Meningitis is inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy, the protective membranes of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification, and spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, altered mental status Altered Mental Status Sepsis in Children, and nuchal rigidity Rigidity Continuous involuntary sustained muscle contraction which is often a manifestation of basal ganglia diseases. When an affected muscle is passively stretched, the degree of resistance remains constant regardless of the rate at which the muscle is stretched. This feature helps to distinguish rigidity from muscle spasticity. Megacolon. Diagnosis of meningitis is made on clinical grounds with a thorough neurologic examination. CSF analysis is an important diagnostic tool, as it is difficult to identify the exact cause clinically. Management of meningitis includes immediate broad-spectrum Broad-Spectrum Fluoroquinolones antibiotics and supportive therapy to prevent complications. Specific treatment depends on the etiology of meningitis. Delay in treatment can lead to permanent neurologic defects and death.
Last updated: May 16, 2024
Meningitis is inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the protective membranes of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy, collectively called the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy, that is commonly caused by an acute infection.
Meningitis can be of infectious (most common) or noninfectious origin. Infectious meningitis can be community- or hospital-acquired.
Bacterial meningitis:
Viral meningitis:
Fungal meningitis:
Parasitic meningitis:

3-dimensional (3D) image of a group of diplococcal gram-negative Neisseria meningitidis
Direct inoculation of the infectious agent into the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy is rare in meningitis. Usually, infection at an adjacent or remote site spreads to the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification.
Acute meningitis:
Chronic meningitis:
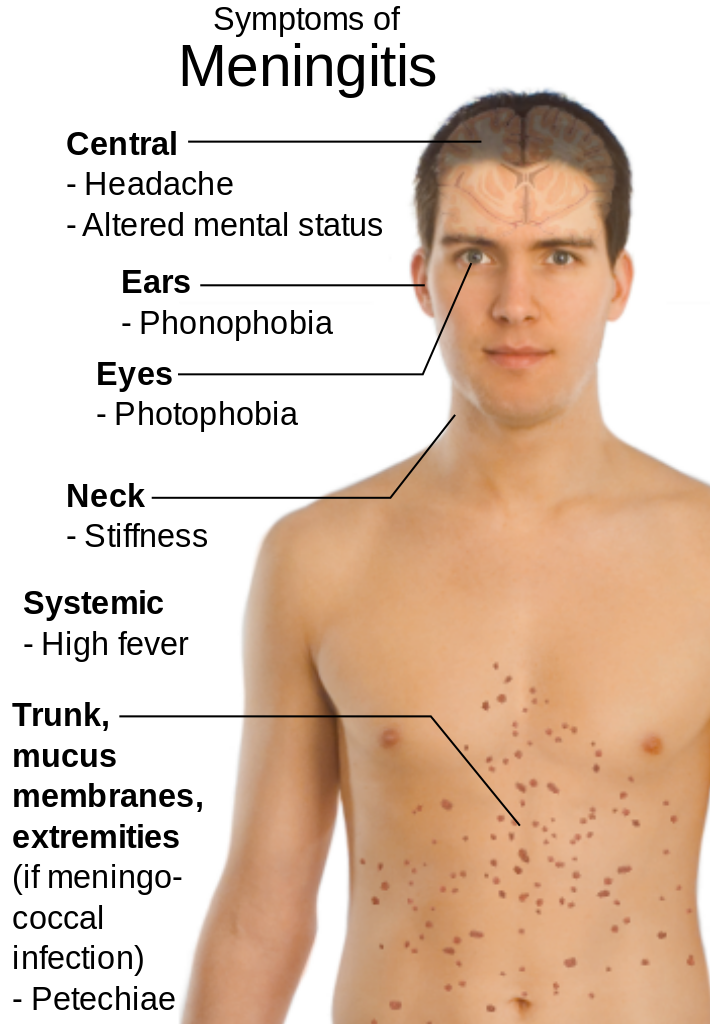
Clinical presentation of meningitis
Image: “Main symptoms of Meningitis” by Mikael Häggström. License: Public Domain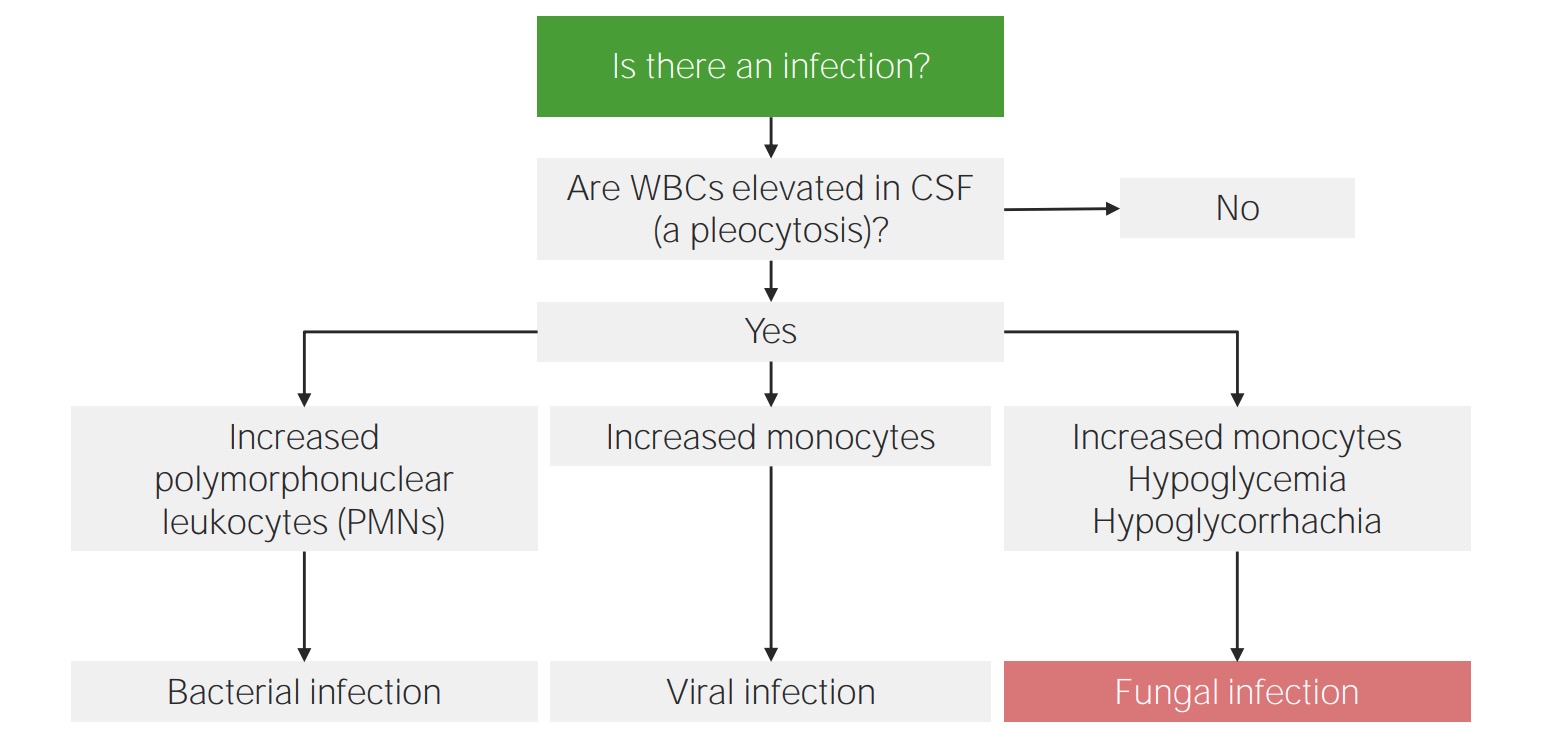
Approach to CSF analysis in meningitis:
Differential count is the key to identifying the etiology of meningitis.
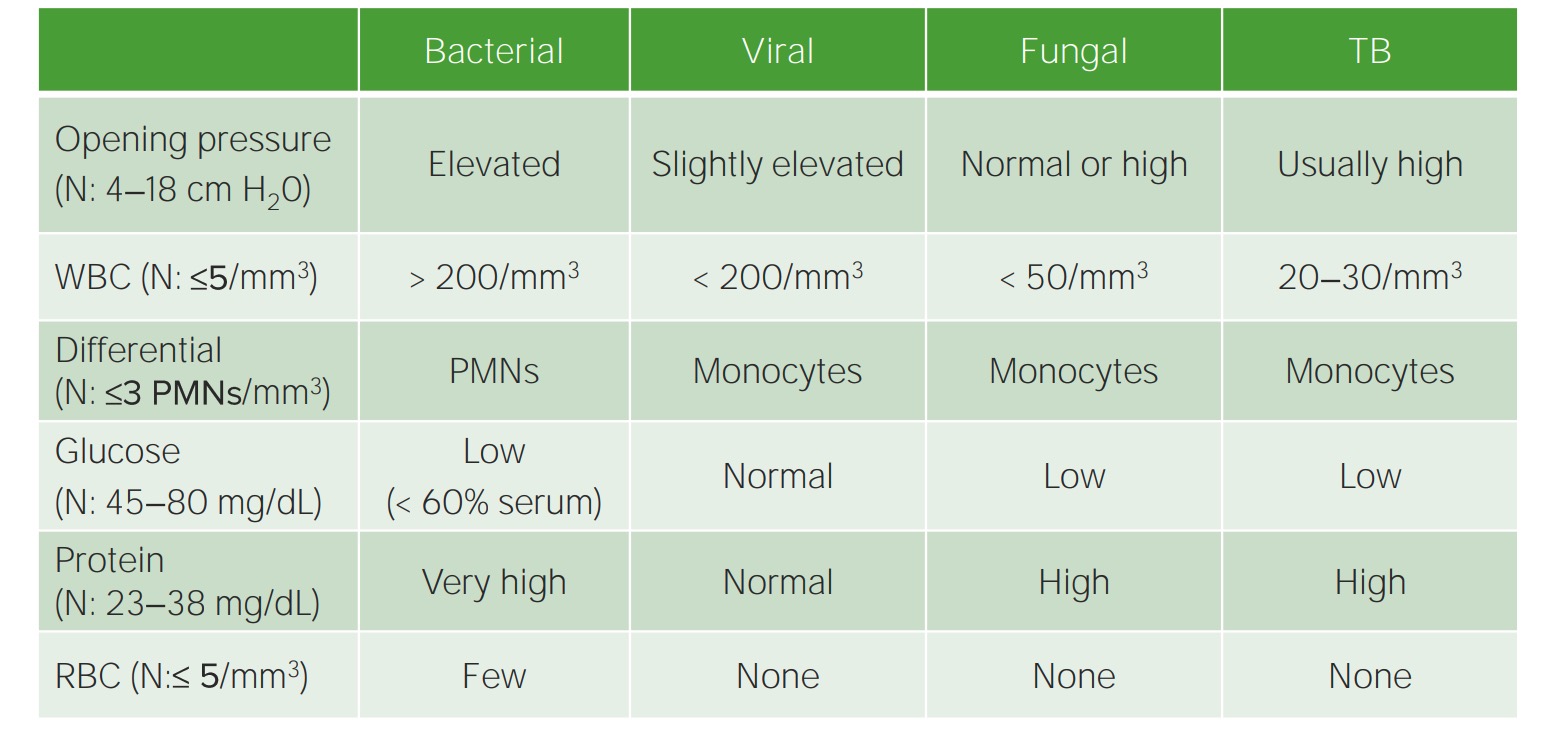
Parameters of CSF analysis in meningitis
N: NormalImaging is not required for diagnosis but is usually indicated before performing a lumbar puncture Lumbar Puncture Febrile Infant if there is a concern about high intracranial pressure Intracranial Pressure Idiopathic Intracranial Hypertension and to detect complications.
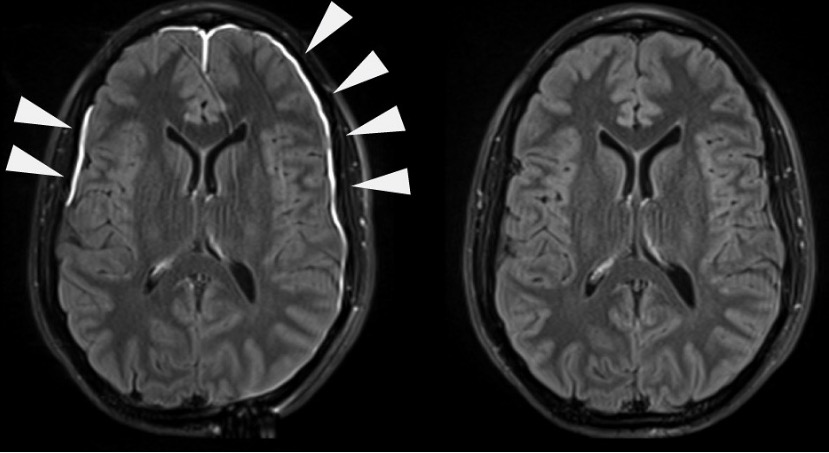
Meningeal irritation evident on contrast-enhanced MRI
Treatment is based on the type of meningitis. Supportive care is common for most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Broad-spectrum Broad-Spectrum Fluoroquinolones antibiotics are usually administered as an immediate measure while the cause is being determined.
Bacterial meningitis:
Viral meningitis:
Viral meningitis is usually self-limiting Self-Limiting Meningitis in Children and requires only supportive management. Antiviral Antiviral Antivirals for Hepatitis B therapy is indicated only in selected and/or severe cases.
Fungal meningitis:
Other types of meningitis:
Vaccinations can protect against certain types of meningitis: