The lymphatic system Lymphatic system A system of organs and tissues that process and transport immune cells and lymph. Primary Lymphatic Organs consists of the lymphoid organs Lymphoid organs A system of organs and tissues that process and transport immune cells and lymph. Primary Lymphatic Organs containing the cells of the immune system Immune system The body's defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs and the lymphatic vessels, which transport interstitial fluid Interstitial fluid Body Fluid Compartments (as lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs) back to the venous circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment. Lymphatic vessels are spread extensively throughout the body, draining and filtering lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs, facilitating homeostasis Homeostasis The processes whereby the internal environment of an organism tends to remain balanced and stable. Cell Injury and Death, and aiding in defense against circulating pathogens. Fluid flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure is unidirectional, enabled by valves in the collecting lymphatic vessels. In vessels without valves, the muscle contraction of organs and adjacent blood vessels help in the fluid movement. To return to the venous circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment, the lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs is collected by the major lymphatic ducts: right lymphatic duct (collects from the right side of the head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess, the right side of the thorax, and the right upper extremity) and the thoracic duct (collects from the rest of the body). Pathologic conditions involving the lymphatic system Lymphatic system A system of organs and tissues that process and transport immune cells and lymph. Primary Lymphatic Organs are associated with infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, lymphatic damage, or injury and malignancies.
Last updated: Apr 2, 2025
The lymphatic system Lymphatic system A system of organs and tissues that process and transport immune cells and lymph. Primary Lymphatic Organs ( lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs vessels, lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs fluid, and lymphoid organs Lymphoid organs A system of organs and tissues that process and transport immune cells and lymph. Primary Lymphatic Organs) is part of the body’s immune system Immune system The body’s defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs.
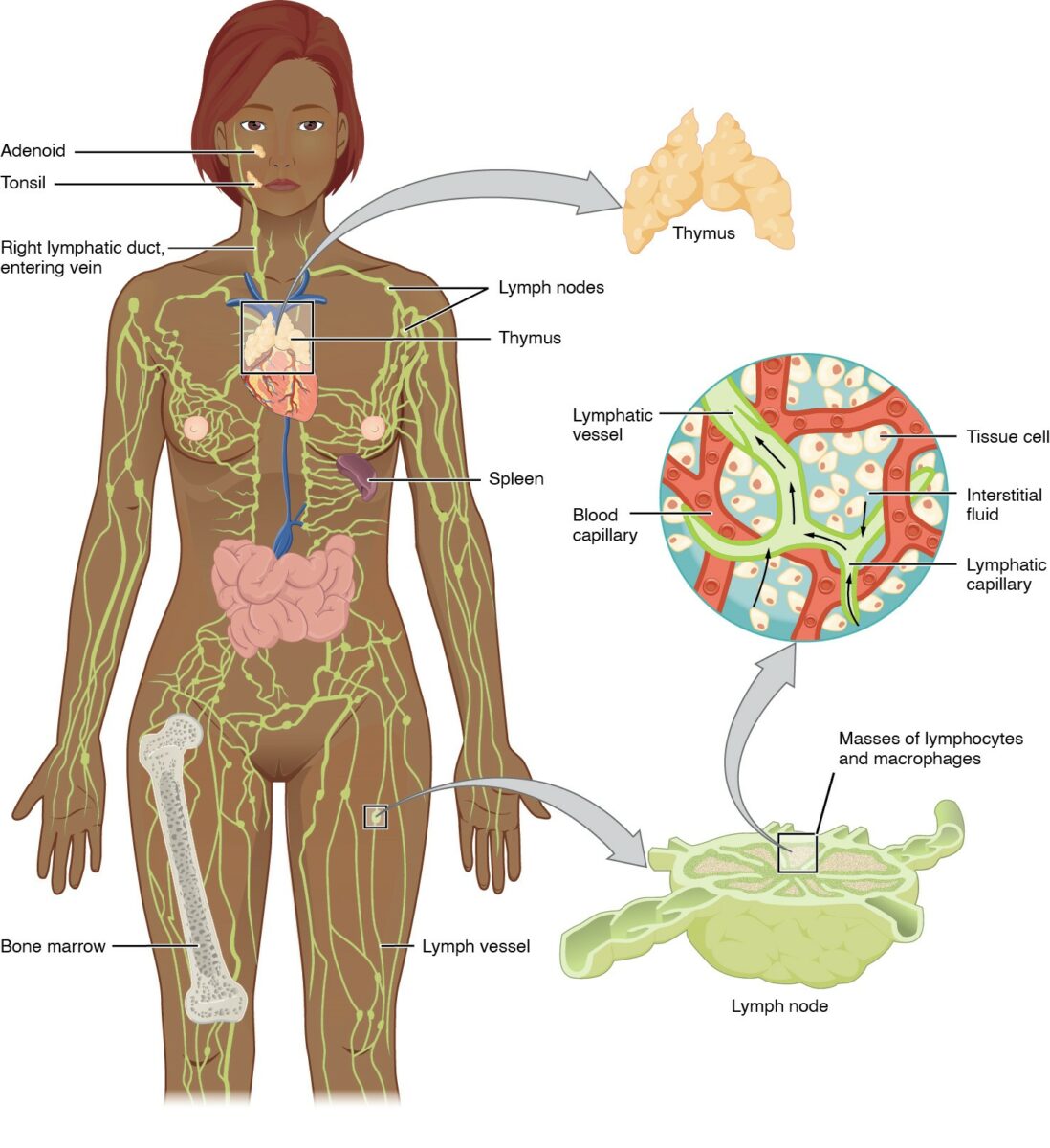
Anatomy of the lymphatic system: includes the primary (bone marrow, thymus) and secondary lymphoid organs (spleen, lymph nodes, and MALT).
Lymphatic vessels convey lymph to the larger lymphatic vessels in the torso, transporting fluid back to the venous circulation.
The glymphatic system is a specialized network of perivascular channels Channels The Cell: Cell Membrane in the CNS responsible for cerebrospinal fluid Cerebrospinal Fluid A watery fluid that is continuously produced in the choroid plexus and circulates around the surface of the brain; spinal cord; and in the cerebral ventricles. Ventricular System: Anatomy (CSF) and interstitial fluid Interstitial fluid Body Fluid Compartments (ISF) exchange within the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification.
