An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage; this condition may be due to cerebral blood vessel occlusion by thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus or embolism, or rarely due to systemic hypoperfusion. The clinical presentation includes neurologic symptoms with varying degrees of motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology and sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology loss corresponding to the area of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification that is affected and the extent of tissue damage. Diagnosis is made by physical examination and imaging. Management is ideally with thrombolytic therapy to restore blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure, depending on the time frame and clinical situation. Long-term rehabilitation with physical, occupational, and speech therapies is important after the acute event.
Last updated: Jul 10, 2023
An ischemic stroke is an acute neurologic injury that occurs as a result of brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage; this condition may be due to cerebral blood vessel occlusion by thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus or embolism or, rarely, due to systemic hypoperfusion.
Thrombotic stroke:
Embolic stroke:
Systemic hypoperfusion:
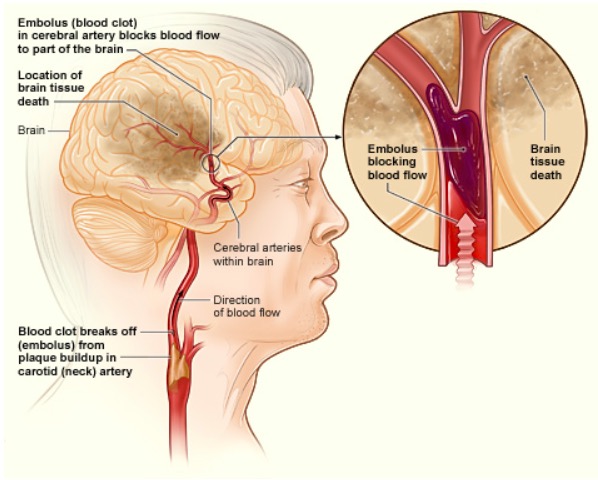
How an ischemic stroke can occur in the brain:
If a blood clot breaks away from plaque buildup in the carotid (neck) artery, it can travel to and lodge in an artery in the brain. The clot can block blood flow to a part of the brain, causing brain tissue death.
A complete reduction in cerebral blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure results in the death of brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification tissue within 4–10 minutes:
Diagnosis is made with a suggestive history and clinical examination findings and confirmed by neuroimaging Neuroimaging Non-invasive methods of visualizing the central nervous system, especially the brain, by various imaging modalities. Febrile Infant.
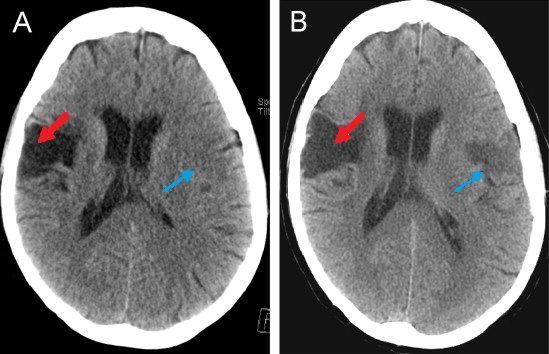
Computed tomogram of an individual with middle cerebral artery stroke illustrating hypodense areas within the temporal and frontal lobes
Image: “CT scan of a patient with middle cerebral artery stroke” by 0475ramosk. License: CC BY-SA 4.0The goal of stroke management is to ensure prompt intervention and optimal outcomes. If possible, restoration of adequate blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure to the injured regions and saving the ischemic penumbra from permanent injury should be attempted.
Complications:
Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas depends on these predictors of outcomes: