Esophagitis is the inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation or irritation of the esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy. The major types of esophagitis are medication-induced, infectious, eosinophilic, corrosive, and acid reflux. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with odynophagia Odynophagia Epiglottitis, dysphagia Dysphagia Dysphagia is the subjective sensation of difficulty swallowing. Symptoms can range from a complete inability to swallow, to the sensation of solids or liquids becoming "stuck." Dysphagia is classified as either oropharyngeal or esophageal, with esophageal dysphagia having 2 sub-types: functional and mechanical. Dysphagia, and retrosternal chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. Diagnosis is by endoscopy Endoscopy Procedures of applying endoscopes for disease diagnosis and treatment. Endoscopy involves passing an optical instrument through a small incision in the skin i.e., percutaneous; or through a natural orifice and along natural body pathways such as the digestive tract; and/or through an incision in the wall of a tubular structure or organ, i.e. Transluminal, to examine or perform surgery on the interior parts of the body. Gastroesophageal Reflux Disease (GERD) and biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. Laboratory tests and imaging are obtained, depending on the degree of damage and involvement of other organ systems. Treatment for esophagitis depends on the underlying etiology and includes dietary changes, avoidance of offending agents, antibiotic therapy, or proton pump Pump ACES and RUSH: Resuscitation Ultrasound Protocols inhibitor use. In severe cases such as in corrosive injury, surgery may need to be performed. If left untreated, esophagitis can lead to complications such as strictures, metaplasia Metaplasia A condition in which there is a change of one adult cell type to another similar adult cell type. Cellular Adaptation of the esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy, and development of malignancy Malignancy Hemothorax.
Last updated: May 17, 2024
To remember the common causes of esophagitis: “PIECE”
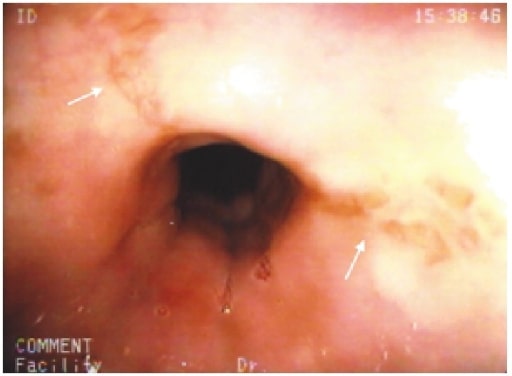
Stellate erosions in the midesophagus (white arrows) in a patient with cloxacillin-induced esophagitis
Image: “Cloxacillin: A New Cause of Pill-Induced Esophagitis” by Zezos P, Harel Z, Saibil F. License: CC BY 4.0Diagnosis is done by upper endoscopy Endoscopy Procedures of applying endoscopes for disease diagnosis and treatment. Endoscopy involves passing an optical instrument through a small incision in the skin i.e., percutaneous; or through a natural orifice and along natural body pathways such as the digestive tract; and/or through an incision in the wall of a tubular structure or organ, i.e. Transluminal, to examine or perform surgery on the interior parts of the body. Gastroesophageal Reflux Disease (GERD).
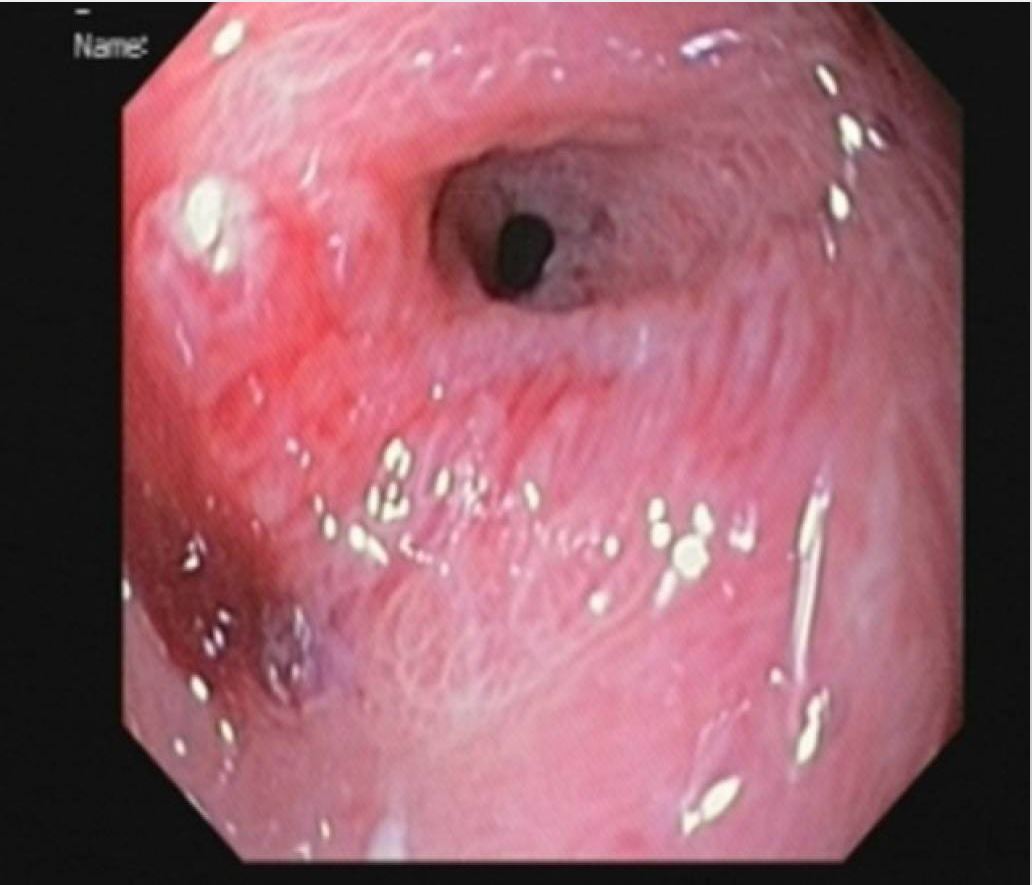
Upper gastrointestinal endoscopic findings in a patient with cytomegalovirus esophagitis. An ulcer with a white base is seen in the esophagus.
Image: “Cytomegalovirus esophagitis developing during chemoradiotherapy for esophageal cancer” by Journal of Medical Case Reports. License: CC BY 4.0Diagnosis is done by upper endoscopy Endoscopy Procedures of applying endoscopes for disease diagnosis and treatment. Endoscopy involves passing an optical instrument through a small incision in the skin i.e., percutaneous; or through a natural orifice and along natural body pathways such as the digestive tract; and/or through an incision in the wall of a tubular structure or organ, i.e. Transluminal, to examine or perform surgery on the interior parts of the body. Gastroesophageal Reflux Disease (GERD).
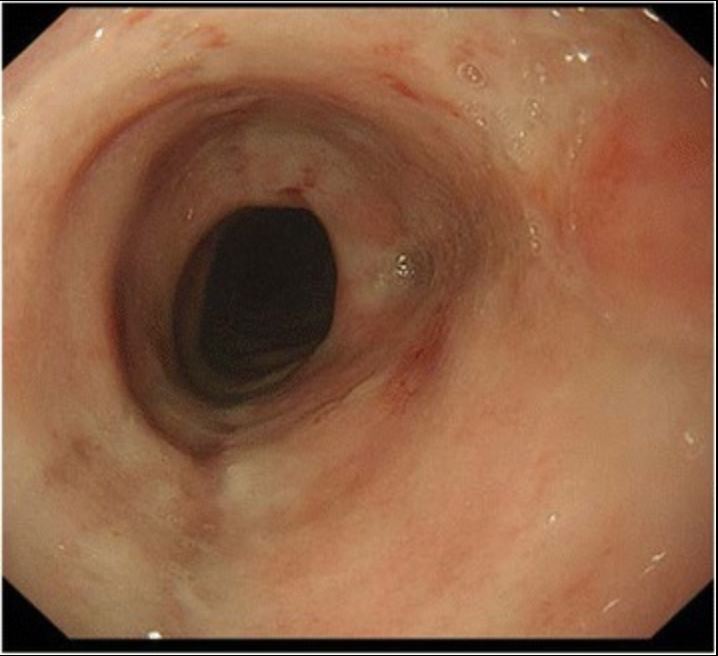
Upper digestive endoscopy of a patient showing numerous injuries on the esophageal surface that are yellow-whitish in color, pleomorphic, and isolated small circular plaques with central erosions.
Image: “Herpetic esophagitis in immunocompetent medical student” by Marinho AV, Bonfim VM, de Alencar LR, Pinto SA, de Araújo Filho JA. License: CC BY 3.0Diagnosis is done by upper endoscopy Endoscopy Procedures of applying endoscopes for disease diagnosis and treatment. Endoscopy involves passing an optical instrument through a small incision in the skin i.e., percutaneous; or through a natural orifice and along natural body pathways such as the digestive tract; and/or through an incision in the wall of a tubular structure or organ, i.e. Transluminal, to examine or perform surgery on the interior parts of the body. Gastroesophageal Reflux Disease (GERD).

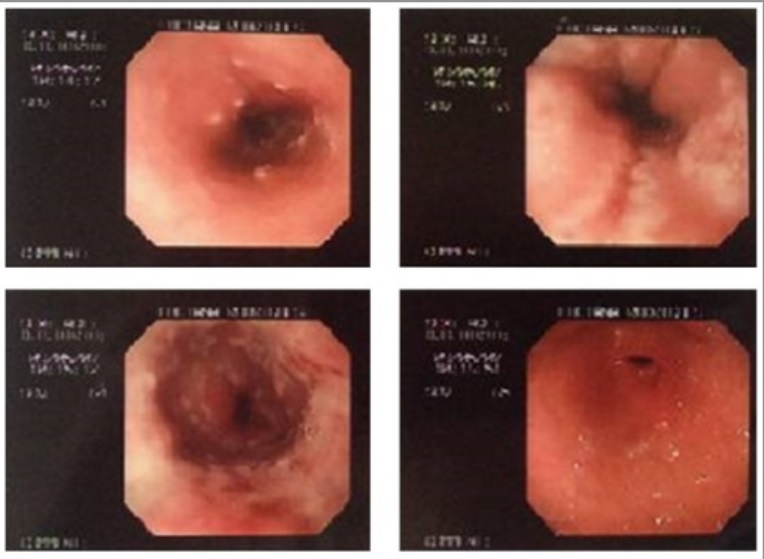
Esophagogastroduodenoscopy illustrates diffuse white lesions in the esophagus characteristic of Candida esophagitis.
Image: “Epigastric Distress Caused by Esophageal Candidiasis” by Chen KH, Weng MT, Chou YH, Lu YF, Hsieh CH. License: CC BY 4.0Diagnosis is done by upper endoscopy Endoscopy Procedures of applying endoscopes for disease diagnosis and treatment. Endoscopy involves passing an optical instrument through a small incision in the skin i.e., percutaneous; or through a natural orifice and along natural body pathways such as the digestive tract; and/or through an incision in the wall of a tubular structure or organ, i.e. Transluminal, to examine or perform surgery on the interior parts of the body. Gastroesophageal Reflux Disease (GERD).
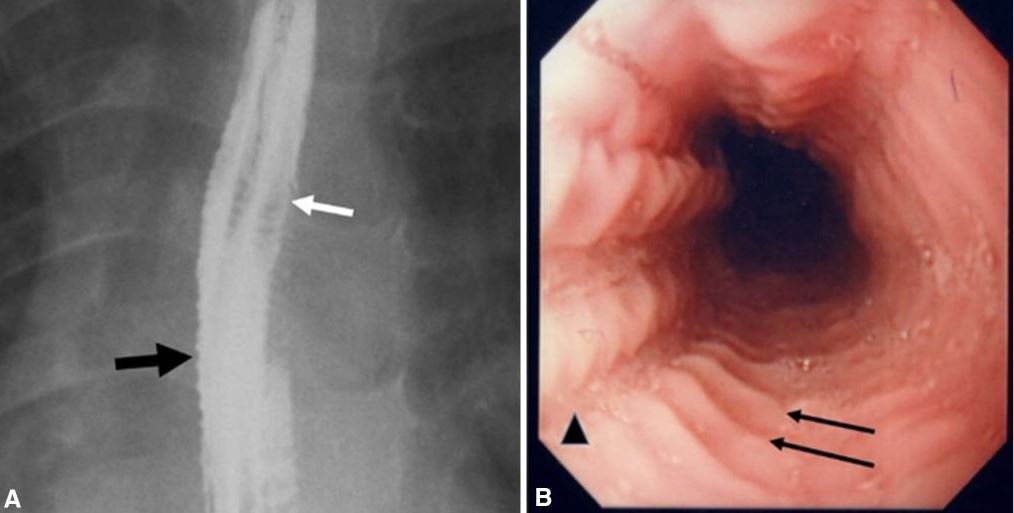
Images of eosinophilic esophagitis:
A. Esophagram in a patient with history of recurrent food impactions and dysphagia shows multiple esophageal rings (white arrow), giving the appearance of a corrugated or ringed esophagus, and mucosal irregularity (black arrow).
B. Endoscopy shows multiple transverse rings (arrows) and mucosal furrowing (arrowhead).
Upper endoscopy finding in a child with alkali ingestion: Pyloric stenosis developed 2 months after injury.
Image: “Pyloric stenosis after 2 months” by Dehghani SM, Aldaghi M, Javaherizadeh H. License: CC BY 3.0Reflux esophagitis is also known as gastroesophageal reflux disease Gastroesophageal Reflux Disease Gastroesophageal reflux disease (GERD) occurs when the stomach acid frequently flows back into the esophagus. This backwash (acid reflux) can irritate the lining of the esophagus, causing symptoms such as retrosternal burning pain (heartburn). Gastroesophageal Reflux Disease (GERD) ( GERD GERD Gastroesophageal reflux disease (GERD) occurs when the stomach acid frequently flows back into the esophagus. This backwash (acid reflux) can irritate the lining of the esophagus, causing symptoms such as retrosternal burning pain (heartburn). Gastroesophageal Reflux Disease (GERD)).
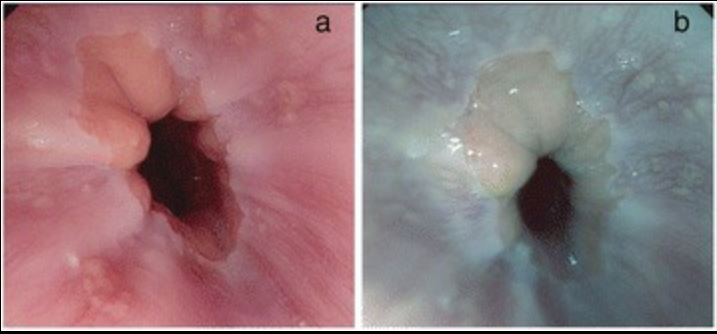
Reflux esophagitis in upper endoscopy:
A: high-definition image of esophageal changes in GERD
B: tone-enhancement image of GERD