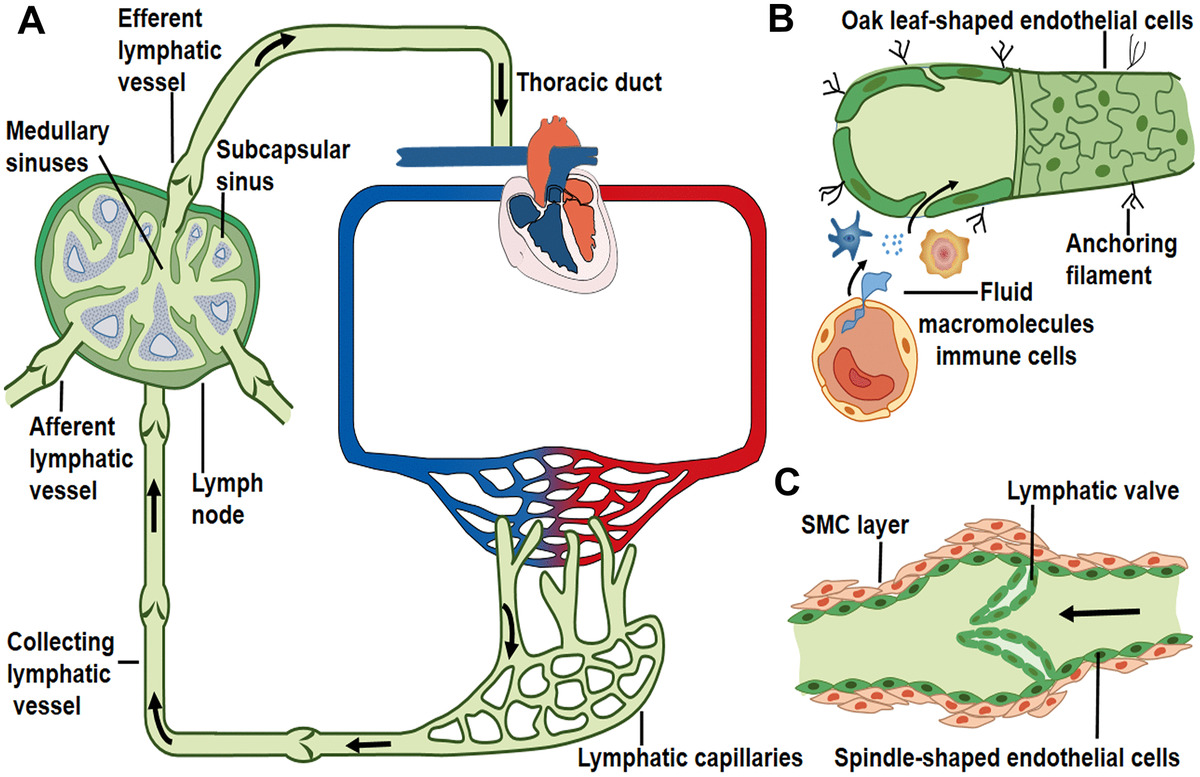
Lymph transport along lymphatic vessels:
A: Unidirectional lymph flow route: Lymphatic capillaries collect peripheral tissue fluid and converge into larger collecting vessels, and then lymph drains into the lymph node afferent lymphatic vessels and flows out from the efferent lymphatic vessel. Afterward, lymph fluid flows through the thoracic duct and the right lymphatic trunk/duct, and it eventually enters into venous circulation. The arrows indicate the direction of lymph flow.
B: Interstitial fluid, macromolecules, and immune cells that extravasate from blood vessels are collected by lymphatic capillaries. Initial lymphatics lack muscle layers and are composed of a layer of oak leaf-shaped endothelial cells, through which fluid (and constituents) enter.
C: Collecting lymphatics contain intraluminal valve and smooth muscle cell (SMC) layers that enable the unidirectional lymph flow.
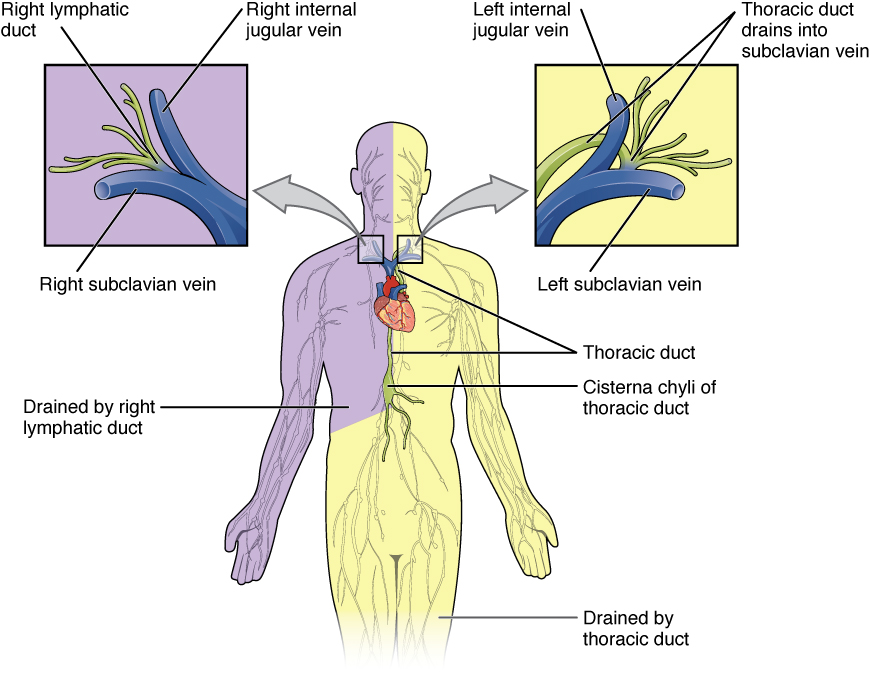
Lymphatic ducts:
The right lymphatic duct drains from the right side of the body (purple) above the diaphragm (the right side of the head and neck, the right side of the thorax, and the right upper extremity).
The thoracic duct drains from the rest of the body (yellow), particularly from both lower limbs, the left upper limb, and the left half of the head and neck.
