Chancroid is a highly transmissible STD caused by Haemophilus ducreyi Haemophilus ducreyi A species of Haemophilus that appears to be the pathogen or causative agent of the sexually transmitted disease, chancroid. Haemophilus. The disease presents with painful ulcer(s) on the genital tract (termed chancroid or “soft chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis”). Up to 50% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship will develop painful inguinal lymphadenopathy Inguinal Lymphadenopathy Lymphadenopathy. Furthermore, of that percentage, 25% may develop complications of the suppurative lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 - 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy. Given the growth of H. ducreyi on a special medium (often not readily available), chancroid is diagnosed based upon clinical appearance and tests to rule out both syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis and herpes (the most common causes of genital ulcers). Although the disease can resolve spontaneously, antibiotics ( azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides or ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins) are the treatment of choice. Treatment should involve both patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship and their sexual contacts.
Last updated: May 16, 2024
Chancroid (soft chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis) is a sexually transmitted disease Sexually Transmitted Disease Sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) caused by a bacterium, Haemophilus ducreyi Haemophilus ducreyi A species of Haemophilus that appears to be the pathogen or causative agent of the sexually transmitted disease, chancroid. Haemophilus, characterized by painful genital ulcers and suppurative inguinal adenopathy.

Chancroid: 1 cm (0.39 in) lesion on the glans of the penis confirmed to be from Haemophilus ducreyi
Image: “Chancroid lesion haemophilus ducreyi PHIL 3728 lores” by Joe Miller. License: Public Domain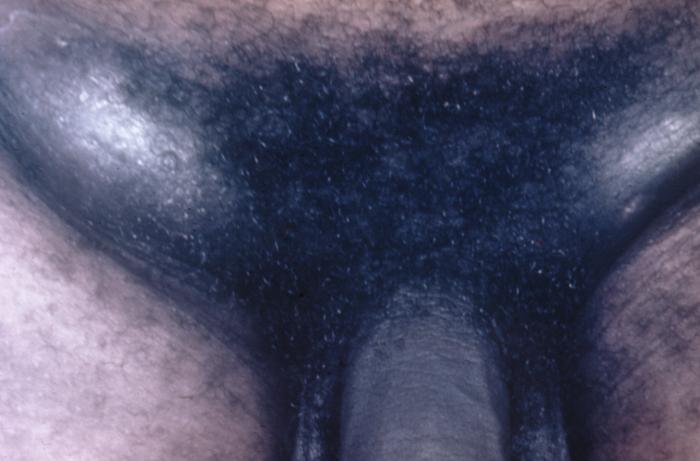
Inguinal lymphadenopathy:
lymph nodes in the groin, which in half of presented cases develop into buboes that can enlarge until they burst through the overlying skin.
Diagnosis is made by clinical judgment Judgment The process of discovering or asserting an objective or intrinsic relation between two objects or concepts; a faculty or power that enables a person to make judgments; the process of bringing to light and asserting the implicit meaning of a concept; a critical evaluation of a person or situation. Psychiatric Assessment and tests to rule out the 2 most common causes of genital ulcers, herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology ( HSV HSV Herpes simplex virus (HSV) is a double-stranded DNA virus belonging to the family Herpesviridae. Herpes simplex virus commonly causes recurrent infections involving the skin and mucosal surfaces, including the mouth, lips, eyes, and genitals. Herpes Simplex Virus 1 and 2) and syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis.

Haemophilus ducreyi bacteria
Image: “Haemophilus ducreyi 01” by CDC. License: Public Domain