Pseudomonas is a non-lactose-fermenting, gram-negative bacillus Bacillus Bacillus are aerobic, spore-forming, gram-positive bacilli. Two pathogenic species are Bacillus anthracis (B. anthracis) and B. cereus. Bacillus that produces pyocyanin, which gives it a characteristic blue-green color. Pseudomonas is found ubiquitously in the environment, as well as in moist reservoirs, such as hospital sinks and respiratory equipment. Pseudomonas has a sweet, grape-like odor. The most clinically relevant species is Pseudomonas aeruginosa (P. aeruginosa), which has a wide array of clinical manifestations from benign Benign Fibroadenoma diseases, such as swimmer’s ear Swimmer’s ear Otitis exteRNA (also known as external otitis or swimmer's ear) is an infection of the external auditory canal that is most often caused by acute bacterial infection and is frequently associated with hot, humid weather and water exposure. Patients commonly present with ear pain, pruritus, discharge, and hearing loss. Otitis Externa and “hot tub” folliculitis, to disseminated bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides and osteomyelitis Osteomyelitis Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus. Osteomyelitis. Risk factors for infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease include: neutropenia Neutropenia Neutrophils are an important component of the immune system and play a significant role in the eradication of infections. Low numbers of circulating neutrophils, referred to as neutropenia, predispose the body to recurrent infections or sepsis, though patients can also be asymptomatic. Neutropenia, cystic Cystic Fibrocystic Change fibrosis Fibrosis Any pathological condition where fibrous connective tissue invades any organ, usually as a consequence of inflammation or other injury. Bronchiolitis Obliterans, asplenia Asplenia Asplenia is the absence of splenic tissue or function and can stem from several factors ranging from congenital to iatrogenic. There is a distinction between anatomic asplenia, which is due to the surgical removal of the spleen, and functional asplenia, which is due to a condition that leads to splenic atrophy, infarct, congestion, or infiltrative disease. Asplenia, burn injuries, and indwelling catheters/endotracheal intubation Intubation Peritonsillar Abscess. Management is primarily with piperacillin Piperacillin Semisynthetic, broad-spectrum, ampicillin derived ureidopenicillin antibiotic proposed for pseudomonas infections. It is also used in combination with other antibiotics. Penicillins/ tazobactam Tazobactam A penicillanic acid and sulfone derivative and potent beta-lactamase inhibitor that enhances the activity of other anti-bacterial agents against beta-lactamase producing bacteria. Cephalosporins.
Last updated: Sep 8, 2022
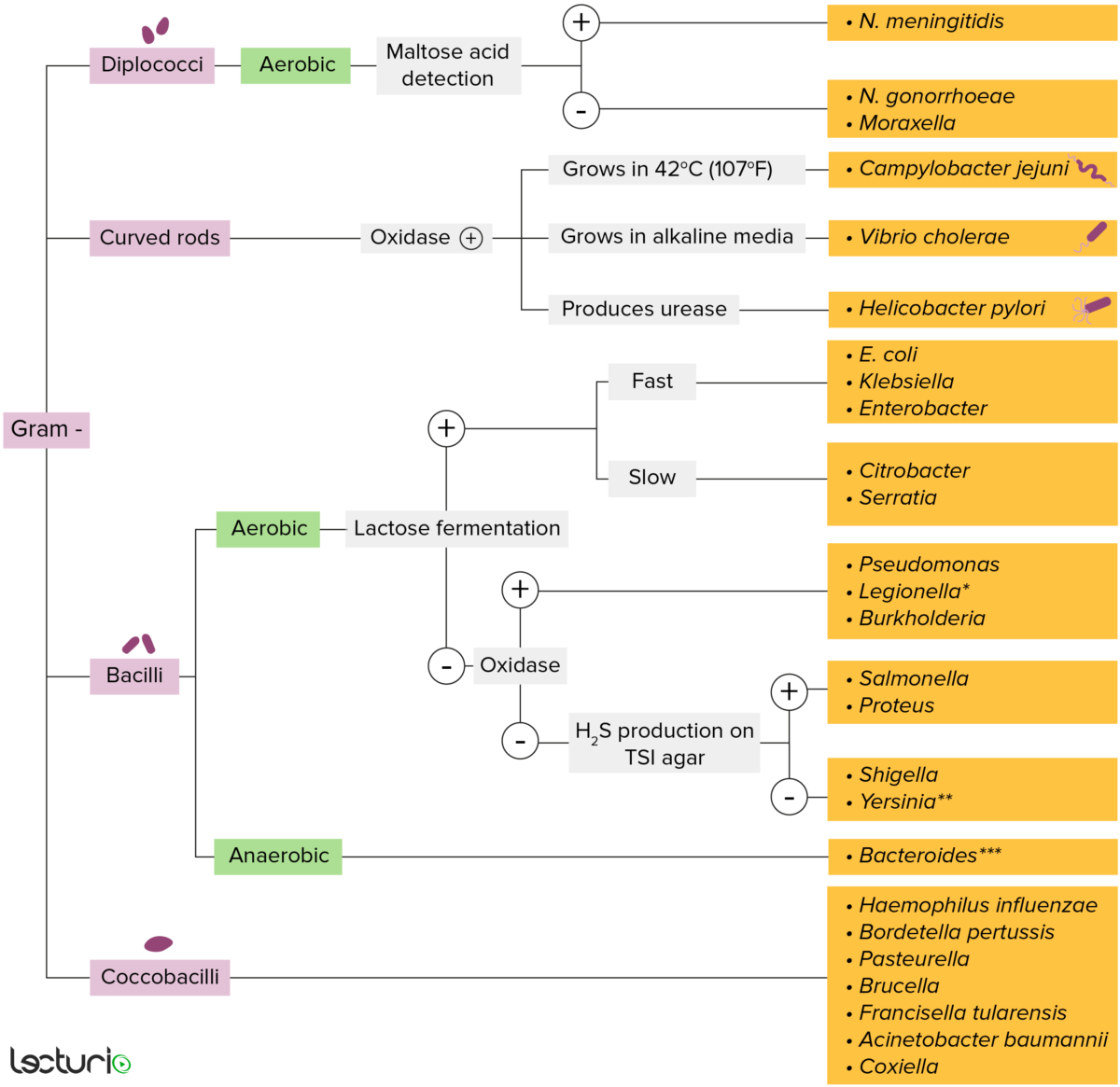
Gram-negative bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thin layer of peptidoglycan do not retain the crystal violet stain utilized in Gram staining. These bacteria do, however, retain the safranin counterstain and thus appear as pinkish-red on the stain, making them gram negative. These bacteria can be further classified according to morphology (diplococci, curved rods, bacilli, and coccobacilli) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The bacteria can be more narrowly identified by growing them on specific media (triple sugar iron (TSI) agar) where their enzymes can be identified (urease, oxidase) and their ability to ferment lactose can be tested.
* Stains poorly on Gram stain
** Pleomorphic rod/coccobacillus
*** Require special transport media

Photograph depicts the colonial growth pattern displayed by Pseudomonas aeruginosa bacteria.
Image: “6688” by the CDC/Dr. Theo Hawkins. License: Public domain.Reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli:
Transmission:
| Virulence Virulence The degree of pathogenicity within a group or species of microorganisms or viruses as indicated by case fatality rates and/or the ability of the organism to invade the tissues of the host. The pathogenic capacity of an organism is determined by its virulence factors. Proteus factor | Effect |
|---|---|
| Polysaccharide capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides |
|
| Pili Pili Filamentous or elongated proteinaceous structures which extend from the cell surface in gram-negative bacteria that contain certain types of conjugative plasmid. These pili are the organs associated with genetic transfer and have essential roles in conjugation. Normally, only one or a few pili occur on a given donor cell. This preferred use of ‘pili’ refers to the sexual appendage, to be distinguished from bacterial fimbriae, also known as common pili, which are usually concerned with adhesion. Salmonella |
|
| Phospholipase C |
|
| Exotoxin A |
|
| Pyocyanin |
|
| Type III secretion Secretion Coagulation Studies system |
|
| In vivo biofilm Biofilm Encrustations formed from microbes (bacteria, algae, fungi, plankton, or protozoa) embedded in an extracellular polymeric substance matrix that is secreted by the microbes. They occur on body surfaces such as teeth (dental deposits); inanimate objects, and bodies of water. Biofilms are prevented from forming by treating surfaces with dentifrices; disinfectants; anti-infective agents; and anti-fouling agents. Staphylococcus formation |
|
| ꞵ-lactamase and efflux pumps Efflux Pumps Lincosamides |
|
| Type of condition | Characteristics |
|---|---|
| Urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy infection |
|
| Burn wound infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease |
Associated with burn injuries, causing:
|
| Ear infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease |
Otitis externa
Otitis externa
Otitis externa (also known as external otitis or swimmer’s ear) is an infection of the external auditory canal that is most often caused by acute bacterial infection and is frequently associated with hot, humid weather and water exposure. Patients commonly present with ear pain, pruritus, discharge, and hearing loss.
Otitis Externa:
|
| Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease |
Ecthyma
Ecthyma
An ulcerative pyoderma usually caused by group a beta-hemolytic streptococcal infection at the site of minor trauma.
Impetigo gangrenosum:
|
| Pulmonary infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease |
|
| Eye infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease |
Occurs in contact
lens
Lens
A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation.
Eye: Anatomy wearers or minor eye trauma:
|
| Disseminated infections Disseminated infections IL-12 Receptor Deficiency |
Occurs in
immunocompromised
immunocompromised
A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation.
Gastroenteritis hosts:
|
| Osteomyelitis Osteomyelitis Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus. Osteomyelitis |
|

A lateral neck radiograph showing epiglottitis and complete obstruction of the airways in a 5-year-old girl. The condition is commonly caused by the Haemophilus influenzae bacteria.
Image: “Acute epiglottitis as the initial presentation of pediatric Systemic Lupus Erythematosus” by Charuvanij S et al. License: CC BY 2.0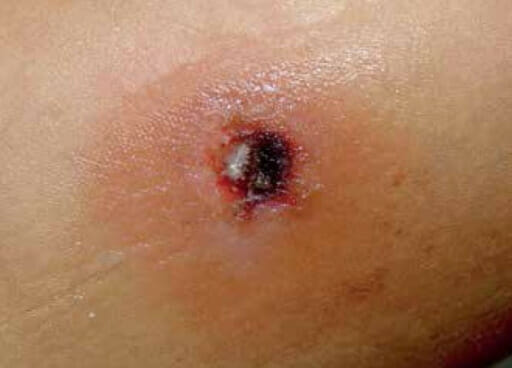
Image showing Ecthyma Gangrenosum due to pseudomonas bacteria in an immunocompromised child
Image: “A single black ulcer in a child with acute lymphocytic leukemia” by Michelangelo Vestita et al. License: CC BY 4.0To help remember the many clinically relevant facts about Pseudomonas, use the mnemonic “PSEUDOMONAS”: