A hemothorax is a collection of blood in the pleural cavity Pleural cavity Paired but separate cavity within the thoracic cavity. It consists of the space between the parietal and visceral pleura and normally contains a capillary layer of serous fluid that lubricates the pleural surfaces. Pleura: Anatomy. Hemothorax most commonly occurs due to damage to the intercostal arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology or from a lung laceration Laceration Torn, ragged, mangled wounds. Blunt Chest Trauma following chest trauma. Hemothorax can also occur as a complication of disease, or hemothorax may be spontaneous or iatrogenic Iatrogenic Any adverse condition in a patient occurring as the result of treatment by a physician, surgeon, or other health professional, especially infections acquired by a patient during the course of treatment. Anterior Cord Syndrome. Large hemothoraces can be life-threatening by leading to lung collapse. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea and chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. Physical exam findings include hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, decreased lung sounds, and dullness on percussion Percussion Act of striking a part with short, sharp blows as an aid in diagnosing the condition beneath the sound obtained. Pulmonary Examination of the chest. Diagnosis is by upright chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests. Management is with tube thoracostomy Tube Thoracostomy Surgical procedure involving the creation of an opening (stoma) into the chest cavity for drainage; used in the treatment of pleural effusion; pneumothorax; hemothorax; and empyema. Thoracic Surgery drainage, video-assisted thoracoscopic surgery (VATS), or thoracotomy Thoracotomy Surgical incision into the chest wall. Thoracic Surgery when massive hemothorax or persistent bleeding is present.
Last updated: Feb 19, 2025
A hemothorax is defined as a collection of fluid with a hematocrit Hematocrit The volume of packed red blood cells in a blood specimen. The volume is measured by centrifugation in a tube with graduated markings, or with automated blood cell counters. It is an indicator of erythrocyte status in disease. For example, anemia shows a low value; polycythemia, a high value. Neonatal Polycythemia of at least 50% accumulated in the potential space between the parietal Parietal One of a pair of irregularly shaped quadrilateral bones situated between the frontal bone and occipital bone, which together form the sides of the cranium. Skull: Anatomy and visceral pleura Visceral pleura Pleura: Anatomy of the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy.
The source of blood may be the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy, lung parenchyma, heart, or great vessels from either traumatic or non-traumatic causes.
Traumatic causes:
Non-traumatic causes:
Hemodynamic component:
Large volume loss (each hemothorax can contain up to 40% of total circulating blood volume) into the pleura Pleura The pleura is a serous membrane that lines the walls of the thoracic cavity and the surface of the lungs. This structure of mesodermal origin covers both lungs, the mediastinum, the thoracic surface of the diaphragm, and the inner part of the thoracic cage. The pleura is divided into a visceral pleura and parietal pleura. Pleura: Anatomy can lead to decreased cardiac function due to:
Respiratory component:
Blood collecting in the pleura Pleura The pleura is a serous membrane that lines the walls of the thoracic cavity and the surface of the lungs. This structure of mesodermal origin covers both lungs, the mediastinum, the thoracic surface of the diaphragm, and the inner part of the thoracic cage. The pleura is divided into a visceral pleura and parietal pleura. Pleura: Anatomy decreases the lung’s functional vital capacity Vital capacity The volume of air that is exhaled by a maximal expiration following a maximal inspiration. Ventilation: Mechanics of Breathing by:
Diagnosis is established by utilizing history, physical, and appropriate imaging. In cases of trauma, use of the primary survey Primary Survey Thoracic Trauma in Children is paramount to rapid diagnosis and treatment.
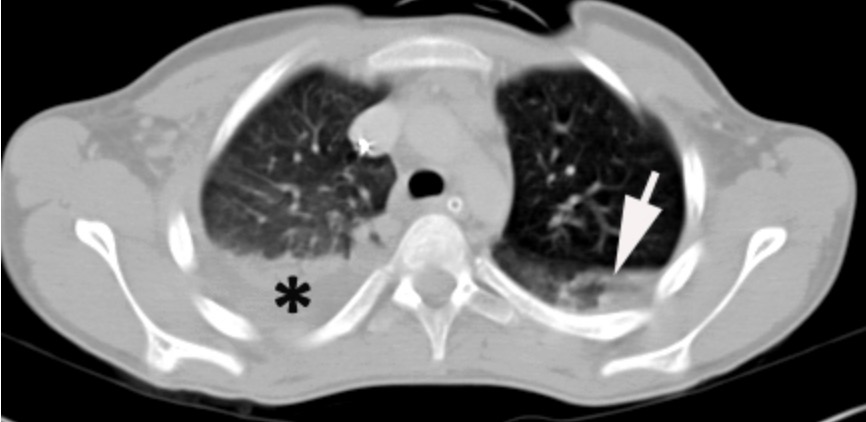
Chest CT showing a hemothorax in the right lung
Arrow indicates a lung contusion and a collection of fluid thought to be a hemothorax.
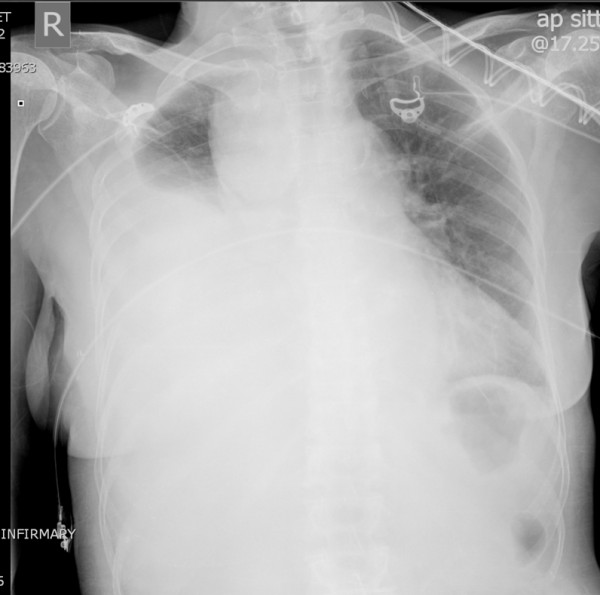
Massive right hemothorax
Chest X-ray showing a collection of fluid in the right pleural space, as illustrated by the opacified lung
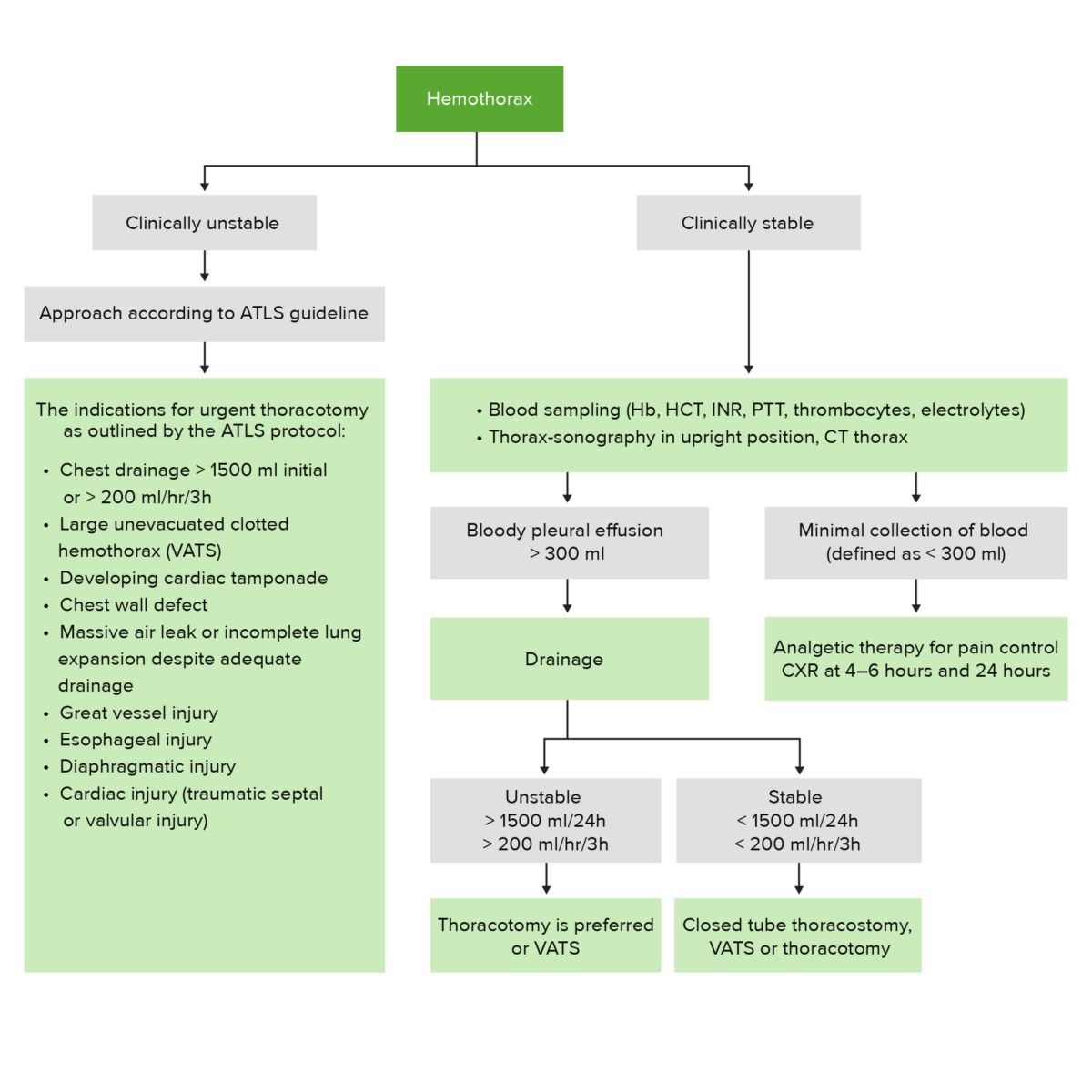
Hemothorax management algorithm
ATLS: Advanced Trauma Life Support
CXR: chest X-ray
Hb: hemoglobin
HCT: hematocrit
INR: international normalized ratio
PTT: prothrombin time
VATS: video-assisted thoracoscopic surgery
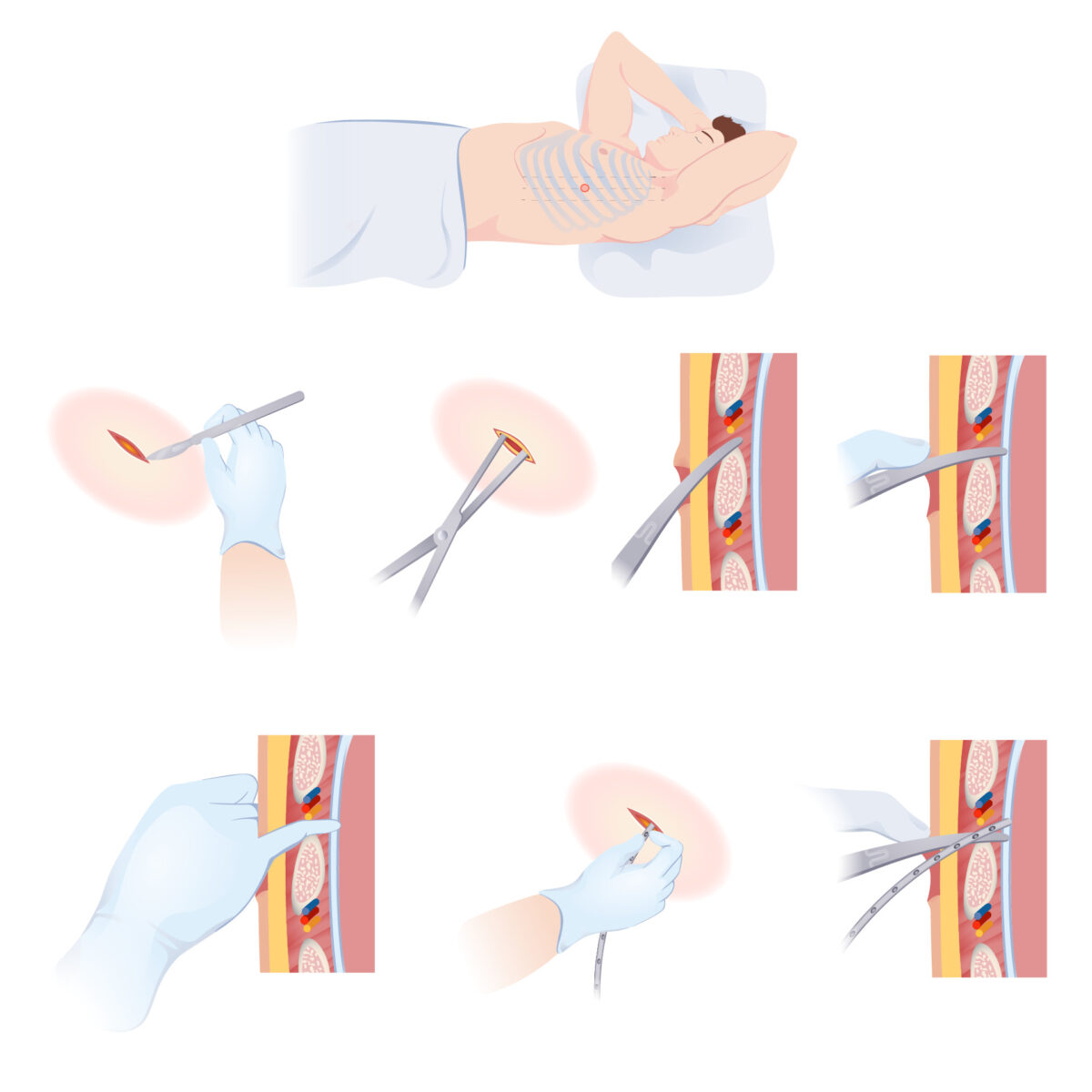
How to insert a chest tube
Stepwise illustration on how to insert a chest tube to drain fluid accumulation from the pleural space