The jaw is made up of the mandible, which comprises the lower jaw, and the maxilla Maxilla One of a pair of irregularly shaped bones that form the upper jaw. A maxillary bone provides tooth sockets for the superior teeth, forms part of the orbit, and contains the maxillary sinus. Skull: Anatomy, which comprises the upper jaw Upper jaw One of a pair of irregularly shaped bones that form the upper jaw. A maxillary bone provides tooth sockets for the superior teeth, forms part of the orbit, and contains the maxillary sinus. Skull: Anatomy. The mandible articulates with the temporal bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types via the temporomandibular joint (TMJ). The 4 muscles of mastication produce the movements of the TMJ to ensure the efficient chewing of food. Blood is supplied to this region by the external carotid system, and the TMJ is primarily innervated by branches of the trigeminal nerve Trigeminal nerve The 5th and largest cranial nerve. The trigeminal nerve is a mixed motor and sensory nerve. The larger sensory part forms the ophthalmic, mandibular, and maxillary nerves which carry afferents sensitive to external or internal stimuli from the skin, muscles, and joints of the face and mouth and from the teeth. Most of these fibers originate from cells of the trigeminal ganglion and project to the trigeminal nucleus of the brain stem. The smaller motor part arises from the brain stem trigeminal motor nucleus and innervates the muscles of mastication. The 12 Cranial Nerves: Overview and Functions.
Last updated: Nov 19, 2024
The pharyngeal arches Pharyngeal arches The branchial arches, also known as pharyngeal or visceral arches, are embryonic structures seen in the development of vertebrates that serve as precursors for many structures of the face, neck, and head. These arches are composed of a central core of mesoderm, which is covered externally by ectoderm and internally by endoderm. Branchial Apparatus and Aortic Arches are embryonic structures that serve as precursors for many structures of the face, neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess, and head. The arches are composed of mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation and neural crest cells Neural crest cells Gastrulation and Neurulation and are accompanied externally by ectoderm Ectoderm The outer of the three germ layers of an embryo. Gastrulation and Neurulation and internally by endoderm Endoderm The inner of the three germ layers of an embryo. Gastrulation and Neurulation.
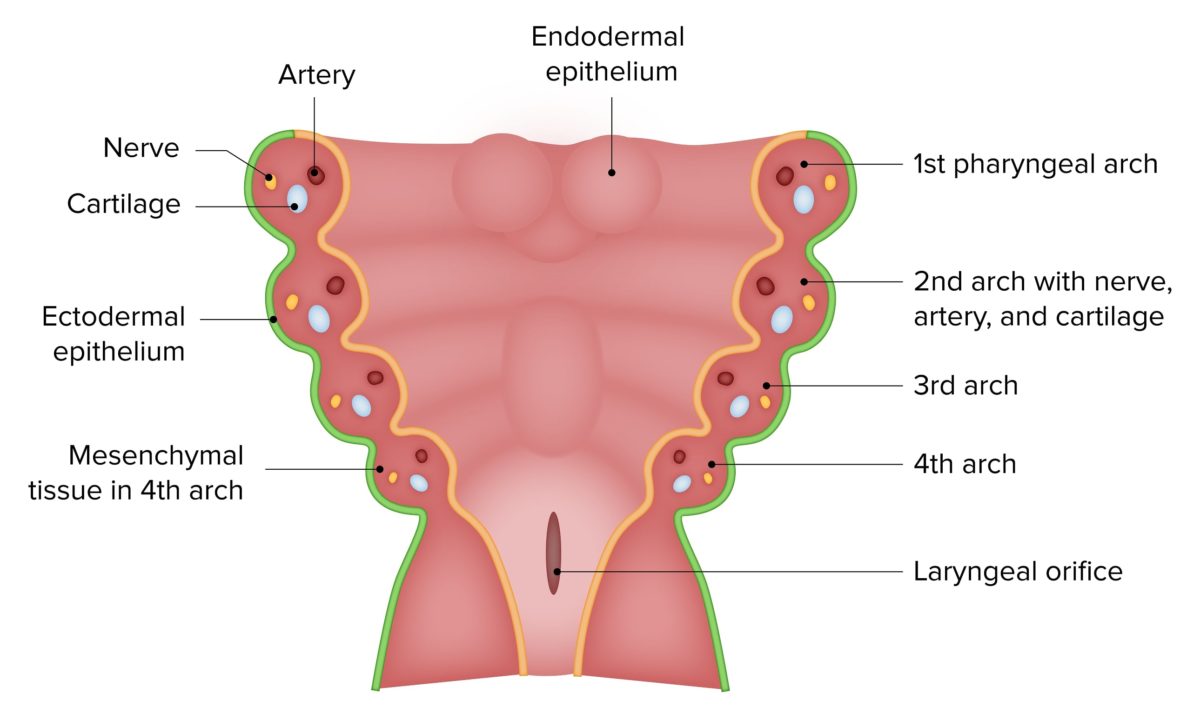
The first pharyngeal arch is the most cephalad of the six pharyngeal arches.
