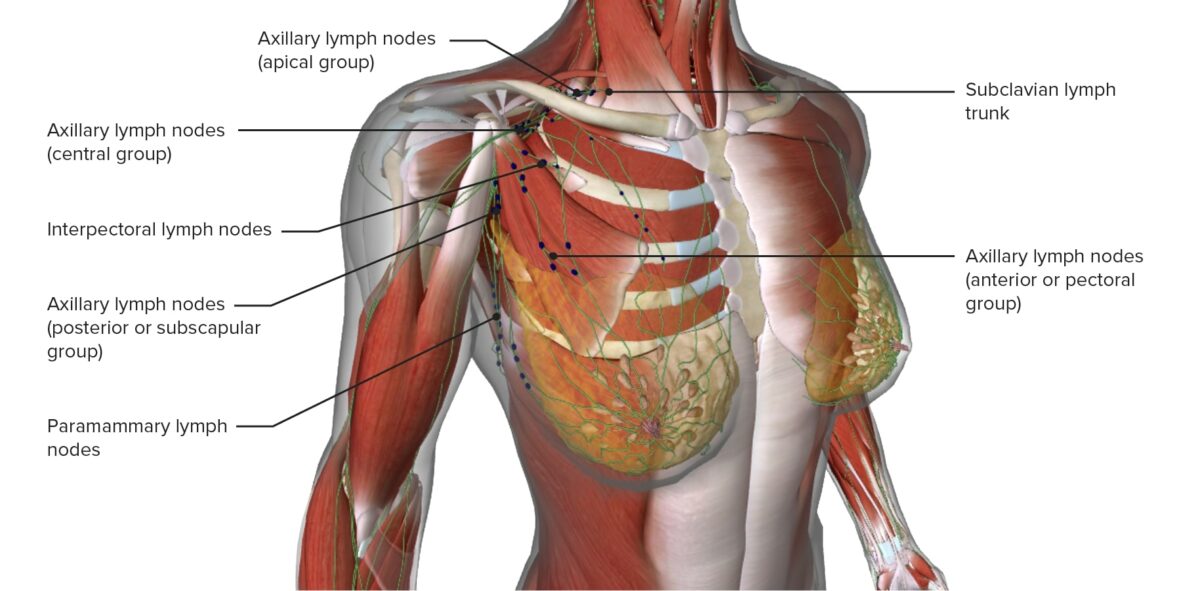
Lymphatic drainage of the breast
Image by Lecturio.