Giant cell arteritis (GCA), also known as temporal arteritis, is a type of large-vessel vasculitis Vasculitis Inflammation of any one of the blood vessels, including the arteries; veins; and rest of the vasculature system in the body. Systemic Lupus Erythematosus that predominantly affects the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy and its major branches, with a predilection for the branches of the carotid (including the temporal artery). Giant cell arteritis is defined by inflammatory leukocytes Leukocytes White blood cells. These include granular leukocytes (basophils; eosinophils; and neutrophils) as well as non-granular leukocytes (lymphocytes and monocytes). White Myeloid Cells: Histology in the vessel walls leading to reactive damage, ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage, and necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage. Giant cell arteritis causes headaches, scalp tenderness, jaw Jaw The jaw is made up of the mandible, which comprises the lower jaw, and the maxilla, which comprises the upper jaw. The mandible articulates with the temporal bone via the temporomandibular joint (TMJ). The 4 muscles of mastication produce the movements of the TMJ to ensure the efficient chewing of food. Jaw and Temporomandibular Joint: Anatomy pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, vision Vision Ophthalmic Exam problems, and potentially blindness Blindness The inability to see or the loss or absence of perception of visual stimuli. This condition may be the result of eye diseases; optic nerve diseases; optic chiasm diseases; or brain diseases affecting the visual pathways or occipital lobe. Retinopathy of Prematurity. The diagnosis is made with temporal artery biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. Prompt treatment with glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids can relieve symptoms and prevent vision Vision Ophthalmic Exam loss.
Last updated: Apr 15, 2025
Giant cell arteritis (GCA) is caused by a complicated cascade of vascular inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation, damage, and dysfunctional repair:
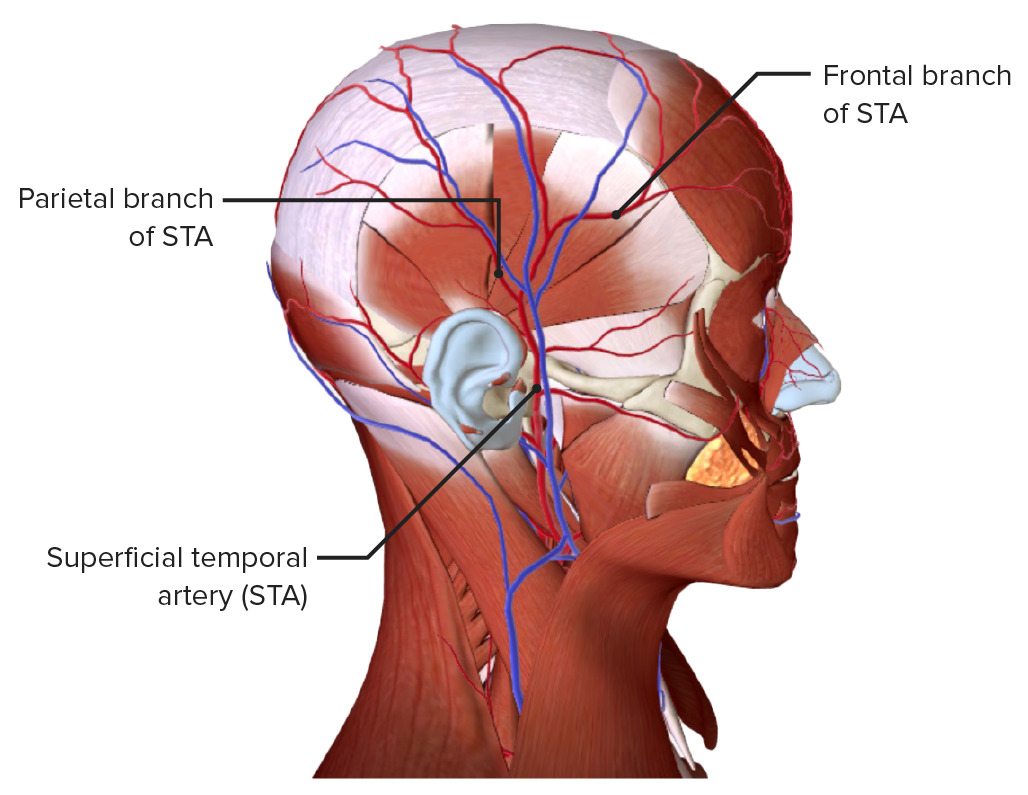
Branches of the STA, which may be involved in GCA
Image by BioDigital, edited by Lecturio.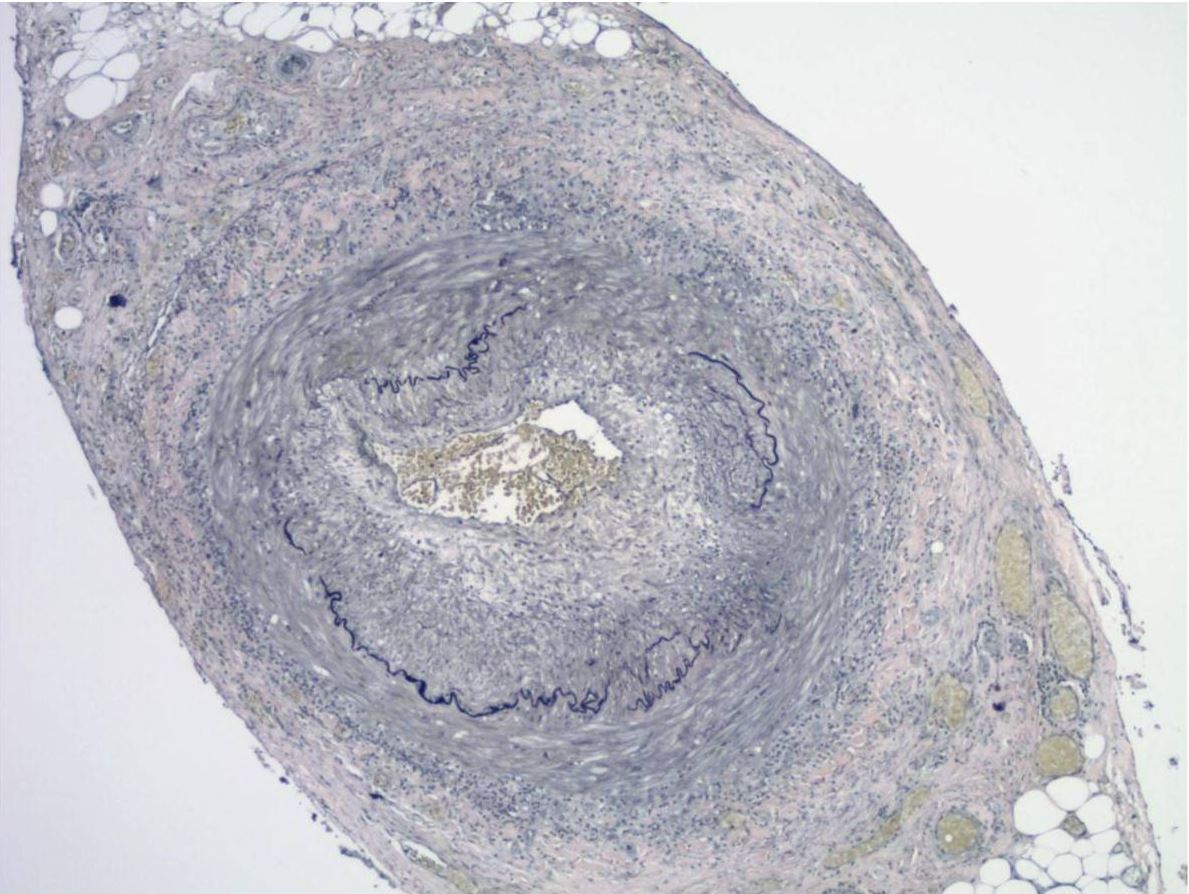
Elastic stains on the same case of a histologically positive temporal artery biopsy showing the fragmentation, distortion, and lack of continuity of the internal elastic lamina, a characteristic feature of temporal arteritis
Image: “Association between human papillomavirus DNA and temporal arteritis” by Mohammadi, A., Pfeifer, J.D., Lewis, J.S. License: CC BY 2.0.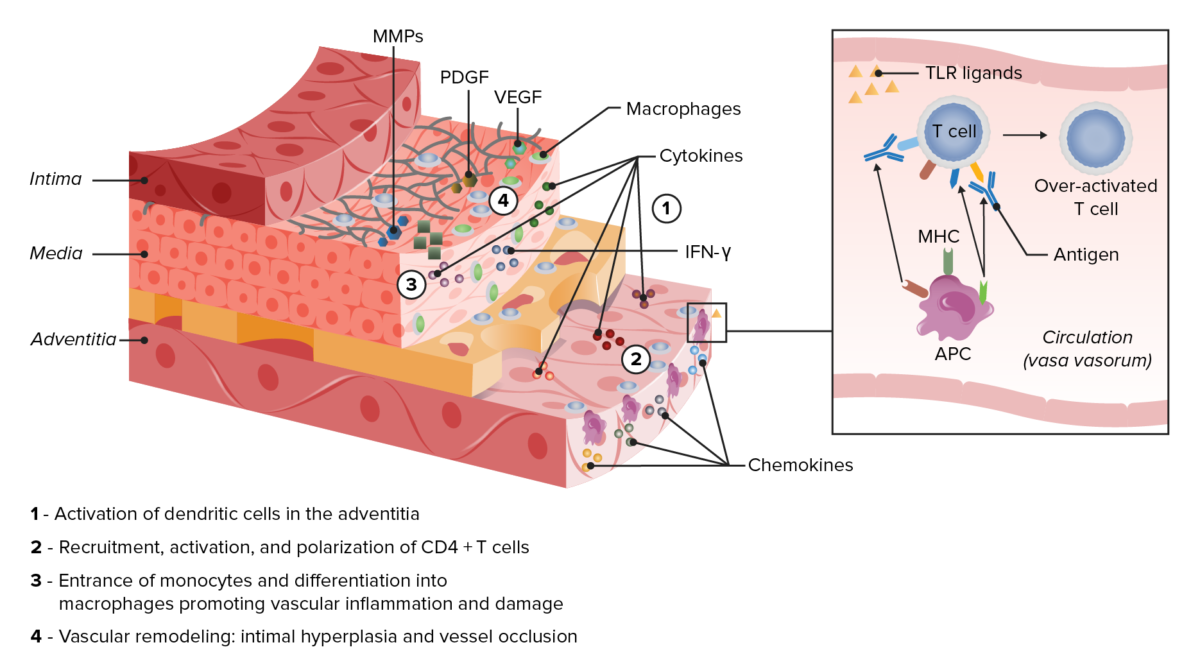
Pathophysiology in giant cell arteritis
Notice the activation of T cells through presentation of an antigen by dendritic cells (APC). These recruit and activate more inflammatory cells, including macrophages, though toll-like receptor ligands (TLR), cytokines, and chemokines. Macrophages will organize into giant cells, and produce matrix metalloproteinases (MMPs) and growth factors (PDGF and VEGF). This causes the destruction and hyperplasia that will eventually cause vessel occlusion.
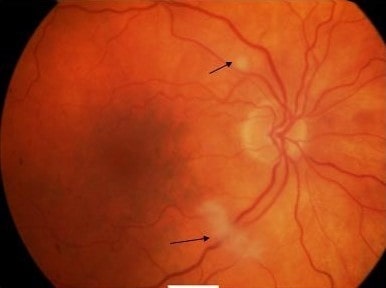
Fundoscopy of the right eye, showing cotton-wool spots along the superotemporal and inferotemporal arterioles (arrows). The cotton-wool spots denote obstruction of the retinal arterioles, leading to retinal ischemia.
Image: “Cotton-wool spots” by James Paget University Hospital NHS Foundation Trust, Lowestoft Road, Gorleston, Great Yarmouth NR31 6LA, Norfolk, UK. License: CC BY 2.0.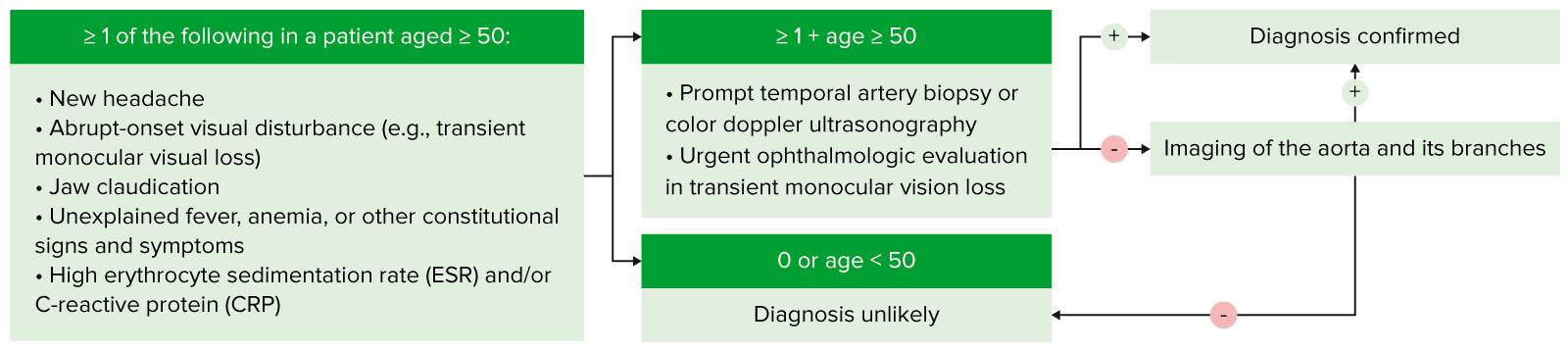
The above is a simple algorithm to help aid in the diagnosis of GCA. This outlines when this disease should be considered, and the basic steps in diagnosis.
Image by Lecturio.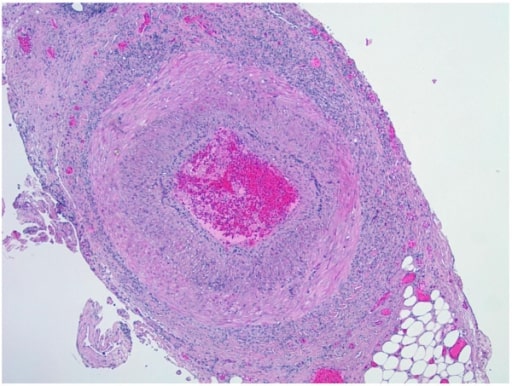
Biopsy of temporal artery showing transmural mixed inflammatory cell infiltrates with intimal thickening, fragmentation, and distortion of the internal elastic lamina
Image: “Biopsy of temporal artery” by the Department of Pathology and Laboratory Medicine, University of Florida, College of Medicine, Jacksonville, FL, USA. License: CC BY 2.0.