These lymphatic ducts carry lymph to the venous system at the junction of the jugular and subclavian veins in the neck (right lymphatic duct on the right and thoracic duct on the left).
Lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy is caused by several etiologies, and an approach for determining the etiology is based on the location(s) of and areas drained by the lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node(s).
| Lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node cluster | Areas drained | Associated diseases |
|---|---|---|
| Cervical lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes | Head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess |
|
| Preauricular lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
|
Infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease in areas drained |
| Postauricular lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes | Parietotemporal scalp | Infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease (common in rubella Rubella An acute infectious disease caused by the rubella virus. The virus enters the respiratory tract via airborne droplet and spreads to the lymphatic system. Rubella Virus) |
| Supraclavicular lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
|
|
| Axillary lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
|
|
| Epitrochlear lymph nodes Epitrochlear lymph nodes Cubital Fossa: Anatomy | Medial side of the arm Arm The arm, or “upper arm” in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy below the elbow |
|
| Mediastinal lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
|
|
| Hilar lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes | Lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy | |
| Celiac lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
|
|
| Superior mesenteric lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
|
|
| Inferior mesenteric lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes | Colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy from splenic flexure Splenic flexure Small Intestine: Anatomy to upper rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy | |
| Paraaortic (lumbar) lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
|
|
| Iliac lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes (external and internal) |
|
|
| Inguinal lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes |
|
|
| Popliteal lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs nodes | Lower leg Leg The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy | Infection ( cellulitis Cellulitis Cellulitis is a common infection caused by bacteria that affects the dermis and subcutaneous tissue of the skin. It is frequently caused by Staphylococcus aureus and Streptococcus pyogenes. The skin infection presents as an erythematous and edematous area with warmth and tenderness. Cellulitis) |
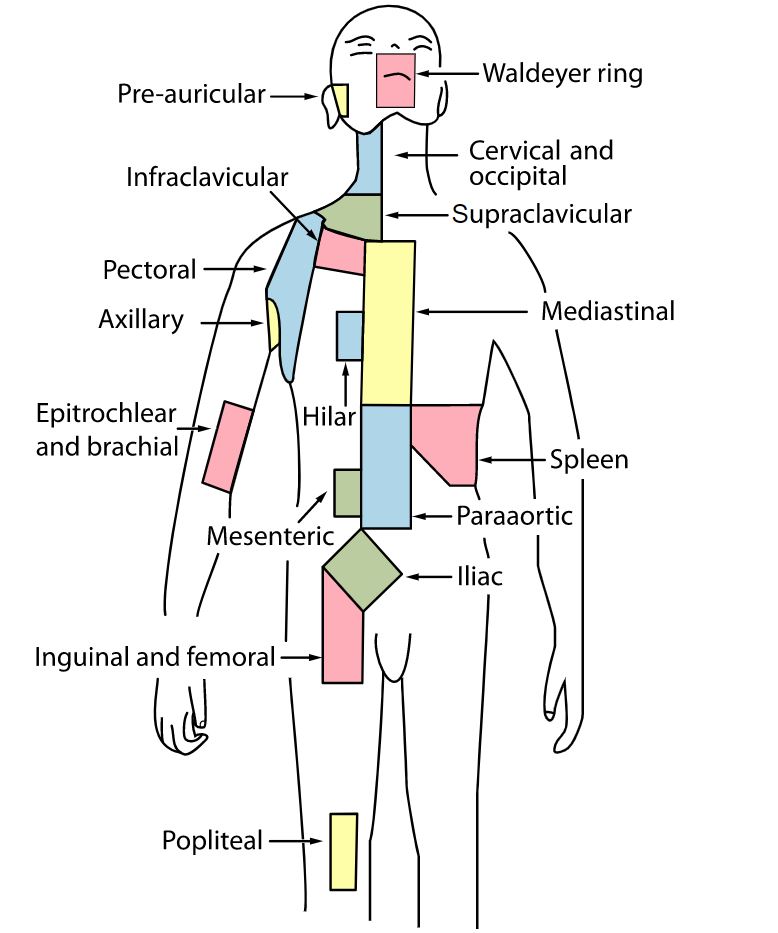
Lymph node regions indicating the clusters of lymph nodes
Image: “Lymph node regions” by Fred the Oyster and Mikael Häggström. License: Public Domain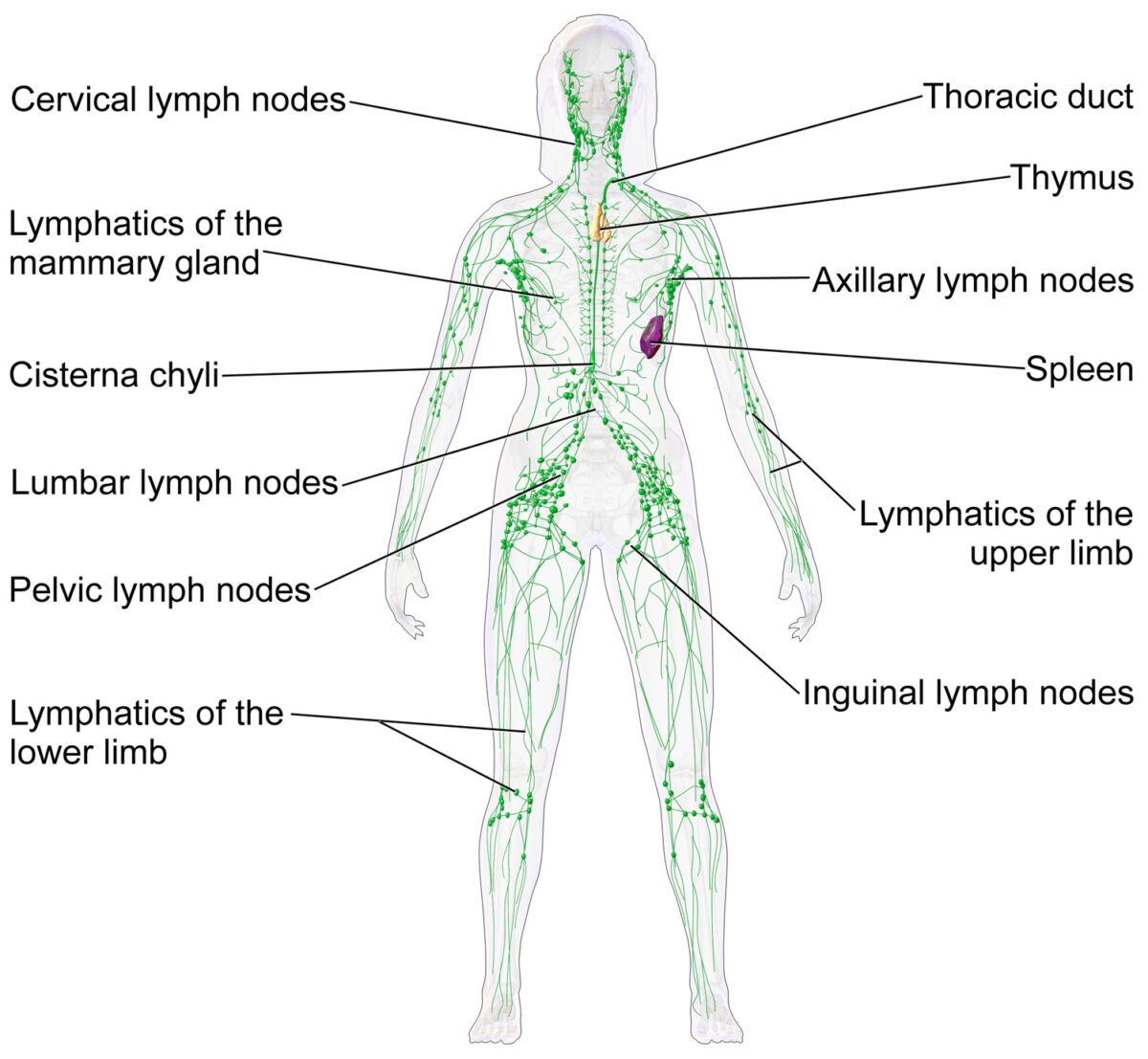
Lymph nodes and the lymphatic system
Image: “Blausen 0623 LymphaticSystem Female” by Blausen. License: CC BY 3.0