Chlamydiae are obligate intracellular gram-negative bacteria gram-negative bacteria Bacteria which lose crystal violet stain but are stained pink when treated by gram's method. Bacteriology. They lack a peptidoglycan Peptidoglycan Penicillins layer and are best visualized using Giemsa stain Giemsa stain Borrelia. Chlamydiae species have a complex replication cycle consisting of 2 morphological forms: elementary bodies and reticulate bodies. The family of Chlamydiaceae comprises 3 pathogens that can infect humans: Chlamydia trachomatis, Chlamydia psittaci, and Chlamydia pneumoniae. C. trachomatis is the most common bacterium responsible for causing sexually transmitted diseases in the United States and is associated with urogenital infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, lymphogranuloma venereum Lymphogranuloma venereum Subacute inflammation of the inguinal lymph glands caused by certain immunotypes of Chlamydia trachomatis. It is a sexually transmitted disease in the U.S. But is more widespread in developing countries. It is distinguished from granuloma venereum, which is caused by calymmatobacterium granulomatis. Chlamydial Infections, neonatal conjunctivitis Conjunctivitis Conjunctivitis is a common inflammation of the bulbar and/or palpebral conjunctiva. It can be classified into infectious (mostly viral) and noninfectious conjunctivitis, which includes allergic causes. Patients commonly present with red eyes, increased tearing, burning, foreign body sensation, and photophobia. Conjunctivitis, and trachoma Trachoma A chronic infection of the conjunctiva and cornea caused by Chlamydia trachomatis. Chlamydial Infections. C. psittaci causes psittacosis (parrot fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever), whereas C. pneumoniae causes atypical pneumonia Atypical pneumonia Mycoplasma.
Last updated: Feb 3, 2025
Mnemonic
To help recall the characteristics of the life cycle, remember the 3 Es and 2 Rs:
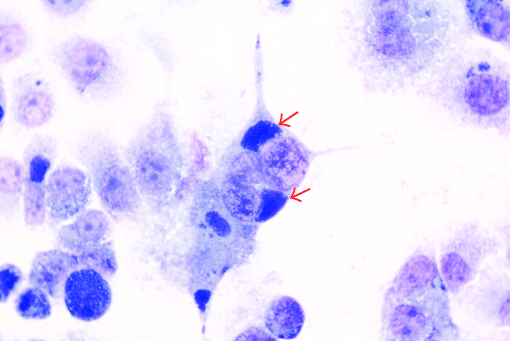
C. trachomatis: Perinuclear chlamydial inclusions (arrows) in a tissue culture of McCoy cells (a cell line originally derived from human synovial fluid) are seen on a Giemsa stain.
Image: “Perinuclear chlamydial inclusions (arrows) in McCoy cells when infected with the isolated strain” by Zhaocai Li, Xiaoan Cao, Baoquan Fu, Jizhang Zhou. License: CC BY 3.0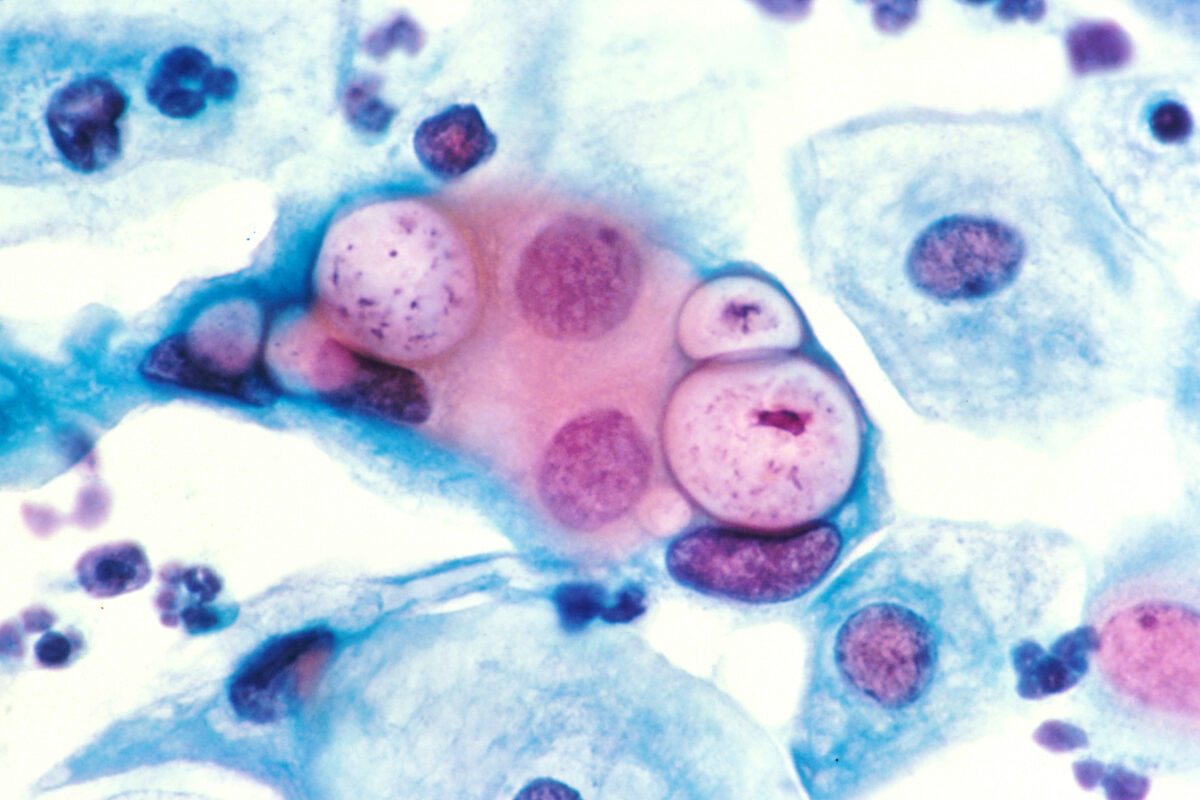
Papanicolaou stain of a cervicovaginal cytology preparation showing three chlamydial intranuclear inclusions within squamous epithelial cells that are next to several normal epithelial cells
Image: “Pap smear showing chlamydia in the vacuoles 500x H&E” by Dr. Lance Liotta Laboratory. License: Public Domain| C. trachomatis | C. psittaci | C. pneumoniae | |
|---|---|---|---|
| Host range | Humans primarily |
|
Humans only |
| Transmission |
|
Inhalation of contaminated, dried bird feces | Aerosolized droplets Droplets Varicella-Zoster Virus/Chickenpox |
| Risk factors |
|
Exposure to birds | Crowded settings (schools, nursing homes); the elderly are at higher risk for severe disease. |
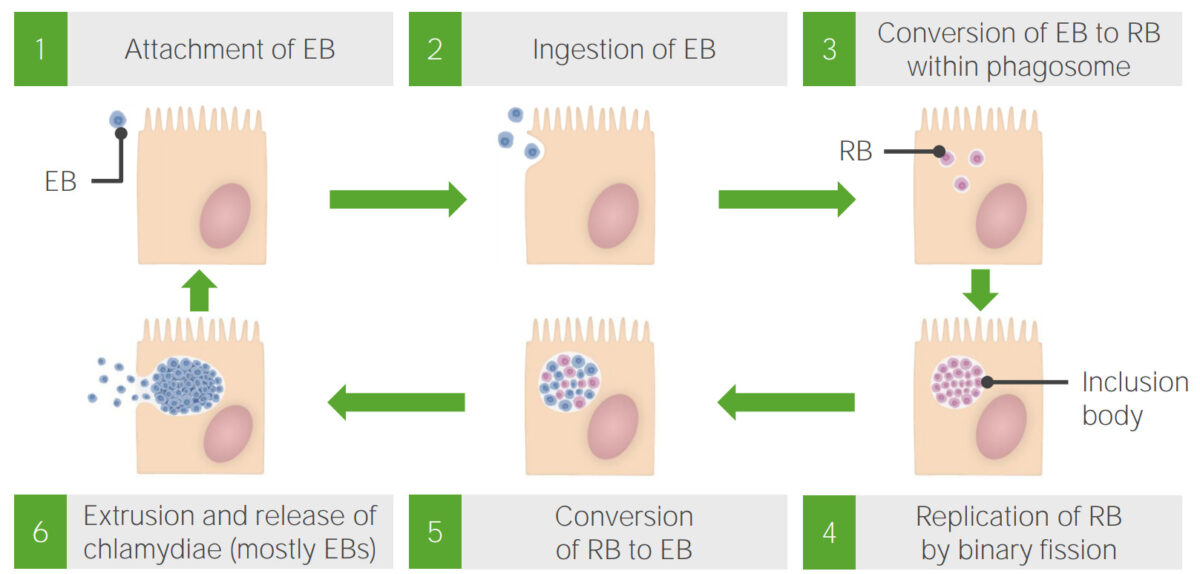
Growth cycle of chlamydiae:
Elementary bodies (EB) are ingested into the cell after attaching to its surface and are then converted into the reticulocyte body (RB) form. As RBs begin to replicate, they create a cluster known as an inclusion body. After replication terminates, the inclusion bodies release EB forms, which leave the cell.
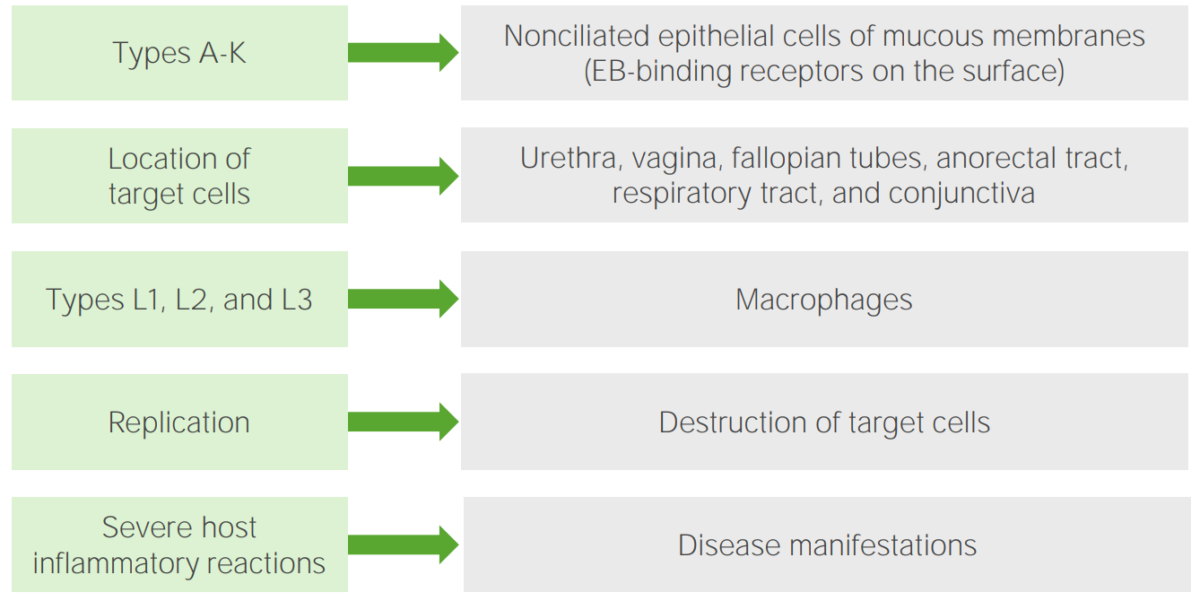
Pathogenesis of Chlamydia trachomatis
Image by Lecturio.Sexually transmitted:
Neonatal infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease (serovars D–K):
Trachoma Trachoma A chronic infection of the conjunctiva and cornea caused by Chlamydia trachomatis. Chlamydial Infections (serovars A–C):
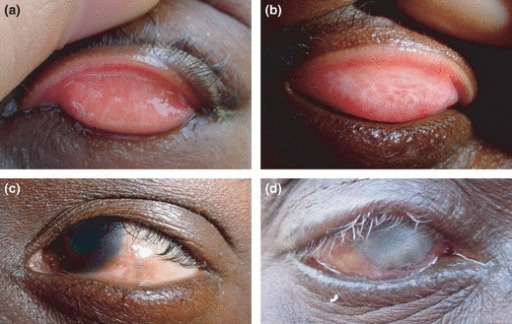
Trachoma
Recurrent episodes of infection with serovars A–C of Chlamydia trachomatis cause conjunctival inflammation in children, who eventually develop scarring and blindness as adults.

Lymphogranuloma venereum caused by the invasive serovars L1, L2, or L3 of Chlamydia trachomatis. This young adult experienced an acute onset of tender, enlarged lymph nodes in both groins.
Image: “Lymphogranuloma venerum – lymph nodes” by Herbert L. Fred, Hendrik A. van Dijk. License: CC BY 2.0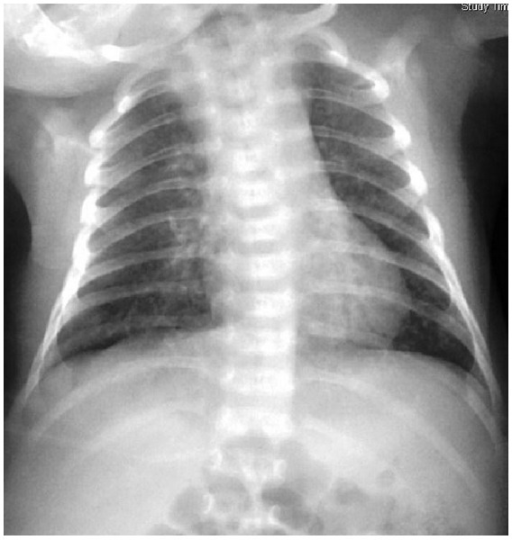
Chlamydia trachomatis neonatal pneumonia: diffuse patchiness on a chest radiogram.
Image: “Chlamydial pneumonitis: a creepy neonatal disease” by Hon KL, Leung AK. License: CC BY 3.0