Tick-borne encephalitis virus (TBEV) is a positive-sense, single-stranded RNA virus of the genus Flavivirus. Transmission occurs primarily via Ixodes ticks found in Europe, the former Soviet Union, and Asia. The virus causes tick-borne encephalitis. Most patients are asymptomatic; however, symptomatic individuals may experience a biphasic illness. After presenting with nonspecific symptoms such as fever, malaise and arthralgia, individuals can develop a second phase of symptoms characterized by neurologic manifestations, such as meningitis, encephalitis, or meningoencephalitis. Serology or PCR can confirm the diagnosis. There is no effective antiviral therapy for TBEV infections, so management is supportive.
Last updated: Oct 27, 2022
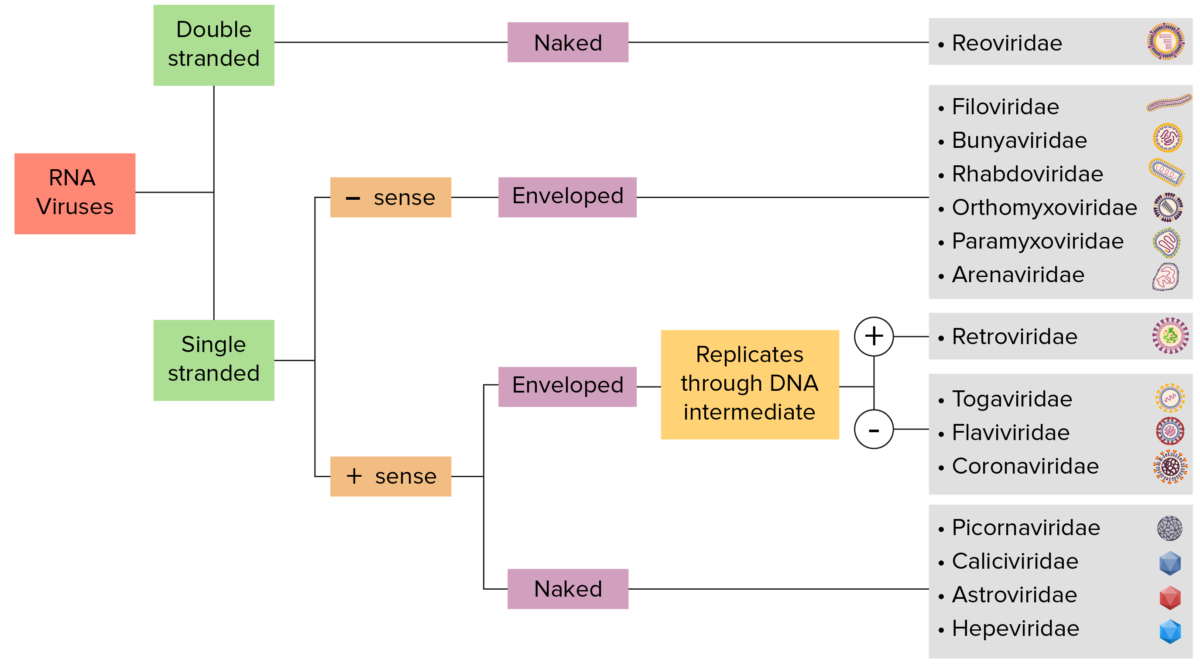
RNA virus identification:
Viruses can be classified in many ways. Most viruses, however, will have a genome formed by either DNA or RNA. RNA genome viruses can be further characterized by either a single- or double-stranded RNA. “Enveloped” viruses are covered by a thin coat of cell membrane (usually taken from the host cell). If the coat is absent, the viruses are called “naked” viruses. Viruses with single-stranded genomes are “positive-sense” viruses if the genome is directly employed as messenger RNA (mRNA), which is translated into proteins. “Negative-sense,” single-stranded viruses employ RNA dependent RNA polymerase, a viral enzyme, to transcribe their genome into messenger RNA.
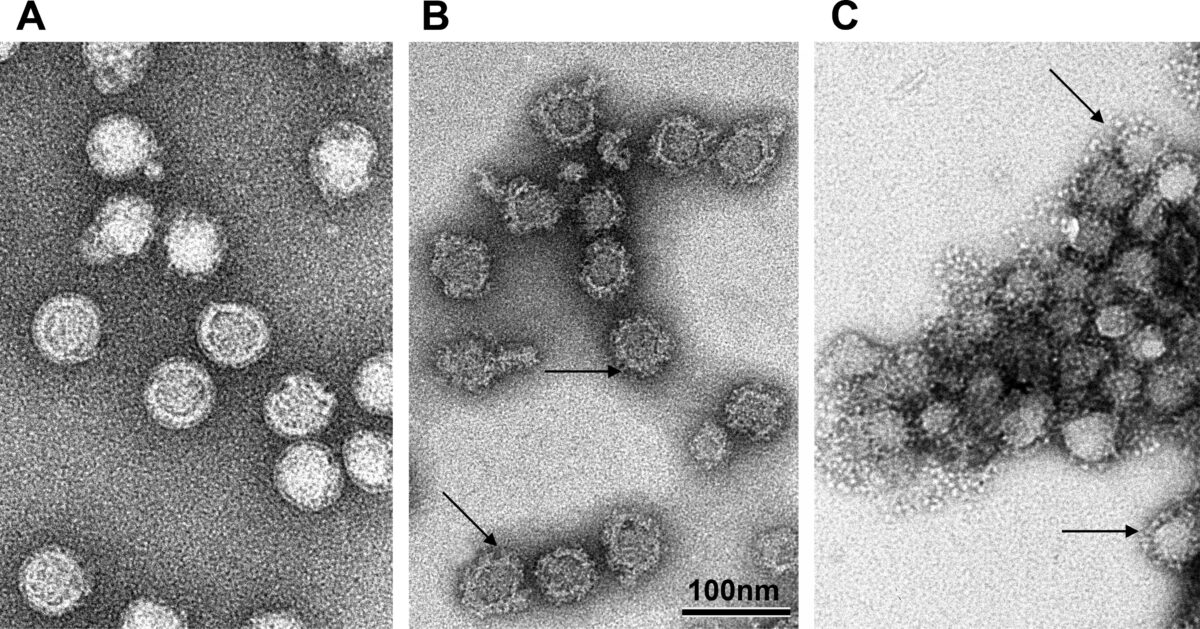
Tick-borne encephalitis virus at different pHs:
A: 8.0
B: 10.0
C: 5.4
Tick-borne encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis (TBE) is caused by 3 subtypes of closely related viruses Viruses Minute infectious agents whose genomes are composed of DNA or RNA, but not both. They are characterized by a lack of independent metabolism and the inability to replicate outside living host cells. Virology:
TBE is the most common tick-borne CNS infection in Europe and Asia ASIA Spinal Cord Injuries.

An adult Ixodes ricinus tick, the vector for the European subtype of tick-borne encephalitis virus
Image: “Soft tick, Ixodes Ricinus, on human skin” by Gabrielsen J. License: CC BY 3.0Outdoor recreational and occupational activities in endemic regions can increase the risk of acquiring TBEV:
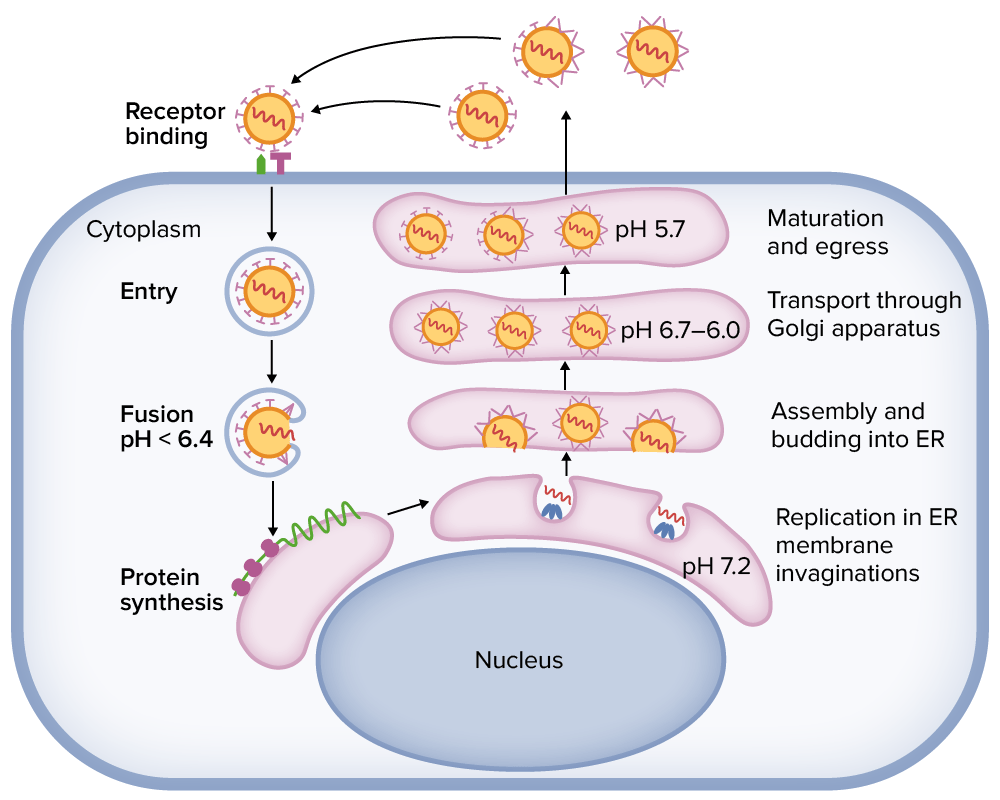
Tick-borne encephalitis virus replication cycle within a cell
ER: endoplasmic reticulum
Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are asymptomatic. Symptomatic individuals may have a biphasic course.
Blood or CSF samples can be used for diagnostic testing:
Supporting evaluation:
There is no specific drug therapy. Management is supportive.
| Organism | Tick-borne encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology | Japanese encephalitis virus Japanese encephalitis virus A species of flavivirus, one of the japanese encephalitis virus group, which is the etiological agent of japanese encephalitis found in Asia, southeast Asia, and the Indian subcontinent. Encephalitis | St. Louis encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology | West Nile virus West Nile Virus West Nile virus is an enveloped, positive-sense, single-stranded RNA virus of the genus Flavivirus. Birds are the primary hosts and the disease is most often transmitted by Culex mosquitoes. Most people infected with West Nile virus are asymptomatic. Some patients develop West Nile fever (a self-limited, febrile illness) and a very small proportion of patients develop West Nile neuroinvasive disease. West Nile Virus |
|---|---|---|---|---|
| Characteristics | The structural features are almost identical. | |||
| Region |
|
|
North America |
|
| Transmission | Tick | Mosquito | Mosquito | Mosquito |
| Clinical |
|
|
|
|
| Diagnosis |
|
Serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus | Serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus |
|
| Management | Supportive | Supportive | Supportive | Supportive |
| Prevention |
|
|
Mosquito avoidance measures | Mosquito avoidance measures |