Q fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever is a bacterial zoonotic infection Zoonotic infection Diseases of non-human animals that may be transmitted to humans or may be transmitted from humans to non-human animals. Brucella/Brucellosis caused by Coxiella burnetii. Transmission occurs primarily through the inhalation of contaminated aerosols and exposure to infected animal products. The clinical presentation can vary and often result in mild disease with flu-like symptoms Flu-Like Symptoms Babesia/Babesiosis. Other manifestations include pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia, hepatitis, endocarditis Endocarditis Endocarditis is an inflammatory disease involving the inner lining (endometrium) of the heart, most commonly affecting the cardiac valves. Both infectious and noninfectious etiologies lead to vegetations on the valve leaflets. Patients may present with nonspecific symptoms such as fever and fatigue. Endocarditis, and aseptic meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis. In a small percentage of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, the disease can become chronic. A high degree of suspicion is required to make the diagnosis, which is aided using serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus and PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR). Antibiotics are the mainstay of management.
Last updated: Sep 11, 2023
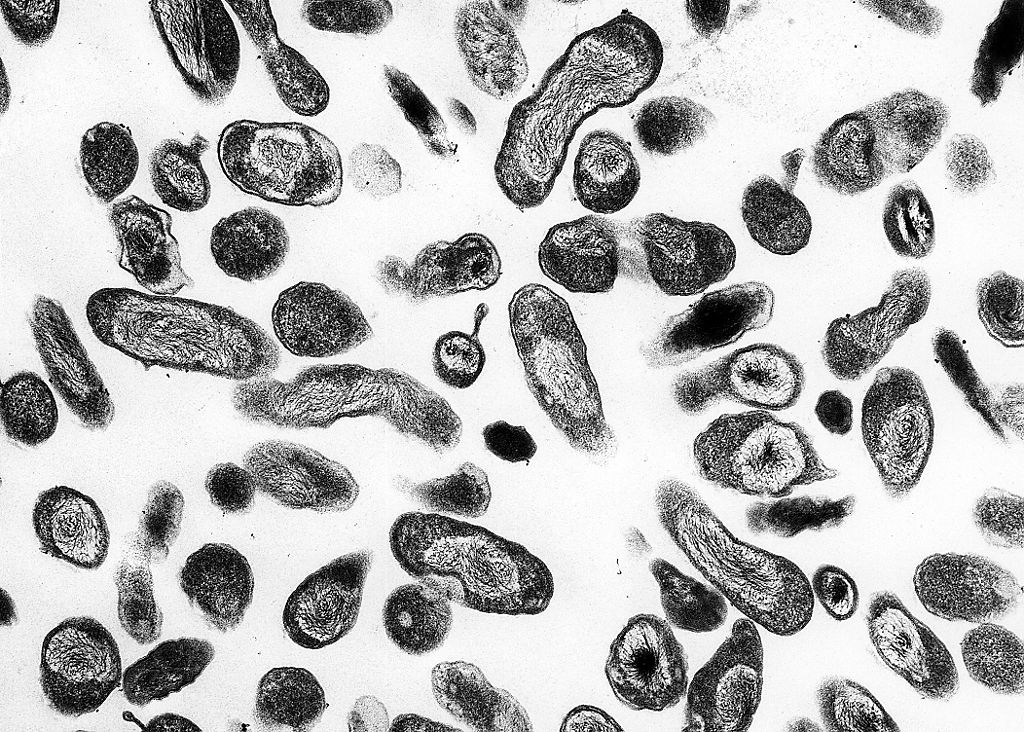
Coxiella under light microscope
Image: “Coxiella burnetii” by NIAID. License: Public Domain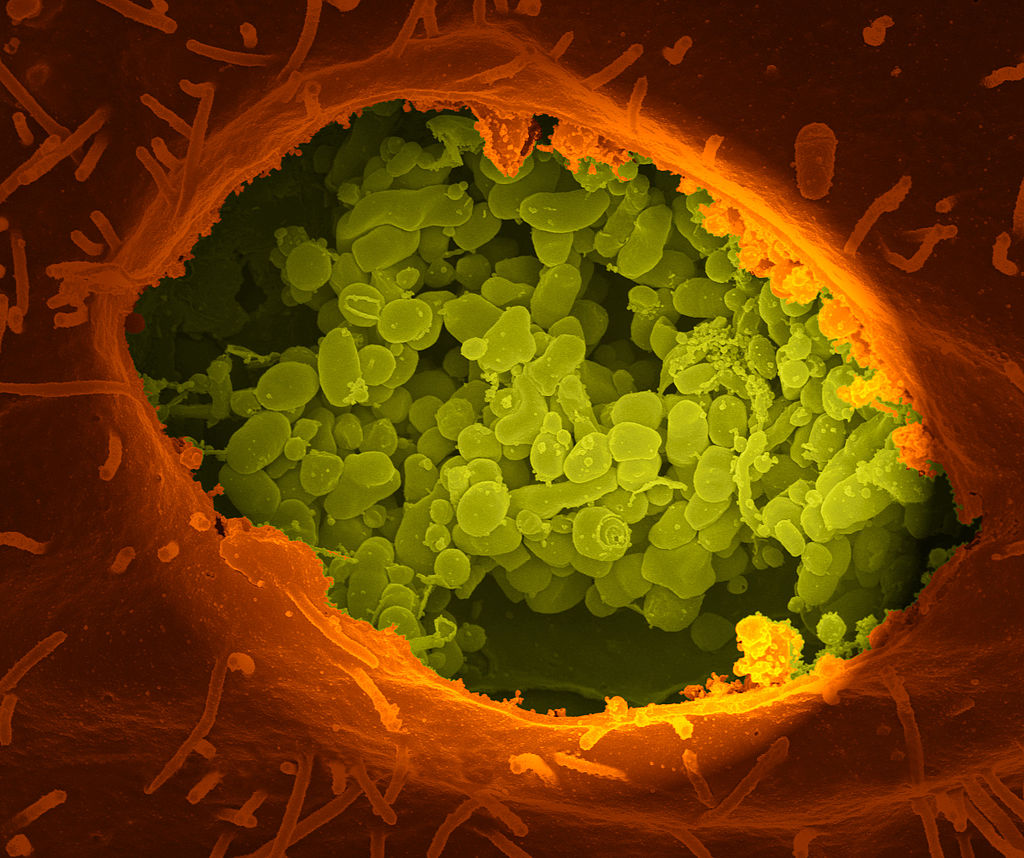
A dry fracture of a cell exposing the contents of a vacuole where Coxiella burnetii (green color) are growing
Image: “A dry fracture of a Vero cell” by National Institutes of Health (NIH). License: Public DomainCoxiella burnetii causes Q fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever.
Antigenic phase variation Phase variation The outer surface proteins are modified to adapt to changes in the host environment. Haemophilus:
Morphological variants:
Escape from intracellular killing:
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may present with a wide range of symptoms, and vary in severity from asymptomatic to severe disease.
The incubation Incubation The amount time between exposure to an infectious agent and becoming symptomatic. Rabies Virus period for acute infection is approximately 20 days. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may present with any of the following conditions:
Chronic infection may manifest months or years after an acute infection.
Q fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever in pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care is associated with:
Q fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever lacks a distinct clinical presentation; therefore, the diagnosis relies on a high index of suspicion based on the patient’s risk factors.
Diagnostic testing:
Supporting evaluation:
Antibiotic therapy includes:
| Organism | Coxiella burnetii | Legionella pneumophila Legionella pneumophila A species of gram-negative, aerobic bacteria that is the causative agent of legionnaires’ disease. It has been isolated from numerous environmental sites as well as from human lung tissue, respiratory secretions, and blood. Legionella/Legionellosis | Francisella tularensis Francisella Tularensis Aminoglycosides |
|---|---|---|---|
| Characteristics |
|
|
|
| Reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli |
|
Aquatic |
|
| Transmission |
|
|
|
| Clinical presentation | Q fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever |
|
Tularemia |
| Diagnosis |
|
|
|
| Management | Doxycycline |
|
Streptomycin |
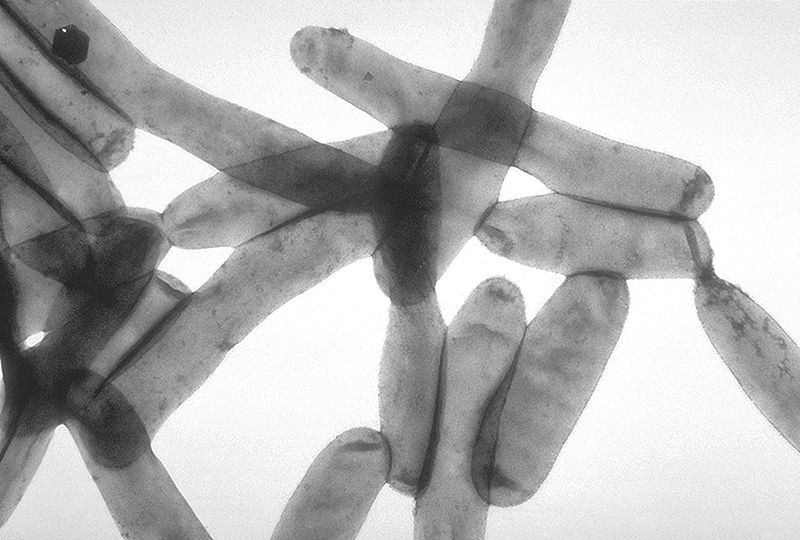
Microscopic view of Legionella pneumophila
Image: “Legionella pneumophila” by CDC. License: Public Domain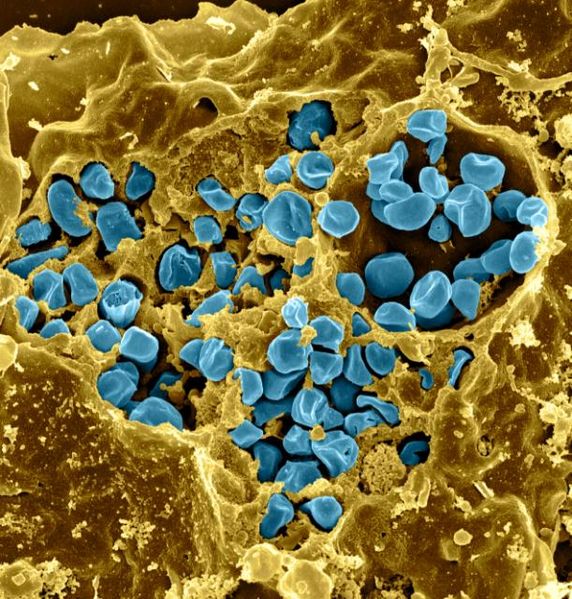
Dry fracture of a macrophage infected with Francisella tularensis (blue color)
Image: “Macrophage Infected with Francisella tularensis Bacteria” by NIAID. License: CC BY 2.0