Image by Lecturio.The jaw consists of 3 bones: the maxilla Maxilla One of a pair of irregularly shaped bones that form the upper jaw. A maxillary bone provides tooth sockets for the superior teeth, forms part of the orbit, and contains the maxillary sinus. Skull: Anatomy, the mandible, and the temporal bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types.
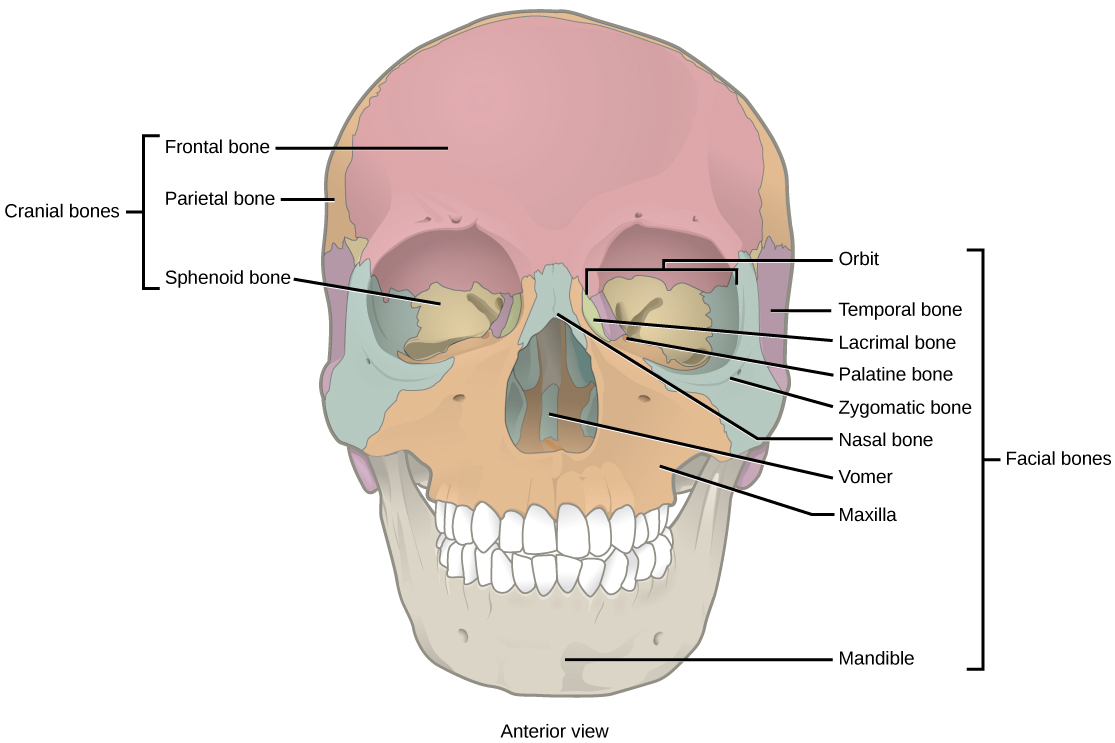
Anterior view of the skull:
Note the locations of the maxilla, the mandible, and the temporal bone.
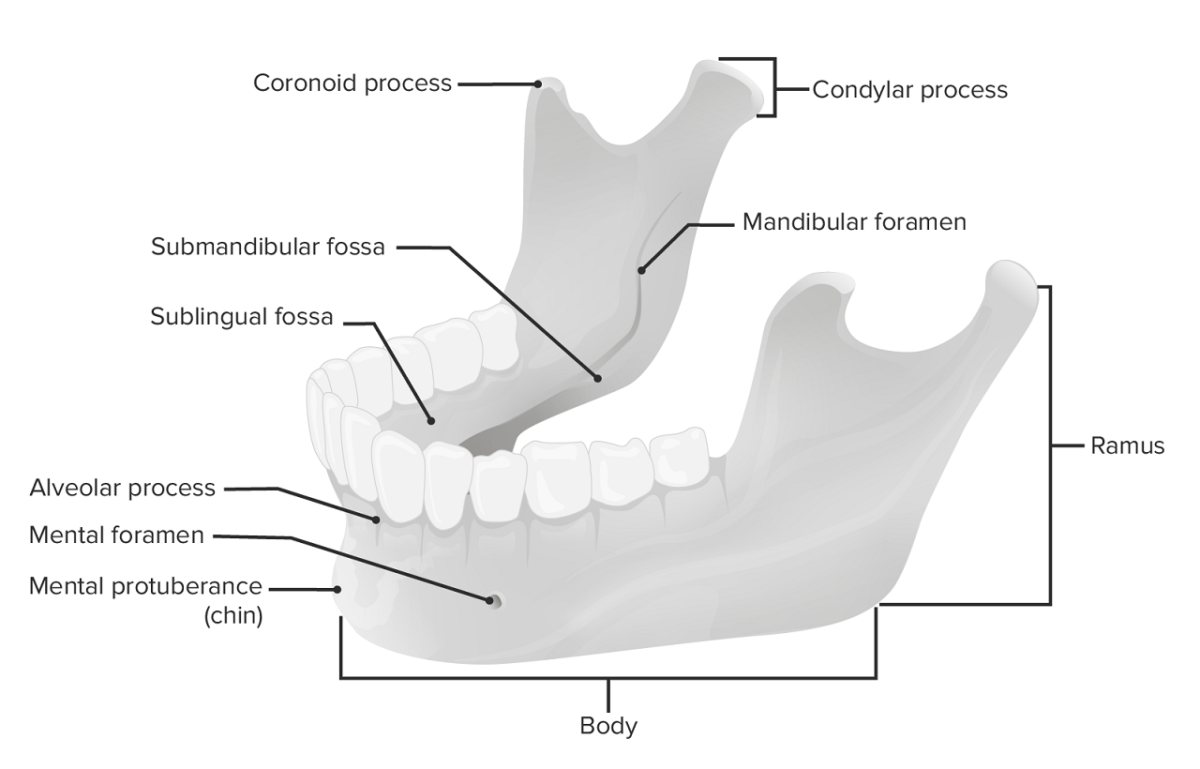
The mandible
Image by Lecturio.The mandibular fossa is the articular surface in which the condylar process of the ramus of the mandible articulates with the skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy, forming the TMJ.
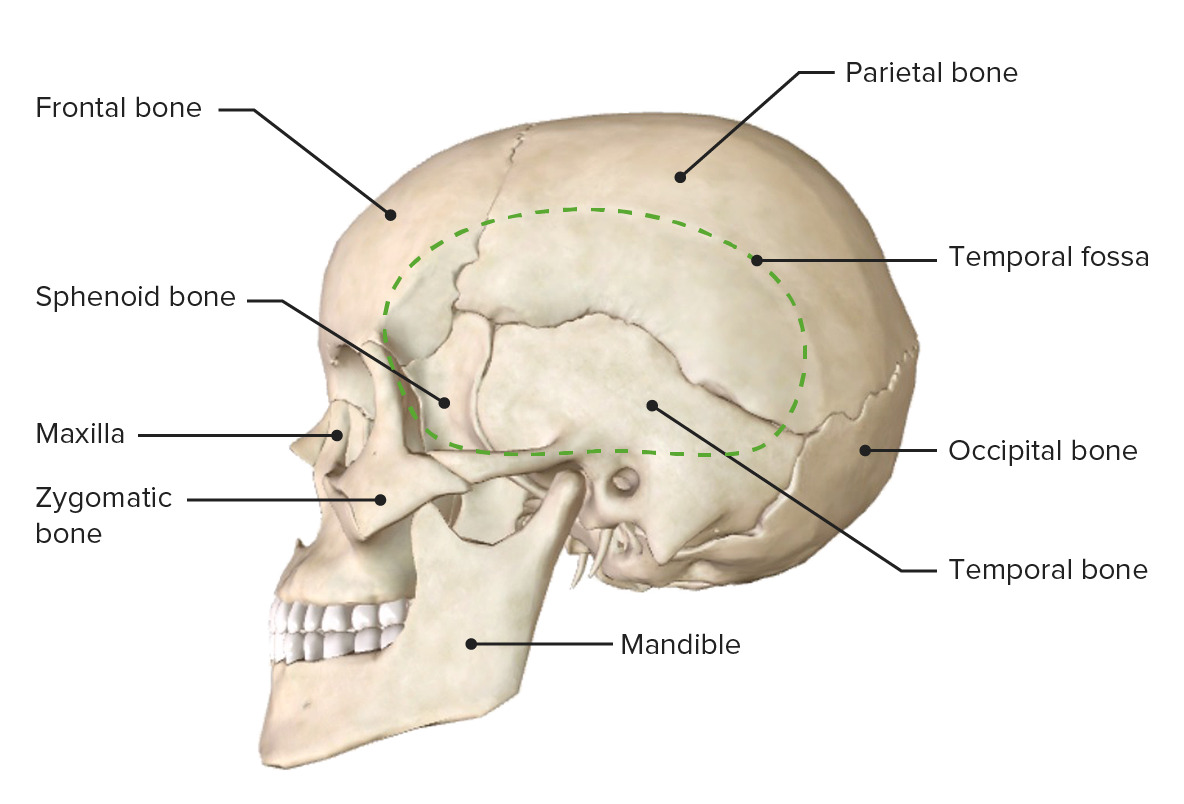
Lateral view of the skull
Image: “Lateral view of the skull” by OpenStax College. License: CC BY 3.0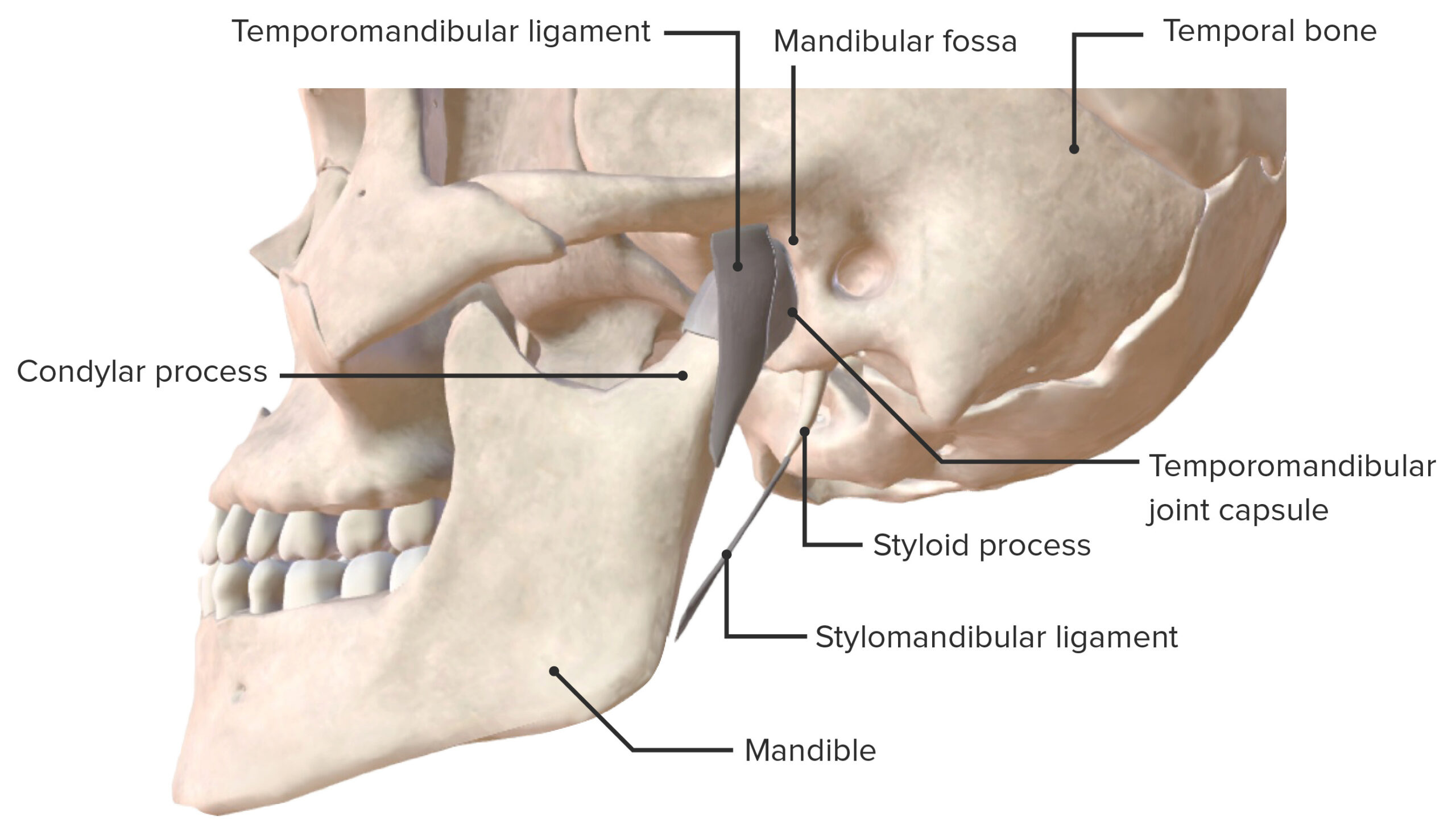
Lateral view of the temporomandibular joint and supporting ligaments
Image by BioDigital, edited by Lecturio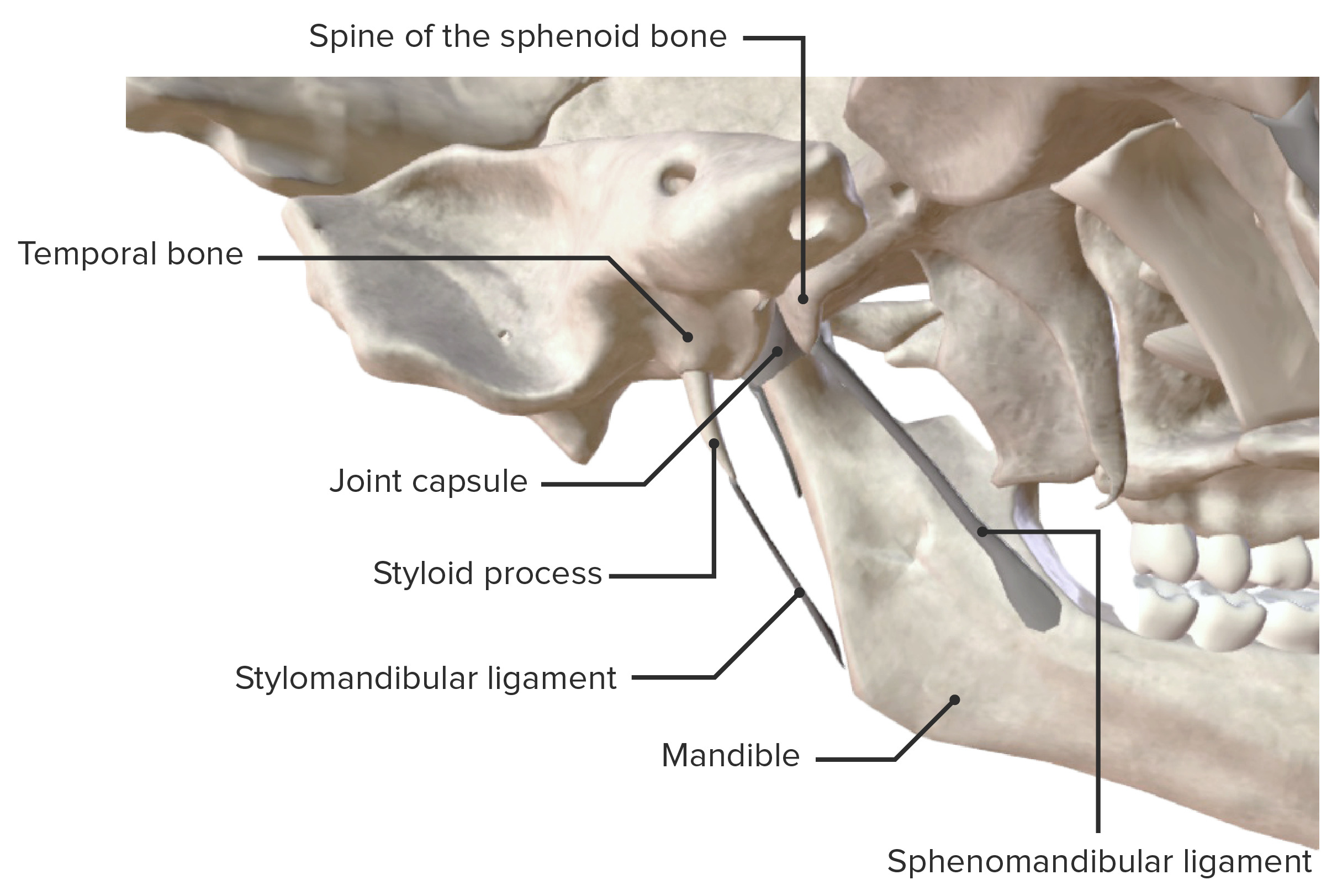
Medial view of the temporomandibular joint and supporting ligaments
Image by BioDigital, edited by Lecturio| Muscle | Origin | Insertion | Nerve supply | Function |
|---|---|---|---|---|
| Temporalis | Broad origin from the floor of the temporal fossa Temporal fossa Skull: Anatomy | Coronoid process and anterior border of the ramus of the mandible | Branches of the mandibular division of the trigeminal nerve Trigeminal nerve The 5th and largest cranial nerve. The trigeminal nerve is a mixed motor and sensory nerve. The larger sensory part forms the ophthalmic, mandibular, and maxillary nerves which carry afferents sensitive to external or internal stimuli from the skin, muscles, and joints of the face and mouth and from the teeth. Most of these fibers originate from cells of the trigeminal ganglion and project to the trigeminal nucleus of the brain stem. The smaller motor part arises from the brain stem trigeminal motor nucleus and innervates the muscles of mastication. The 12 Cranial Nerves: Overview and Functions (due to their common origin: mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation of 1st pharyngeal arch) | Elevates and retracts the mandible |
| Masseter | Medial surface of the maxillary process of the zygomatic bone Zygomatic bone Either of a pair of bones that form the prominent part of the cheek and contribute to the orbit on each side of the skull. Orbit and Extraocular Muscles: Anatomy and zygomatic Zygomatic Either of a pair of bones that form the prominent part of the cheek and contribute to the orbit on each side of the skull. Skull: Anatomy arch | Angle and lateral surface of ramus of the mandible | Elevates the mandible | |
| Lateral pterygoid | Infratemporal surface and crest of the greater wing and lateral plate of the pterygoid process of the sphenoid | Pterygoid fossa of the mandible |
|
|
| Medial pterygoid |
|
Medial surface of the ramus of the mandible, inferior to the mandibular foramen |
|
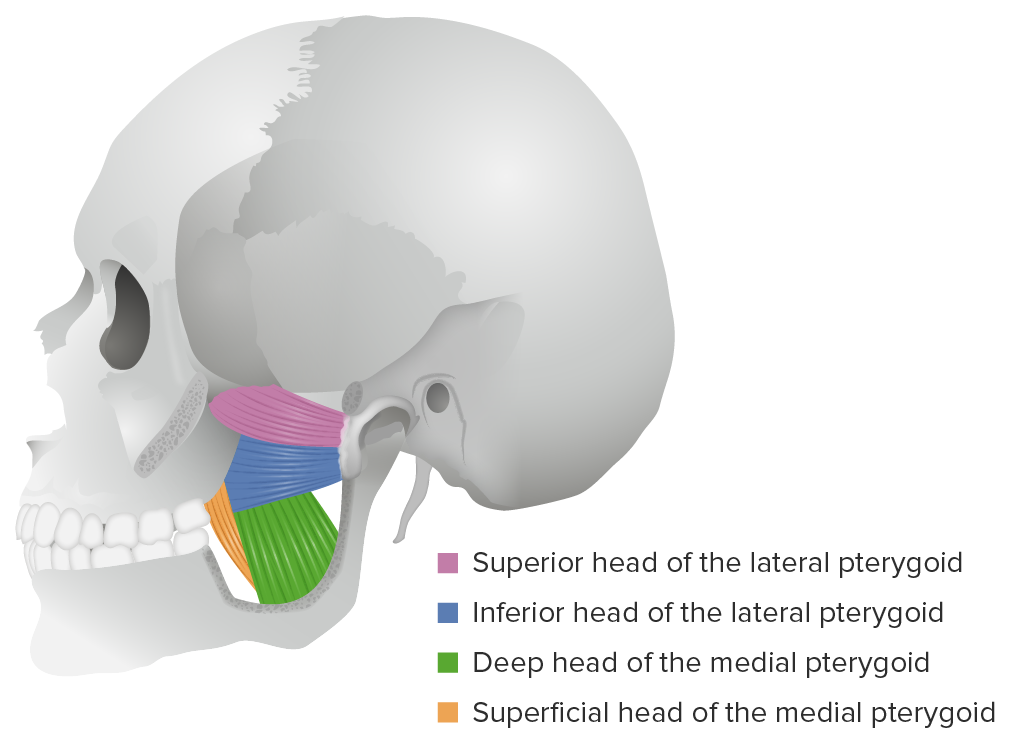
Lateral view of the lateral and medial pterygoid muscles
Image by Lecturio. License: CC BY-NC-SA 4.0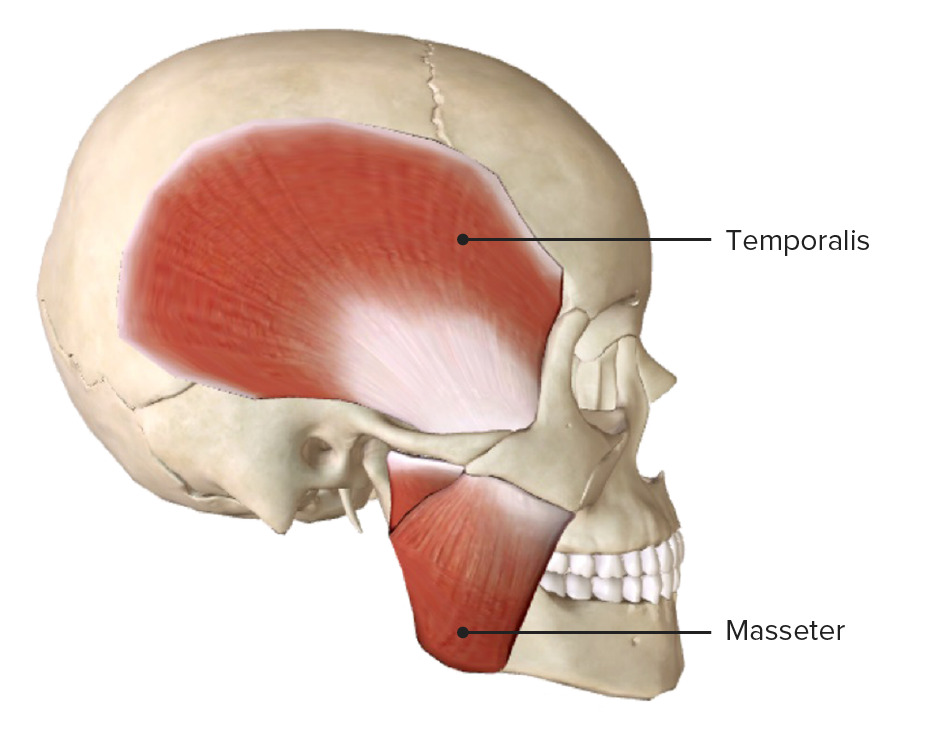
Lateral view of the skull, featuring the temporalis and masseter muscles
Image by BioDigital, edited by Lecturio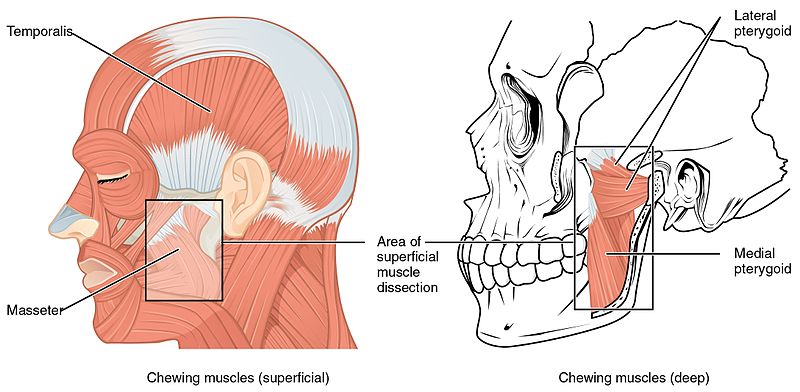
Lateral view of the head, featuring the muscles of mastication:
Note that the masseter and temporalis muscles are superficial, while the lateral and medial pterygoid muscles are on a deeper muscular layer in direct relation with the temporomandibular joint.
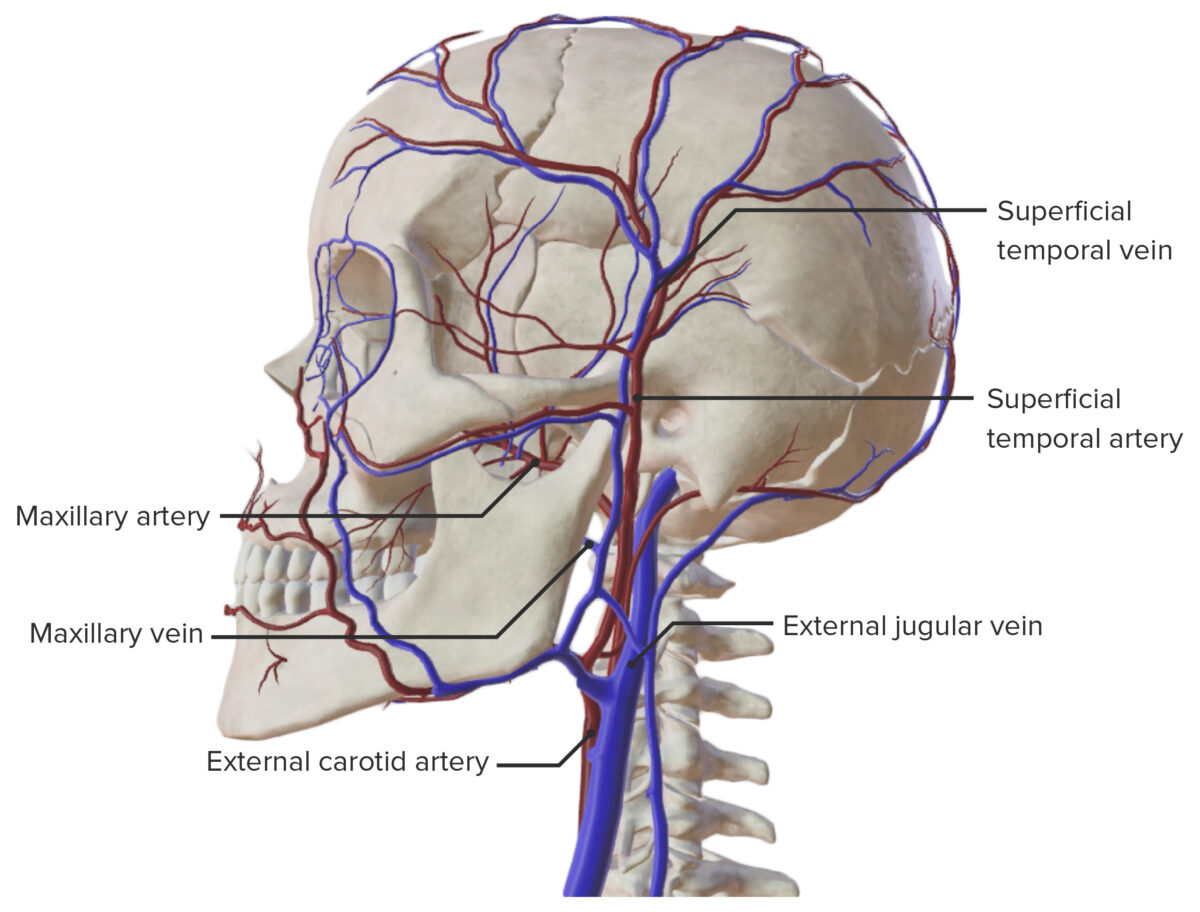
Lateral view of the major arteries and veins of the skull
Image by BioDigital, edited by Lecturio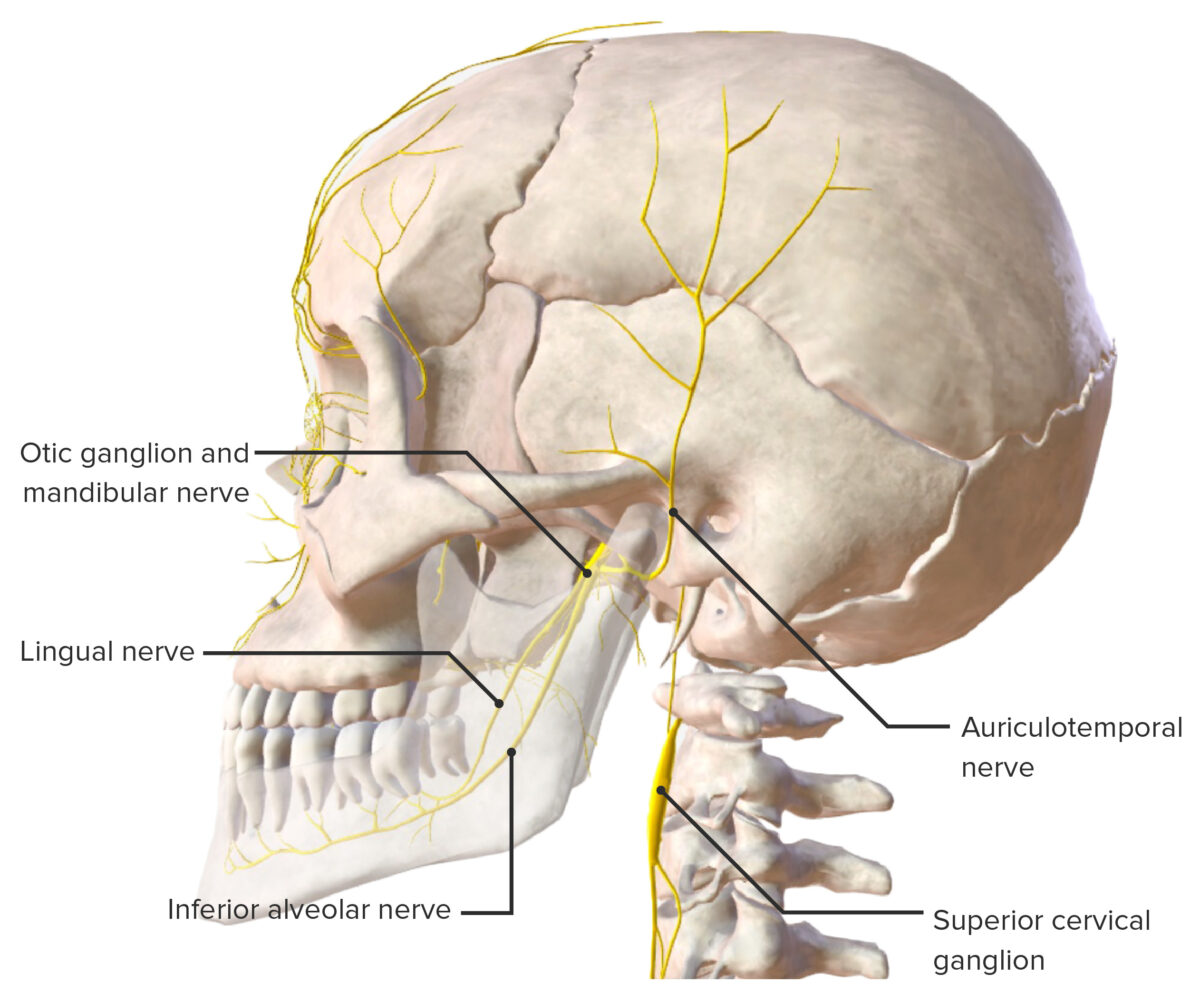
Branches of the trigeminal nerve
Image by BioDigital, edited by LecturioThe following conditions can affect the TMJ: