Head trauma occurs when external forces are directed to the skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy and brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification structures, resulting in damage to the skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy, brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification injury), and range from mild to severe and life-threatening. The majority of cases are mild, but presentation can vary from a mild concussion to a comatose state Comatose State Coma depending on the severity of the insult. Management ranges from observation to intensive care monitoring and neurosurgical interventions. Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is good for mild injuries, but severe trauma can result in death or permanent damage.
Last updated: Mar 21, 2023
Head trauma is an injury to the skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy, brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification, and/or intracranial structures.
| Feature | Response | Score |
|---|---|---|
| Eye opening | Open spontaneously | 4 |
| Open to verbal command | 3 | |
| Open to pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 2 | |
| No eye opening | 1 | |
| Verbal response | Oriented and appropriate | 5 |
| Disoriented but conversant | 4 | |
| Nonsensical words | 3 | |
| Moaning | 2 | |
| Silent | 1 | |
| Motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology response | Follows commands | 6 |
| Localizes pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 5 | |
| Withdraws from pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 4 | |
| Flexor posturing | 3 | |
| Extensor posturing Extensor posturing A condition characterized by abnormal posturing of the limbs that is associated with injury to the brainstem. This may occur as a clinical manifestation or induced experimentally in animals. The extensor reflexes are exaggerated leading to rigid extension of the limbs accompanied by hyperreflexia and opisthotonus. This condition is usually caused by lesions which occur in the region of the brainstem that lies between the red nuclei and the vestibular nuclei. In contrast, decorticate rigidity is characterized by flexion of the elbows and wrists with extension of the legs and feet. The causative lesion for this condition is located above the red nuclei and usually consists of diffuse cerebral damage. Increased Intracranial Pressure (ICP) | 2 | |
| Flaccid | 1 |
| Criteria | Mild | Moderate | Severe |
|---|---|---|---|
| Structural imaging | Normal | Normal or abnormal | Normal or abnormal |
| LOC | 0–30 minutes | > 30 minutes and < 24 hours | > 24 hours |
| AOC | For a moment, up to 24 hours | > 24 hours severity based on other criteria | |
| PTA PTA A peritonsillar abscess (PTA), also called quinsy, is a collection of pus between the capsule of the palatine tonsil and the pharyngeal muscles. A pta is usually a complication of acute tonsillitis, an infection caused by group a streptococci. Patients often present with a sore throat, trismus, and a muffled voice. Peritonsillar Abscess | 0–1 day | > 1 and < 7 days | > 7 days |
| GCS GCS A scale that assesses the response to stimuli in patients with craniocerebral injuries. The parameters are eye opening, motor response, and verbal response. Coma | 13–15 | 9–12 | < 9 |
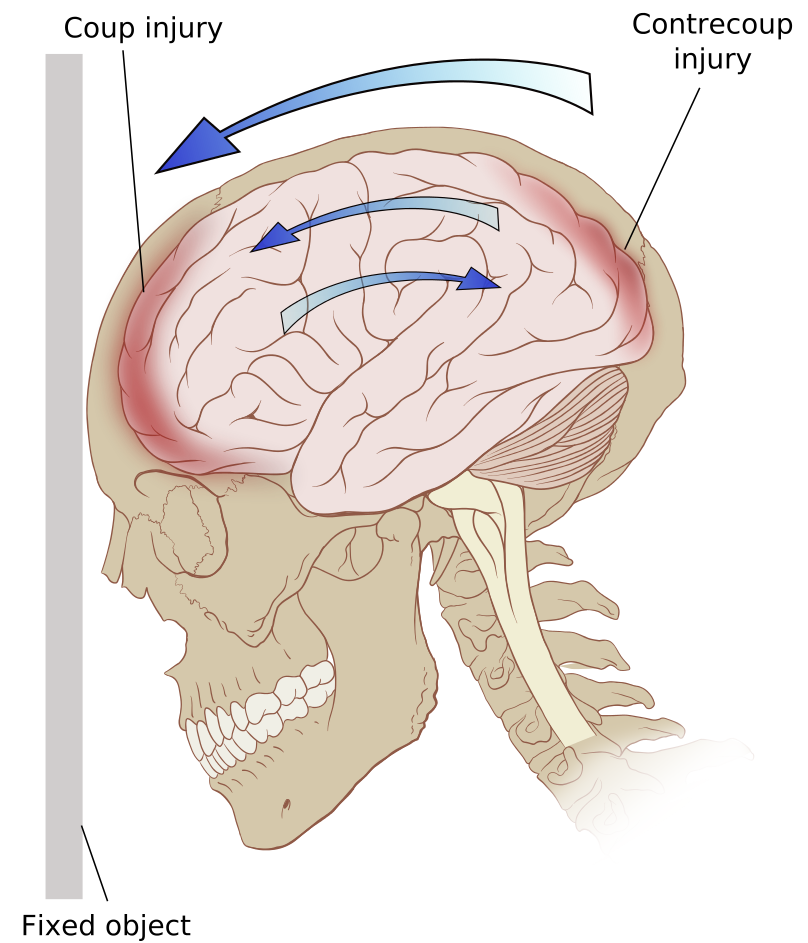
Coup and contrecoup head injury
Image: “Contrecoup” by Patrick J. Lynch. License: CC BY 2.5Linear fractures:
Comminuted fractures:
Depressed fractures:
Elevated fractures:
Basilar skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy fractures:
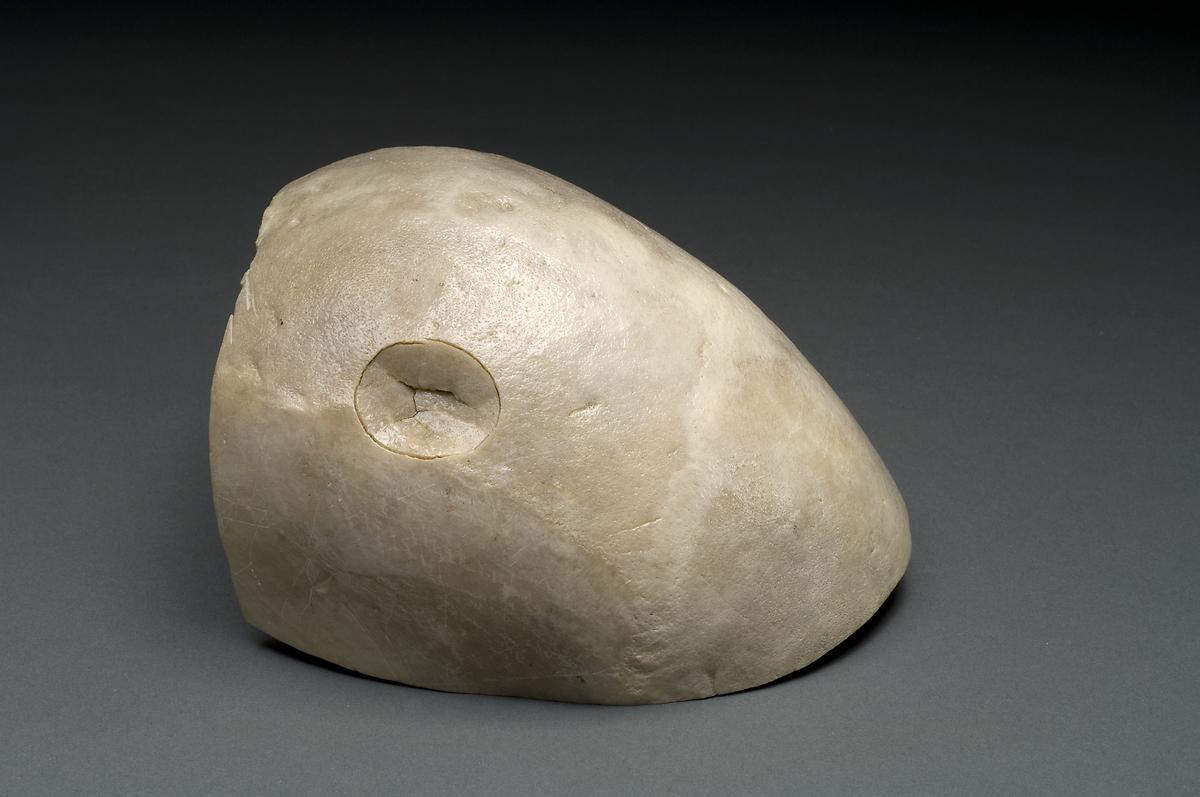
Depressed skull fracture: skull showing ball-peen hammer trauma
Image: “Depressed skull fracture” by National Institutes of Health, Health & Human Services. License: Public Domain
Bilateral periorbital ecchymosis: manifestation of basilar skull fracture
Image: “Bilateral periorbital ecchymosis (raccoon eyes)” by Marion County Sheriff’s Office. License: Public DomainFocal cerebral contusions:
Extra-axial hemorrhage:
The CCHR is used to determine the need for CT in adult emergency department patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with minor head injuries. Its sensitivity is close to 100% for identifying clinically significant brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification trauma (i.e., trauma that requires neurosurgical intervention).
Requirements:
Inclusion criteria:
Exclusion criteria:
High-risk factors:
Medium risk factors:
Interpretation:
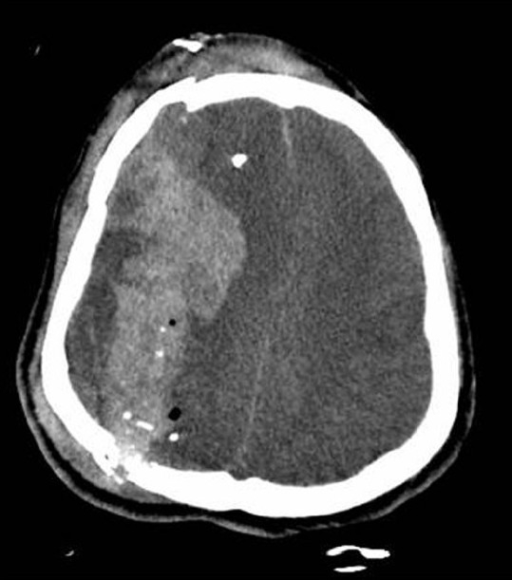
Computed tomography image of a patient’s skull fractures and fragmentation with acute intracerebral hemorrhage and midline shift
Image: “Traumatic brain injury complicated by environmental hyperthermia” by Hermstad E, Adams B. License: CC BY 2.0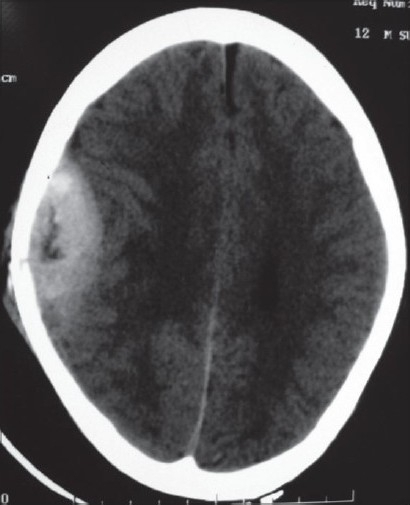
Computed tomography scan of right parietal epidural hematoma
Image: “Pathological intracranial extradural hematoma in a 10-year-old child” by Bhat AR, Jain AK, Kirmani AR, Nizami F. License: CC BY 2.0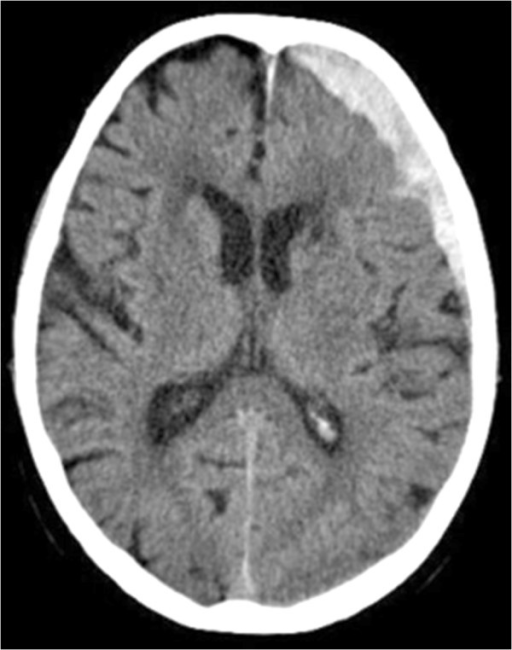
Computed tomography scan demonstrating the fronto-temporal subdural hematoma over the left hemisphere
Image: “Lactococcus garvieae endocarditis presenting with subdural haematoma” by Rasmussen M, Björk Werner J, Dolk M, Christensson B. License: CC BY 2.0Intensive care management (typically required):
Control of ICP ICP Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP):
Surgery: