Intussusception occurs when a part of the intestine (intussusceptum) telescopes into another part (intussuscipiens) of the intestine. The condition can cause obstruction and, if untreated, progress to bowel ischemia Bowel ischemia Mesenteric ischemia is a rare, life-threatening condition caused by inadequate blood flow through the mesenteric vessels, which results in ischemia and necrosis of the intestinal wall. Mesenteric ischemia can be either acute or chronic. Mesenteric Ischemia. Intussusception is most common in the pediatric population, but is occasionally encountered in adults. The pediatric patient typically presents with acute cyclical abdominal pain Abdominal Pain Acute Abdomen and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, while adults present with symptoms of bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis. The diagnosis in children is frequently clinical but may be supported by an abdominal ultrasound showing a classic target sign Target sign Pseudomembranous Colitis. Management options in children include contrast or pneumatic enema, with surgical options reserved for failure of the non-operative measures, complications such as gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction or perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis, and treatment of underlying pathology. In adult patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, surgery is usually required.
Last updated: Jan 18, 2024
Intussusception is telescoping of the proximal part (intussusceptum) into a distal part (intussuscipiens) of the intestine.
Toddlers/infants:
Adults/older children:
History:
Physical exam:
Imaging:

Ileocolic intussusception:
Ultrasonography of the right upper abdominal quadrant shows target sign.
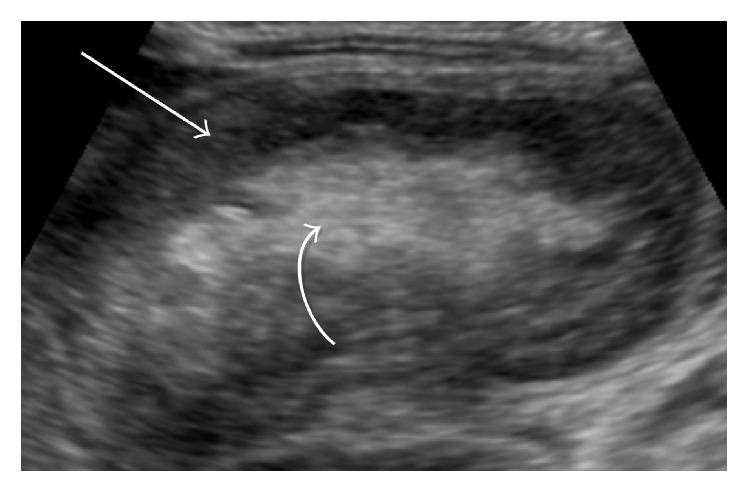
Abdominal ultrasound in the midline demonstrates an ovoid mass (curved arrow) showing the characteristic pseudokidney feature of intussusception.
Image: “Rectal Bleeding and Abdominal Pain Following Vaccination in a 4-Month-Old Infant” by Case Reports in Pediatrics. License: CC BY 4.0History:
Physical exam:
Imaging:
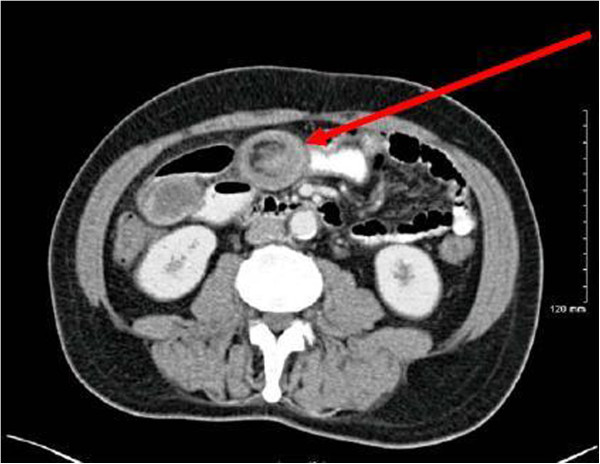
Jejuno-jejunal intussusception secondary to inflammatory fibroid polyp
Image: “Recurrent adult jejuno-jejunal intussusception due to inflammatory fibroid polyp – Vanek’s tumour: a case report” by Joyce KM, Waters PS, Waldron RM, Khan I, Orosz ZS, Németh T, Barry K. License: CC BY 4.0Initial management:
Nonsurgical reduction:
Surgical management:
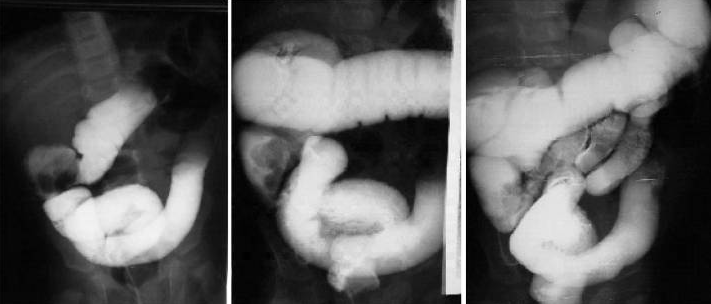
Reduction of ileocolic intussusception with barium enema in a 2-year-old child. The last image shows filling of the cecum and distal small bowel, indicating complete reduction.
Image: “Comparison of different modalities for reducing childhood intussusception” by Alehossein M, Babaheidarian P, Salamati P. License: CC BY 2.5General considerations:
Initial/supportive management:
Surgery:
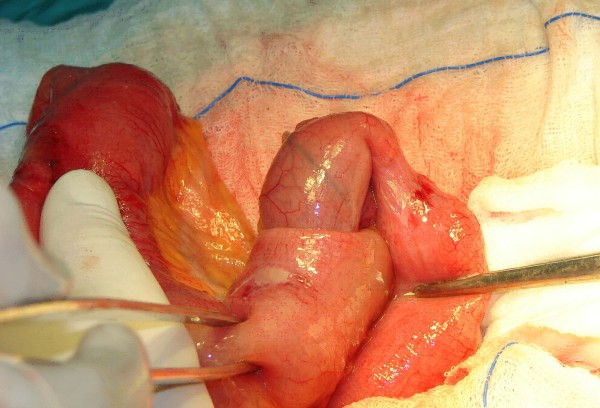
Intraoperative image of an ileoileal intussusception
Image: “Ileoileal intussusception induced by a gastrointestinal stromal tumor” by Vasiliadis K, Kogopoulos E, Katsamakas M, Karamitsos E, Tsalikidis C, Pringos B, Tsalikidis A. License: CC BY 2.0