The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor Pelvic floor Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum Sacrum Five fused vertebrae forming a triangle-shaped structure at the back of the pelvis. It articulates superiorly with the lumbar vertebrae, inferiorly with the coccyx, and anteriorly with the ilium of the pelvis. The sacrum strengthens and stabilizes the pelvis. Vertebral Column: Anatomy, is a ring-like bony structure of the axial Axial Computed Tomography (CT) skeleton that links the vertebral column Vertebral column The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy with the lower extremities. The pelvic ring joints include the pubic symphysis Pubic Symphysis A slightly movable cartilaginous joint which occurs between the pubic bones. Vagina, Vulva, and Pelvic Floor: Anatomy anteriorly and the sacroiliac joints posteriorly. The hip bones are made up of 3 fused bones: the pubis, ischium, and ilium. The pelvic cavity houses various GI, urinary, and reproductive structures, which are supported by the muscles and connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology of the pelvic floor Pelvic floor Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy. The female pelvis, making accommodations for childbirth, is generally wider and larger than the male pelvis.
Last updated: Nov 18, 2024
The pelvis is a ring-like structure that surrounds and protects the pelvic cavity. The pelvis is composed of the following bones:
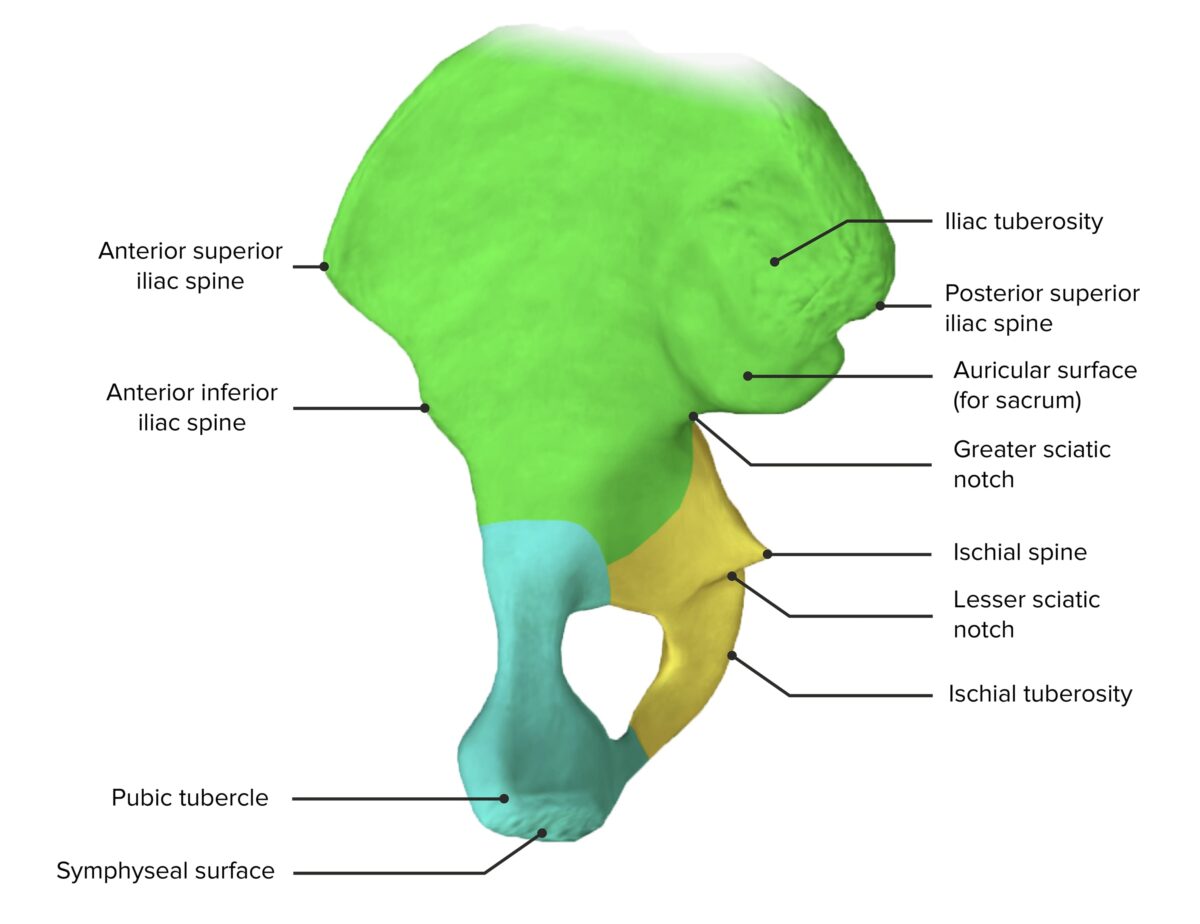
Medial view of the hip bone, featuring its components: the ilium (green), ischium (yellow), and pubis (blue)
Image by BioDigital, edited by Lecturio.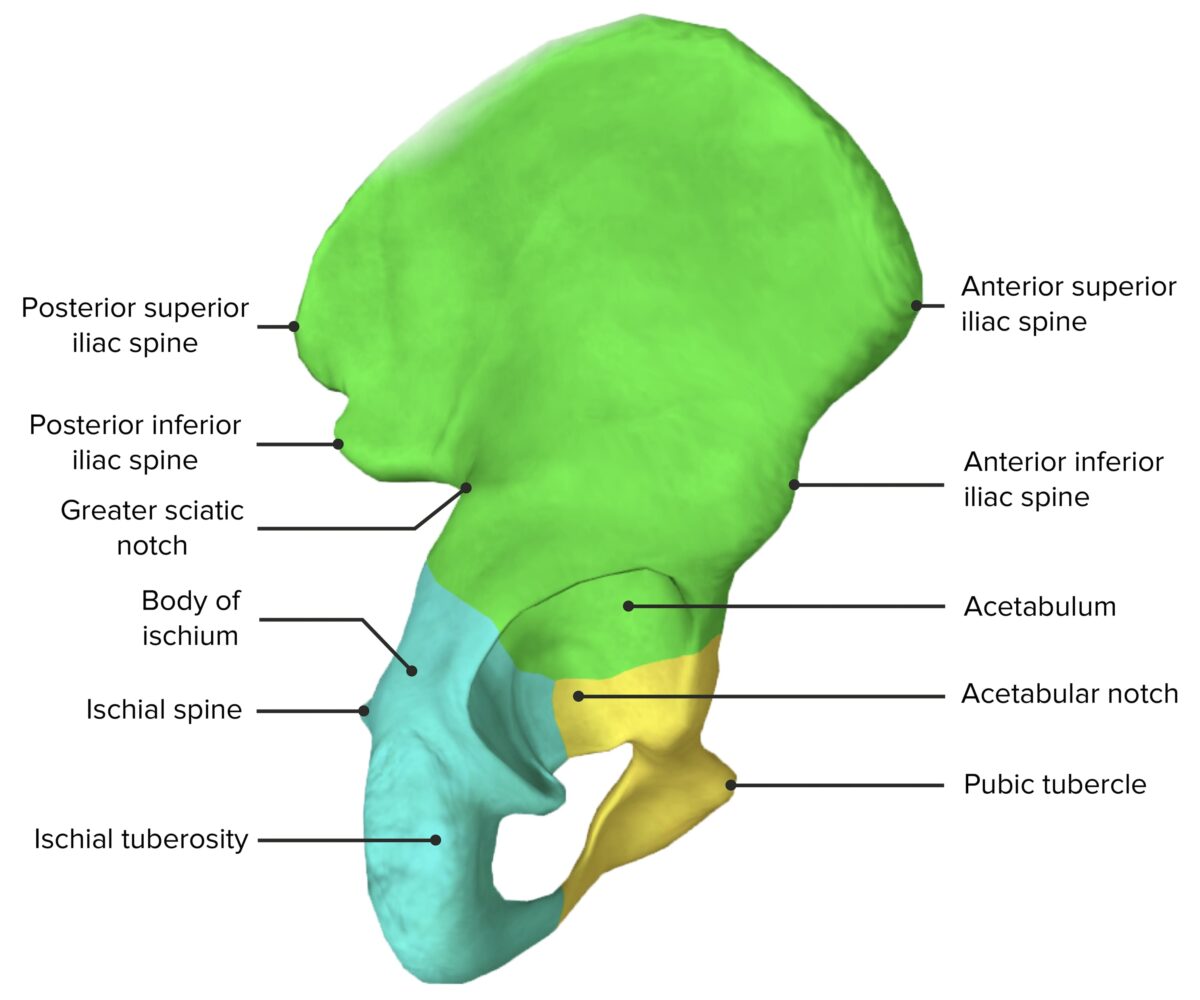
Lateral view of the hip bone, featuring its components: the ilium (green), ischium (yellow), and pubis (blue)
Image by BioDigital, edited by Lecturio.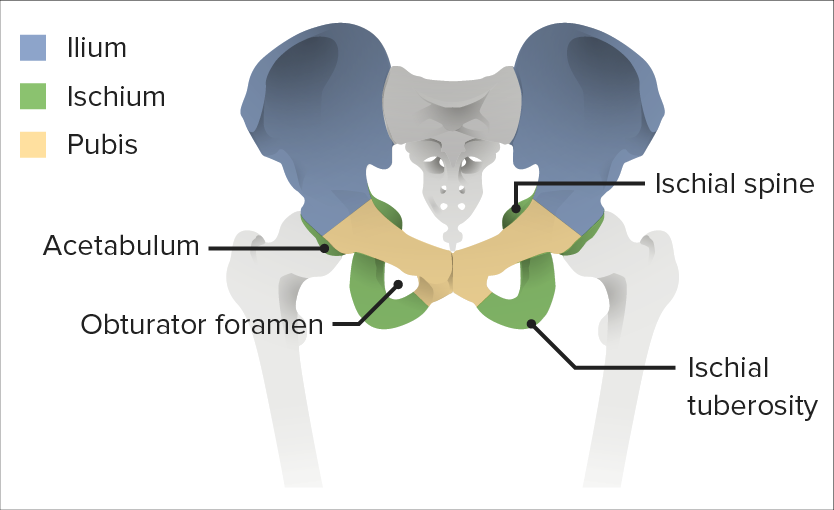
The 3 components of the hip bone
Image by Lecturio.There are 4 primary joints within the pelvis:
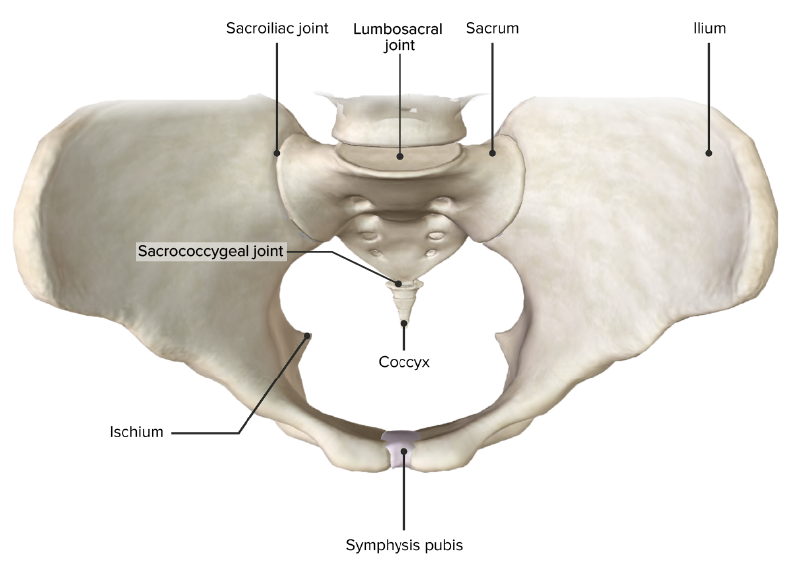
Superior view of the pelvic girdle, featuring the 4 primary joints of the pelvis
Image by BioDigital, edited by Lecturio.The bony pelvis is primarily stabilized by the following ligaments:
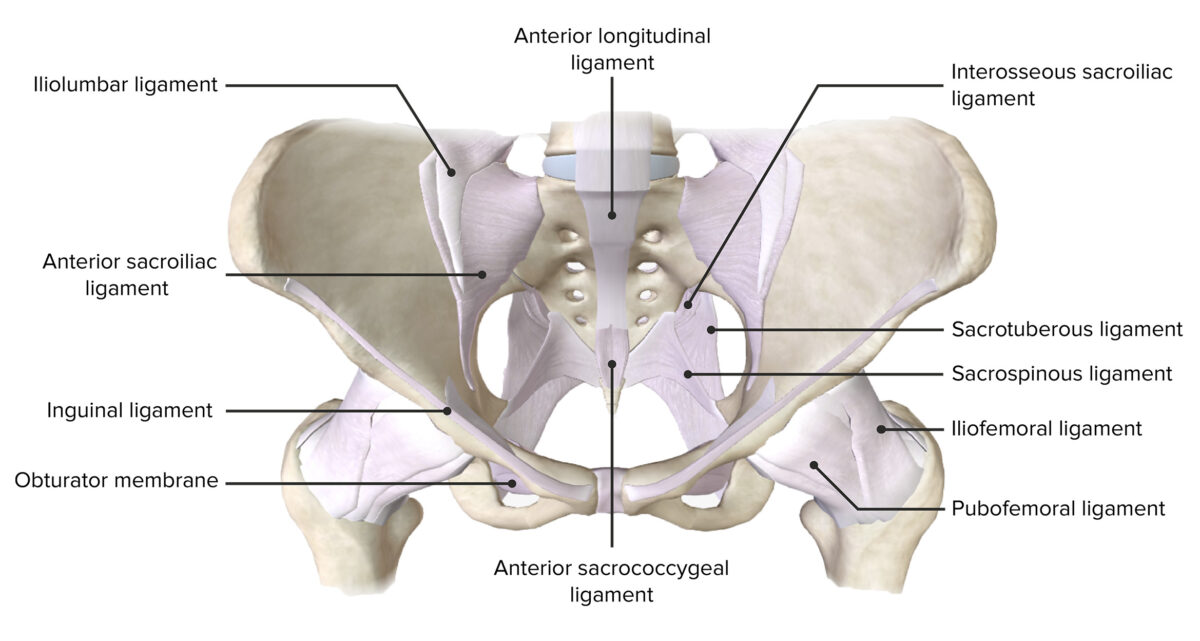
Anterior view of the pelvis, featuring the supporting ligaments of the joints of the pelvic girdle
Image by BioDigital, edited by Lecturio.The pelvic cavity is bound by the bones of the pelvic girdle and primarily contains reproductive organs, urinary organs, and the rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy. As the peritoneal cavity Peritoneal Cavity The space enclosed by the peritoneum. It is divided into two portions, the greater sac and the lesser sac or omental bursa, which lies behind the stomach. The two sacs are connected by the foramen of winslow, or epiploic foramen. Peritoneum: Anatomy rests in the pelvic cavity, spaces from this region are also considered to be part of the space of the pelvic cavity. By using bony landmarks and ligaments, the pelvis can be divided into various openings, foramina, and spaces.
| Location | Boundaries | Contents | |
|---|---|---|---|
| Pelvic inlet | Superior pelvic aperture |
|
|
| Pelvic outlet | Inferior pelvic aperture |
|
Terminal parts of the excretory, reproductive, and digestive systems |
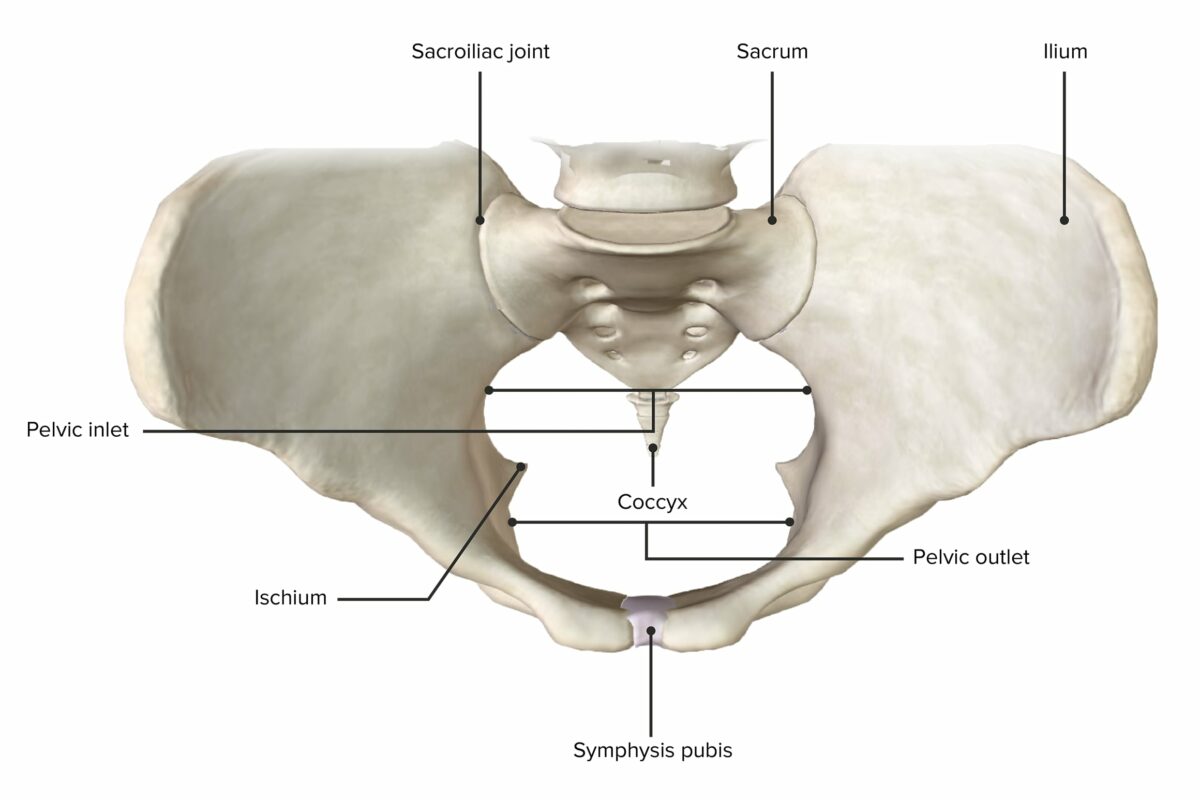
Superior view of the pelvic girdle, depicting the widest horizontal diameter of the pelvic inlet and the pelvic outlet
Image by BioDigital, edited by Lecturio.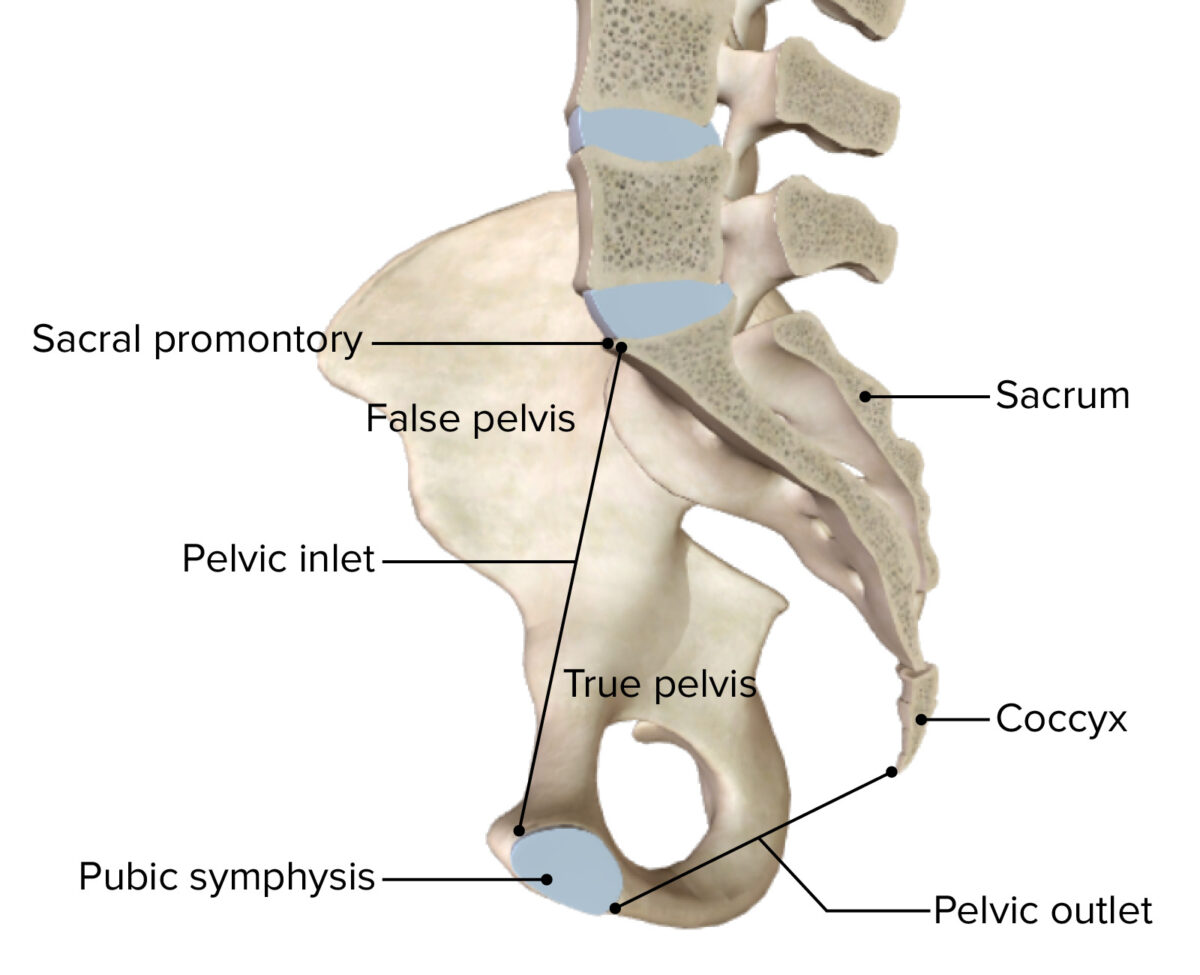
Sagittal cross section of the bony pelvis
Image by BioDigital, edited by Lecturio.| Structure | Boundaries | Contents | |
|---|---|---|---|
| Greater sciatic foramen | Formed by:
|
|
|
| Lesser sciatic foramen |
|
|
|
| Obturator foramen |
|
|
|
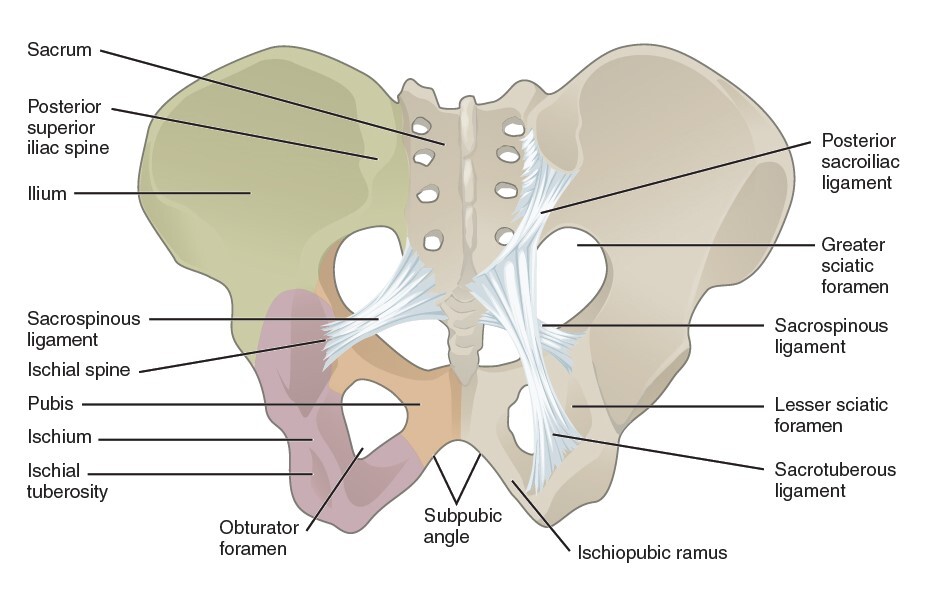
Ligaments of the pelvis:
Anterior view of the pelvis, featuring the greater and lesser sciatic foramina and the obturator foramen
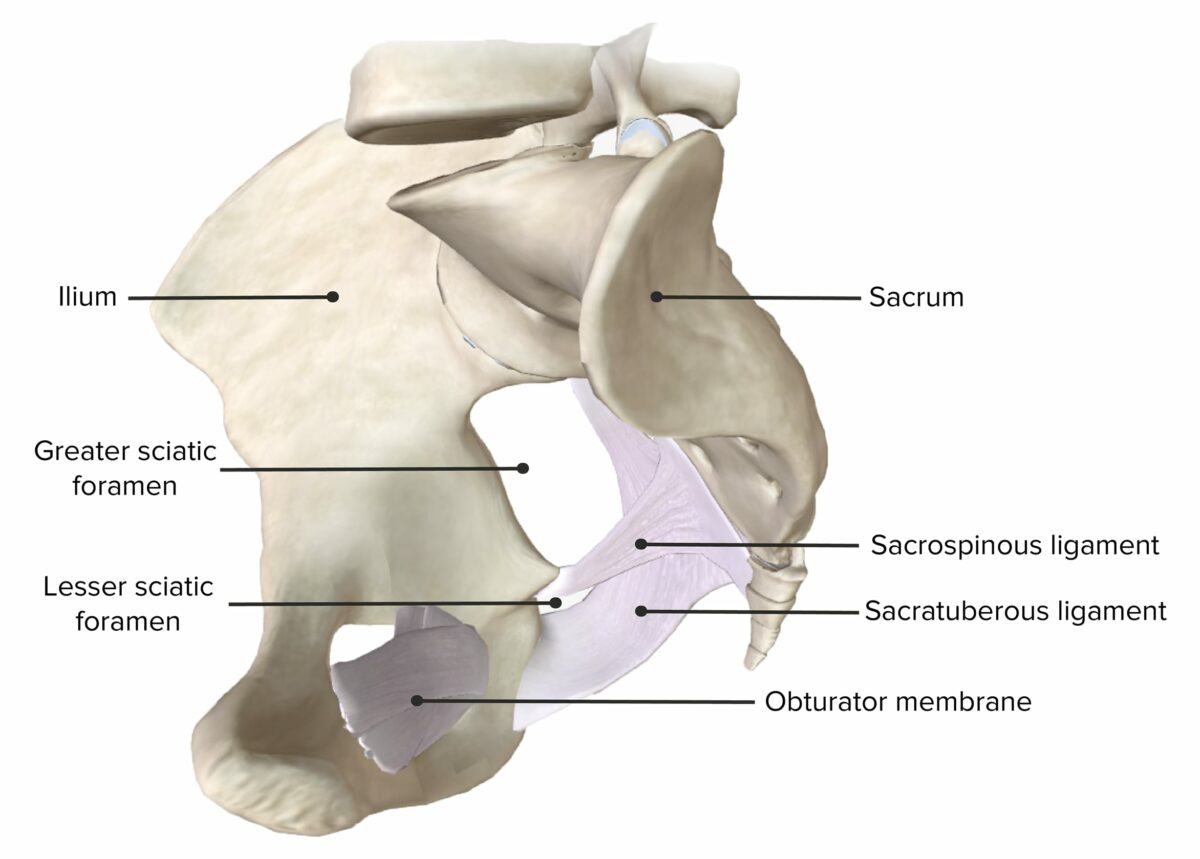
Lateral view of the hemipelvis, featuring the greater and lesser sciatic foramina
Image by BioDigital, edited by Lecturio.The pelvis has multiple spaces related to the caudal end of the peritoneal cavity Peritoneal Cavity The space enclosed by the peritoneum. It is divided into two portions, the greater sac and the lesser sac or omental bursa, which lies behind the stomach. The two sacs are connected by the foramen of winslow, or epiploic foramen. Peritoneum: Anatomy and the peritoneal folds Peritoneal Folds Peritoneum: Anatomy found within the viscera:
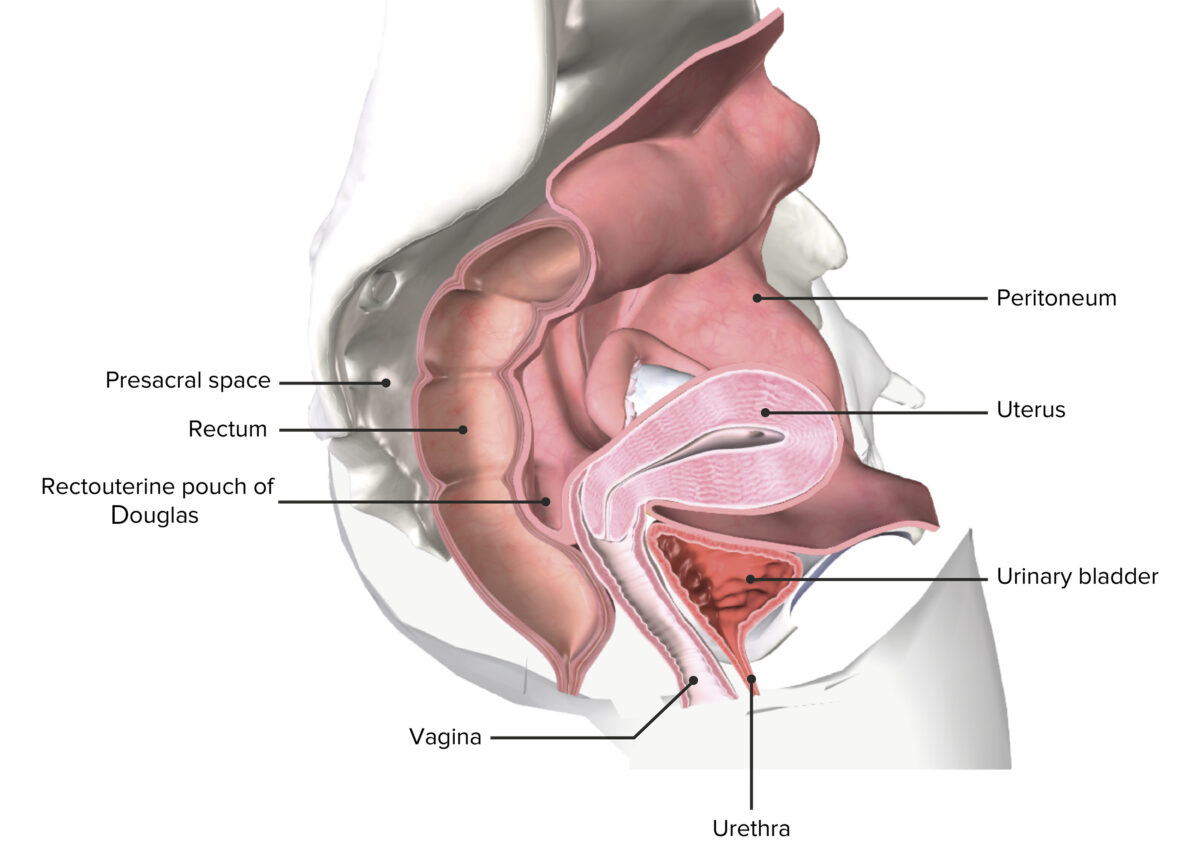
Bacia feminina seccionada que representa o útero in situ
Imagem por BioDigital, editada por Lecturio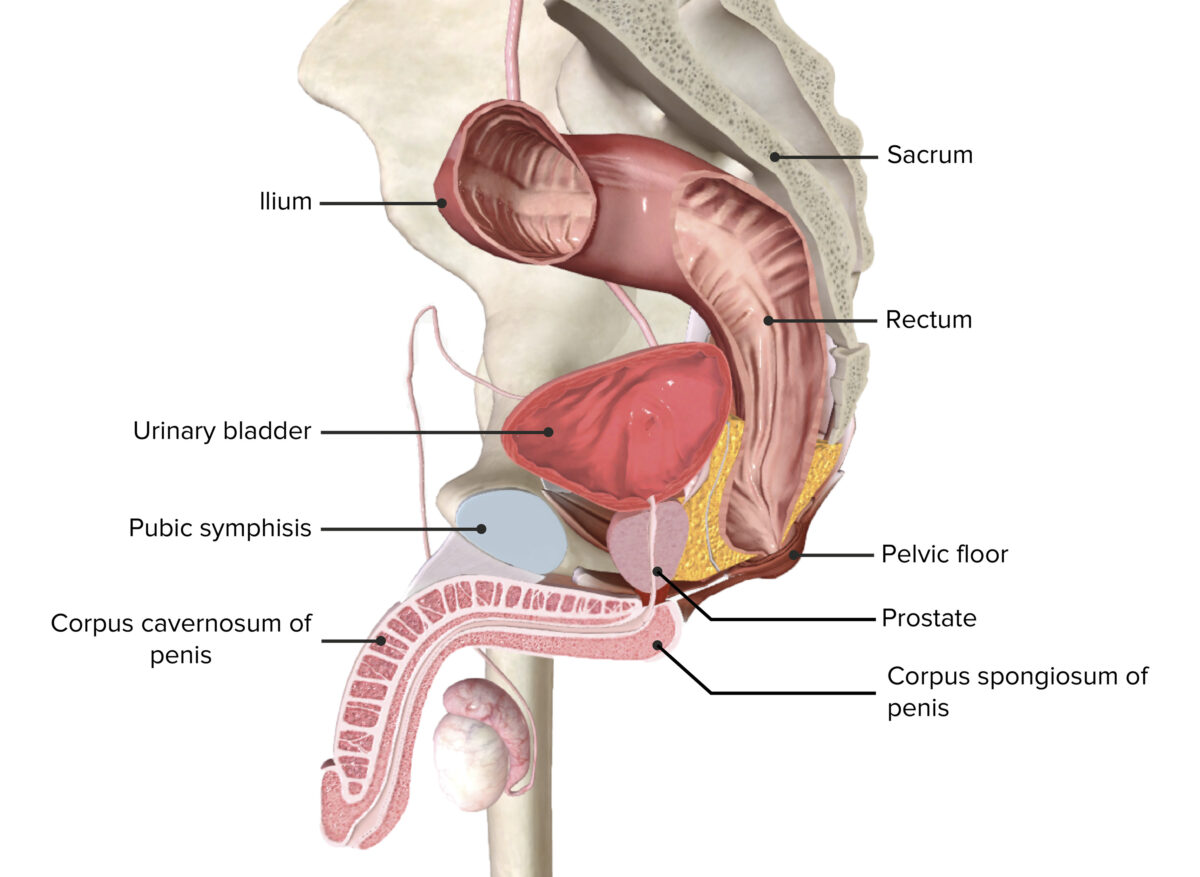
Espaços peritoneais dentro da bacia masculina
Imagem por BioDigital, editada por LecturioThere are anatomical variations between the female (gynecoid) and male (android) pelvis.
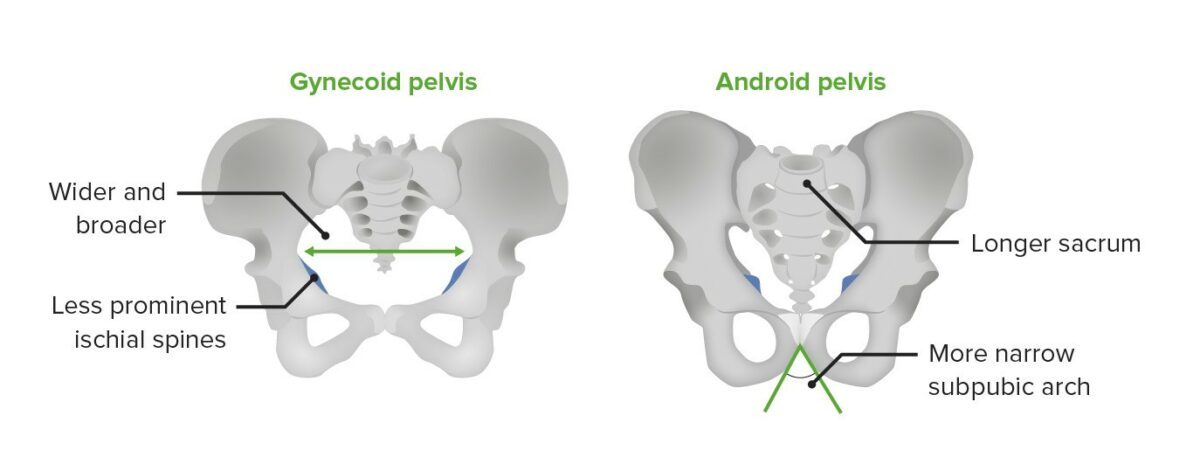
The gynecoid pelvis versus the android pelvis
Image by Lecturio.The pelvic floor Pelvic floor Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy, also referred to as the pelvic diaphragm Pelvic diaphragm Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy, is a group of muscles that supports the abdominal and pelvic viscera. The pelvic floor Pelvic floor Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy has 3 layers:
| Superficial layer: perineum Perineum The body region lying between the genital area and the anus on the surface of the trunk, and to the shallow compartment lying deep to this area that is inferior to the pelvic diaphragm. The surface area is between the vulva and the anus in the female, and between the scrotum and the anus in the male. Vagina, Vulva, and Pelvic Floor: Anatomy | Intermediate layer: pelvic diaphragm Pelvic diaphragm Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy | Deep layer: urogenital diaphragm Urogenital diaphragm Vagina, Vulva, and Pelvic Floor: Anatomy | |
|---|---|---|---|
| Characteristics | Diamond-shaped surface region between coccyx Coccyx The last bone in the vertebral column in tailless primates considered to be a vestigial tail-bone consisting of three to five fused vertebrae. Vertebral Column: Anatomy and pubic symphysis Pubic Symphysis A slightly movable cartilaginous joint which occurs between the pubic bones. Vagina, Vulva, and Pelvic Floor: Anatomy | Separates the perineum Perineum The body region lying between the genital area and the anus on the surface of the trunk, and to the shallow compartment lying deep to this area that is inferior to the pelvic diaphragm. The surface area is between the vulva and the anus in the female, and between the scrotum and the anus in the male. Vagina, Vulva, and Pelvic Floor: Anatomy from the pelvic cavity | Separates the upper pelvis from the deep perineal sac |
| Components |
|
|
|
| Innervation | Pudendal nerve Pudendal nerve A nerve which originates in the sacral spinal cord (s2 to s4) and innervates the perineum, the external genitalia, the external anal sphincter and the external urethral sphincter. It has three major branches: the perineal nerve, inferior anal nerves, and the dorsal nerve of penis or clitoris. Gluteal Region: Anatomy | Sacral nerve roots ( S3 S3 Heart Sounds–S5) | Pudendal nerve Pudendal nerve A nerve which originates in the sacral spinal cord (s2 to s4) and innervates the perineum, the external genitalia, the external anal sphincter and the external urethral sphincter. It has three major branches: the perineal nerve, inferior anal nerves, and the dorsal nerve of penis or clitoris. Gluteal Region: Anatomy |
| Function | Support and raise the pelvic floor Pelvic floor Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy | ||
The muscles of the pelvic floor Pelvic floor Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy have several important functions:
| Layer | Muscle | Origin | Insertion |
|---|---|---|---|
| Perineum Perineum The body region lying between the genital area and the anus on the surface of the trunk, and to the shallow compartment lying deep to this area that is inferior to the pelvic diaphragm. The surface area is between the vulva and the anus in the female, and between the scrotum and the anus in the male. Vagina, Vulva, and Pelvic Floor: Anatomy | Ischiocavernosus | Ischial tuberosity Ischial Tuberosity Chronic Apophyseal Injury | Crus penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy |
| Bulbocavernosus/bulbospongiosus (females/males) | Central tendinous median raphe Raphe Testicles: Anatomy of the perineum Perineum The body region lying between the genital area and the anus on the surface of the trunk, and to the shallow compartment lying deep to this area that is inferior to the pelvic diaphragm. The surface area is between the vulva and the anus in the female, and between the scrotum and the anus in the male. Vagina, Vulva, and Pelvic Floor: Anatomy | Superficial perineal membrane and dorsal penile/clitoral aponeurosis | |
| Superficial transverse perineal | Ischial tuberosity Ischial Tuberosity Chronic Apophyseal Injury | Transverse perineal muscle of the contralateral side | |
| External anal sphincter External anal sphincter Rectum and Anal Canal: Anatomy | 2 flattened muscular planes encircle the anus and meet in front to insert into the perineal body. | ||
| Pelvic diaphragm Pelvic diaphragm Soft tissue formed mainly by the pelvic diaphragm, which is composed of the two levator ani and two coccygeus muscles. The pelvic diaphragm lies just below the pelvic aperture (outlet) and separates the pelvic cavity from the perineum. It extends between the pubic bone anteriorly and the coccyx posteriorly. Vagina, Vulva, and Pelvic Floor: Anatomy | Levator ani group: puborectalis Puborectalis Vagina, Vulva, and Pelvic Floor: Anatomy, pubococcygeus Pubococcygeus Vagina, Vulva, and Pelvic Floor: Anatomy, and iliococcygeus Iliococcygeus Vagina, Vulva, and Pelvic Floor: Anatomy | Puborectalis Puborectalis Vagina, Vulva, and Pelvic Floor: Anatomy: body of the pubis (passes around the lower rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy) | Puborectalis Puborectalis Vagina, Vulva, and Pelvic Floor: Anatomy: meets its counterpart muscle at midline |
| Pubococcygeus Pubococcygeus Vagina, Vulva, and Pelvic Floor: Anatomy: body of the pubis and anterior tendinous arch | Pubococcygeus Pubococcygeus Vagina, Vulva, and Pelvic Floor: Anatomy: coccyx Coccyx The last bone in the vertebral column in tailless primates considered to be a vestigial tail-bone consisting of three to five fused vertebrae. Vertebral Column: Anatomy and anococcygeal ligaments | ||
| Iliococcygeus Iliococcygeus Vagina, Vulva, and Pelvic Floor: Anatomy: ischial spines and posterior tendinous arch | Iliococcygeus Iliococcygeus Vagina, Vulva, and Pelvic Floor: Anatomy: coccyx Coccyx The last bone in the vertebral column in tailless primates considered to be a vestigial tail-bone consisting of three to five fused vertebrae. Vertebral Column: Anatomy and anococcygeal ligaments | ||
| Coccygeus Coccygeus Vagina, Vulva, and Pelvic Floor: Anatomy | Ischial spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy and sacrospinous ligament | Lower sacrum Sacrum Five fused vertebrae forming a triangle-shaped structure at the back of the pelvis. It articulates superiorly with the lumbar vertebrae, inferiorly with the coccyx, and anteriorly with the ilium of the pelvis. The sacrum strengthens and stabilizes the pelvis. Vertebral Column: Anatomy and coccyx Coccyx The last bone in the vertebral column in tailless primates considered to be a vestigial tail-bone consisting of three to five fused vertebrae. Vertebral Column: Anatomy | |
| Piriformis Piriformis Vagina, Vulva, and Pelvic Floor: Anatomy | Anterior sacrum Sacrum Five fused vertebrae forming a triangle-shaped structure at the back of the pelvis. It articulates superiorly with the lumbar vertebrae, inferiorly with the coccyx, and anteriorly with the ilium of the pelvis. The sacrum strengthens and stabilizes the pelvis. Vertebral Column: Anatomy and superior margin of greater sciatic notch | Greater trochanter | |
| Obturator internus Obturator internus Vagina, Vulva, and Pelvic Floor: Anatomy | Ischiopubic rami and obturator membrane | Medial aspect of the greater trochanter | |
| Urogenital diaphragm Urogenital diaphragm Vagina, Vulva, and Pelvic Floor: Anatomy | Deep transverse perineal | Inferior ischial rami | Contralateral counterpart |
| Urethral sphincter | Internal urethral sphincter: inferior bladder Bladder A musculomembranous sac along the urinary tract. Urine flows from the kidneys into the bladder via the ureters, and is held there until urination. Pyelonephritis and Perinephric Abscess to the proximal urethra Urethra A tube that transports urine from the urinary bladder to the outside of the body in both the sexes. It also has a reproductive function in the male by providing a passage for sperm. Urinary Tract: Anatomy ( extension Extension Examination of the Upper Limbs of detrusor muscle Detrusor muscle Urinary Incontinence) | ||
| External urethral sphincter: ischiopubic ramus towards the median plane, where it attaches with its counterpart muscle | |||
| Compressor urethrae muscle | Originates from inferior pubic ramus and wraps anteriorly around the urethra Urethra A tube that transports urine from the urinary bladder to the outside of the body in both the sexes. It also has a reproductive function in the male by providing a passage for sperm. Urinary Tract: Anatomy to merge with its counterpart | ||
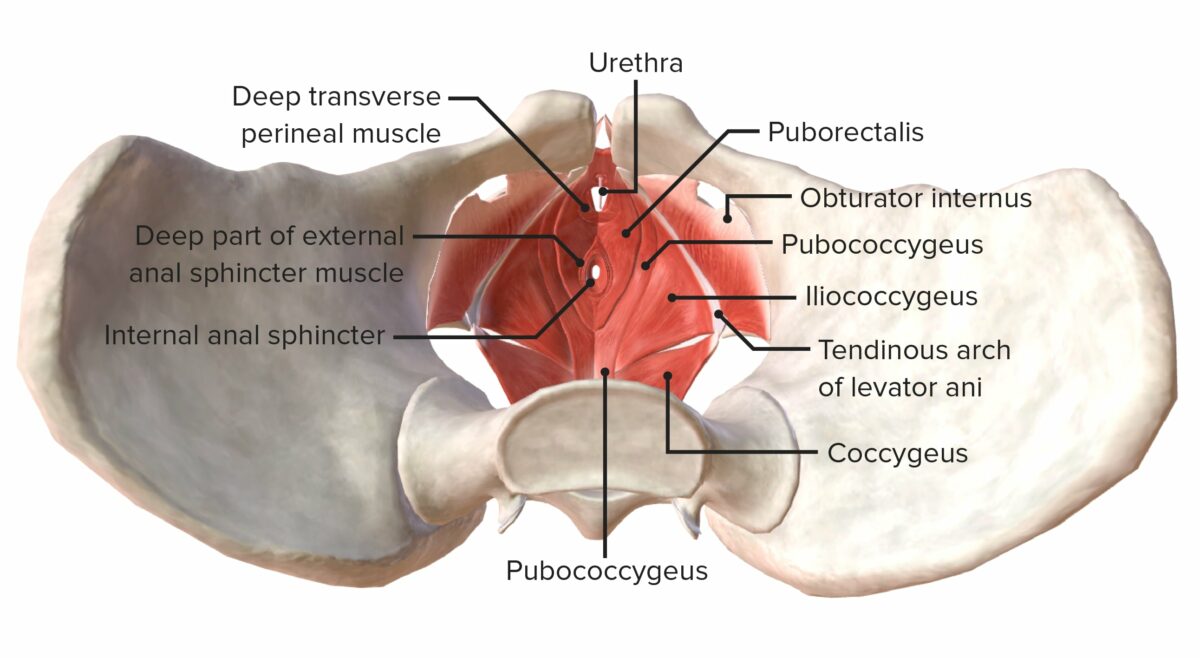
Muscles of the pelvic floor from a superior view
Image by BioDigital, edited by Lecturio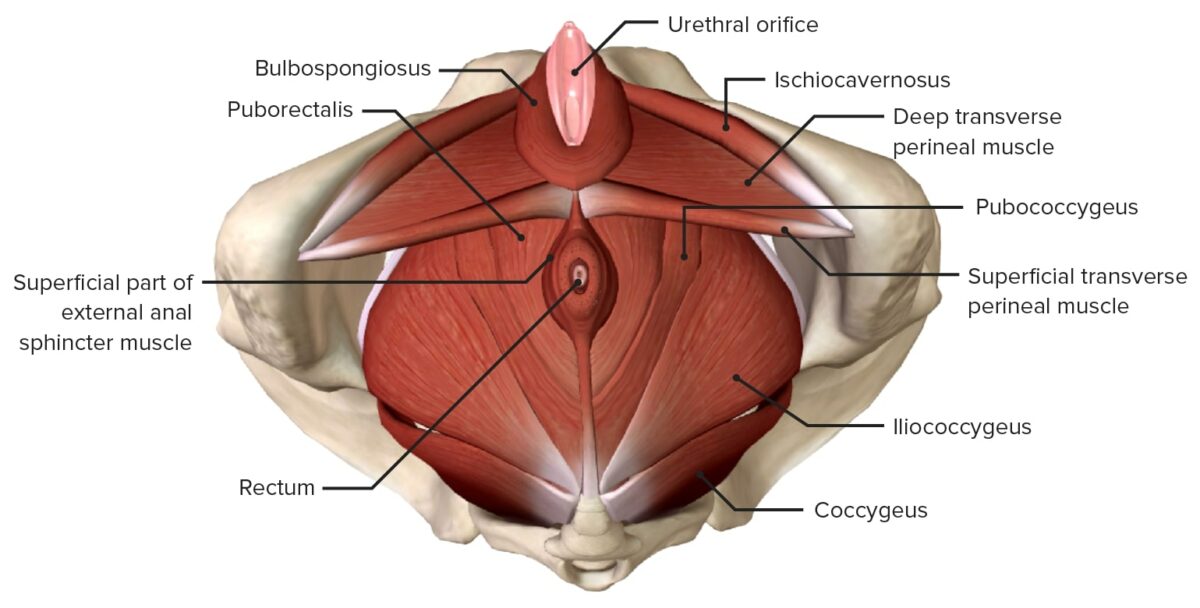
Muscles of the pelvic floor from an inferior view
Image by BioDigital, edited by LecturioBlood to the pelvis is supplied by:
The 3 main veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology of the pelvis follow the course of the arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology and are named accordingly:
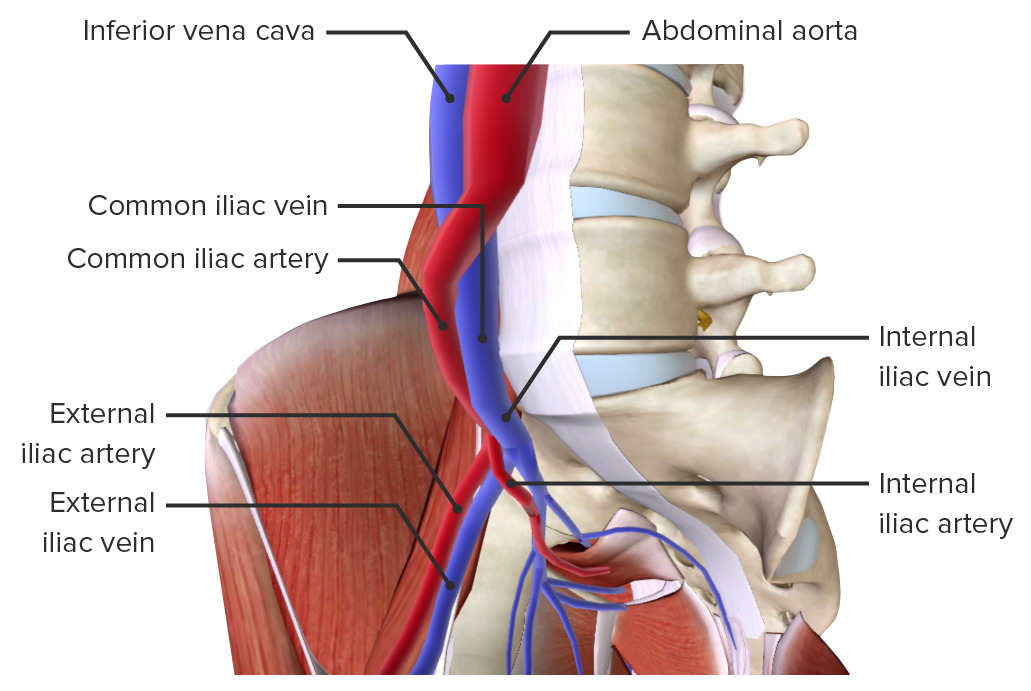
Arteries and veins of the pelvis
Image by BioDigital, edited by LecturioThe innervation of the pelvis is provided by branches from the sacral plexus, including the pudendal nerve Pudendal nerve A nerve which originates in the sacral spinal cord (s2 to s4) and innervates the perineum, the external genitalia, the external anal sphincter and the external urethral sphincter. It has three major branches: the perineal nerve, inferior anal nerves, and the dorsal nerve of penis or clitoris. Gluteal Region: Anatomy, which is formed from the sacral plexus, S2 S2 Heart Sounds– S4 S4 Heart Sounds. The pelvis receives both somatic and autonomic innervation.
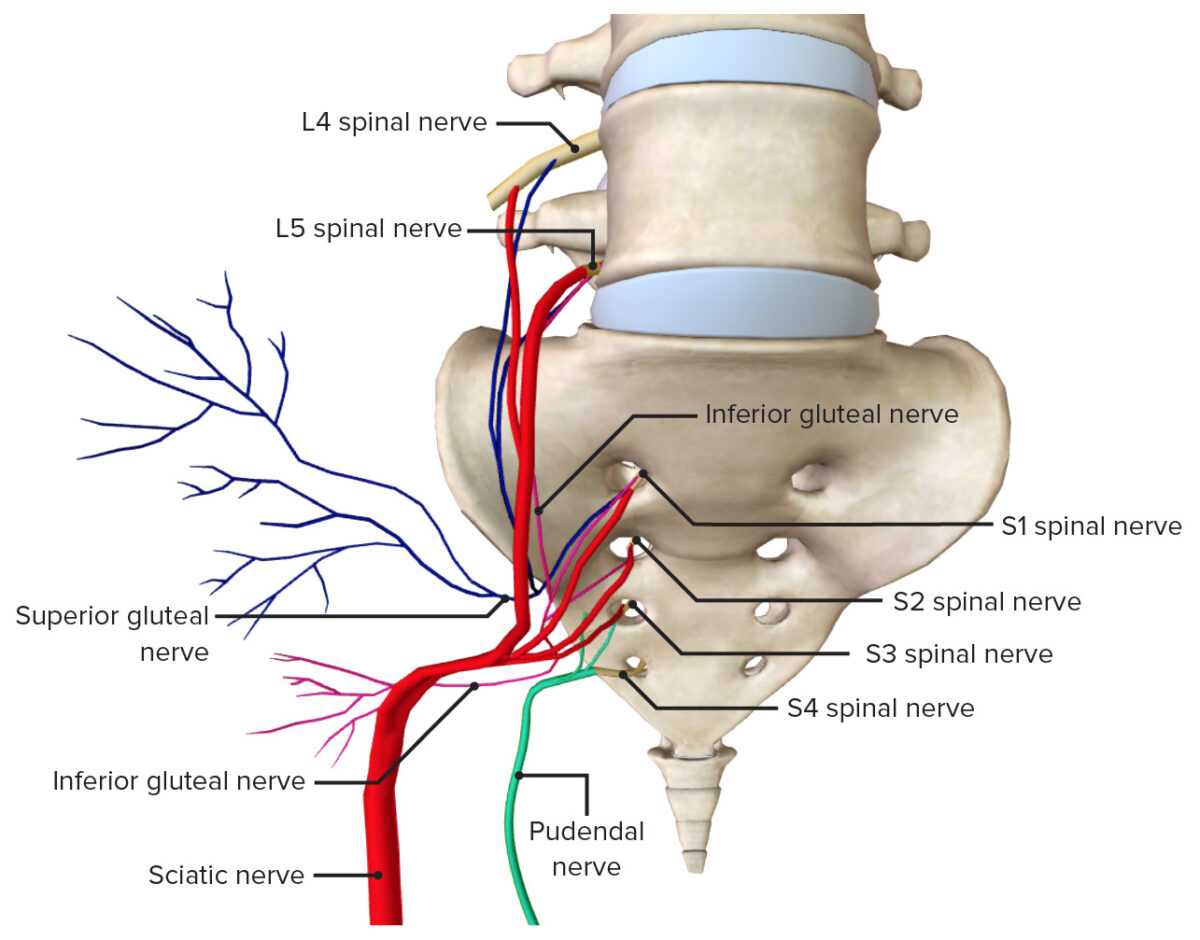
Nerves of the pelvis
Image by BioDigital, edited by Lecturio