Sepsis is defined as a life-threatening systemic response syndrome caused by viruses, bacteria, fungi, and parasites, or toxins released from these organisms. Neonates and children are particularly prone to sepsis owing to their immature immune systems. Affected individuals may present with localizing symptoms specific to a source of infection but may often complain of nonspecific systemic symptoms, such as confusion, lethargy, and fever. Diagnosis is based on history, exam, laboratory testing, and imaging studies. A high index of suspicion, rapid diagnosis, and clinical intervention with appropriate therapy are mandatory to achieve favorable outcomes.
Last updated: Feb 20, 2023
Sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock:
Severe sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock:
Septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock is severe sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock that is unresponsive to fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome.
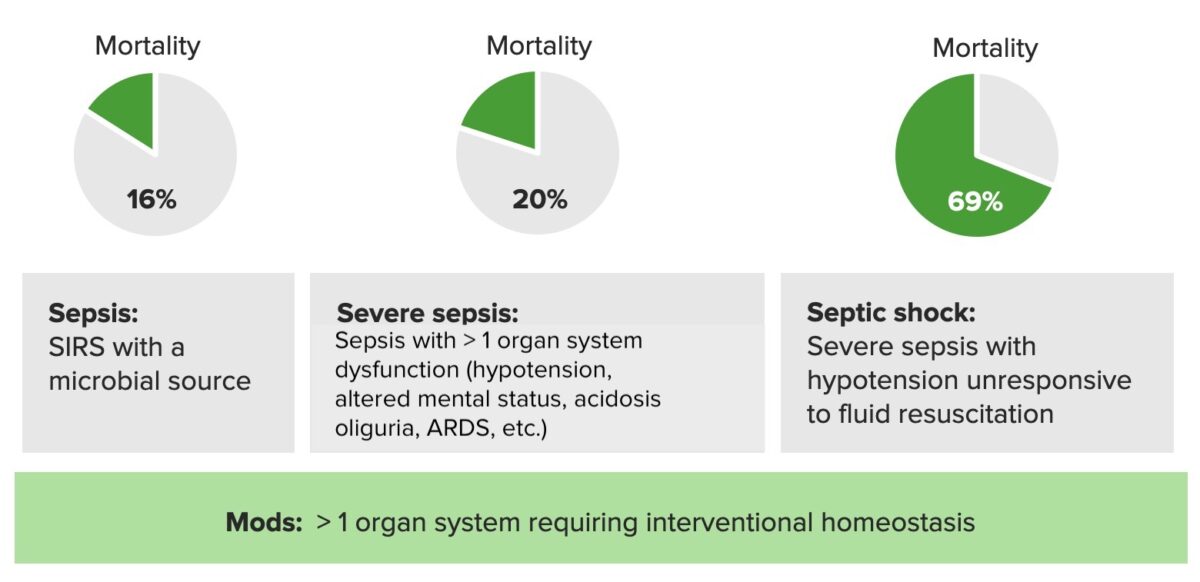
Mortality rates in sepsis, severe sepsis, and septic shock:
SIRS: systemic inflammatory response syndrome
ARDS: acute respiratory distress syndrome
The host’s ability to resist direct damage by the pathogen and immune system Immune system The body’s defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs response determines if an infection can be controlled or will result in sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock.
| Initial phase | Septic phase | Late phase |
|---|---|---|
|
|
|