Proteus spp. are gram-negative, facultatively anaerobic bacilli Bacilli Shigella. Different types of infection result from Proteus, but the urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy is the most common site. The majority of cases are caused by Proteus mirabilis (P. mirabilis). The bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology are part of the normal intestinal flora and are also found in the environment. Proteus spp. exhibit a characteristic swarming motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility and strong urease Urease An enzyme that catalyzes the conversion of urea and water to carbon dioxide and ammonia. Nocardia/Nocardiosis activity, which enable initiation of infection. Hydrolysis Hydrolysis The process of cleaving a chemical compound by the addition of a molecule of water. Proteins and Peptides of urea Urea A compound formed in the liver from ammonia produced by the deamination of amino acids. It is the principal end product of protein catabolism and constitutes about one half of the total urinary solids. Urea Cycle by urease Urease An enzyme that catalyzes the conversion of urea and water to carbon dioxide and ammonia. Nocardia/Nocardiosis leads to alkaline urine with an ammonia-like odor. With the elevated pH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance in the urine, struvite Struvite The mineral magnesium ammonium phosphate with the formula NH4mgpo4. It is associated with urea-splitting organisms in a high magnesium, high phosphate, alkaline environment. Accumulation of crystallized struvite is found in the urinary tract as struvite calculi and as scale on sewage system equipment and wastewater pipes. Nephrolithiasis renal stones form, which eventually can cause obstruction and renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome. Treatment is with antibiotics (e.g., trimethoprim-sulfamethoxazole) for the infection and surgical removal of the stones, if present.
Last updated: Jan 7, 2025
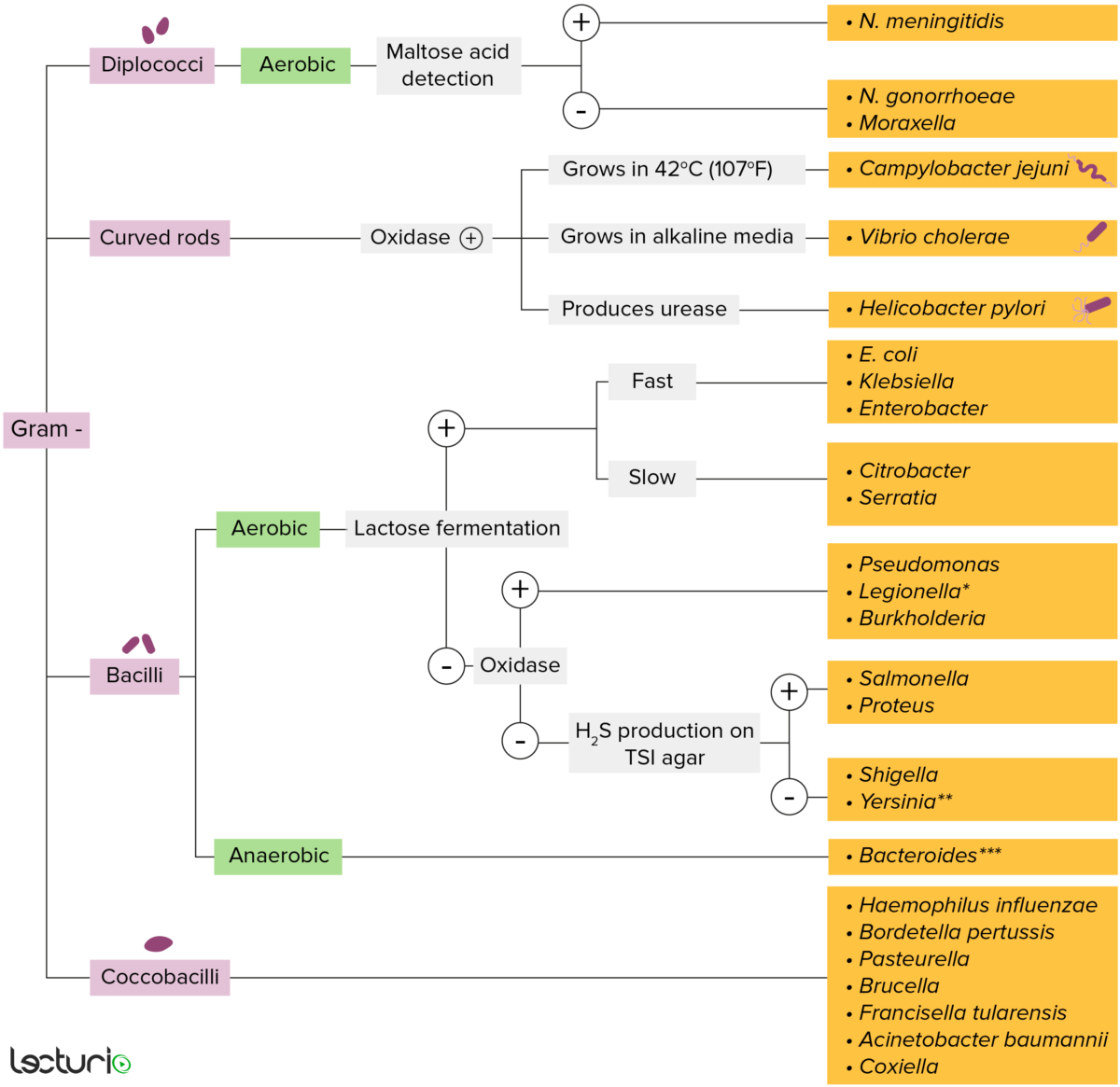
Gram-negative bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thin layer of peptidoglycan do not retain the crystal violet stain utilized in Gram staining. These bacteria do, however, retain the safranin counterstain and thus appear as pinkish-red on the stain, making them gram negative. These bacteria can be further classified according to morphology (diplococci, curved rods, bacilli, and coccobacilli) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The bacteria can be more narrowly identified by growing them on specific media (triple sugar iron (TSI) agar) where their enzymes can be identified (urease, oxidase) and their ability to ferment lactose can be tested.
* Stains poorly on Gram stain
** Pleomorphic rod/coccobacillus
*** Require special transport media
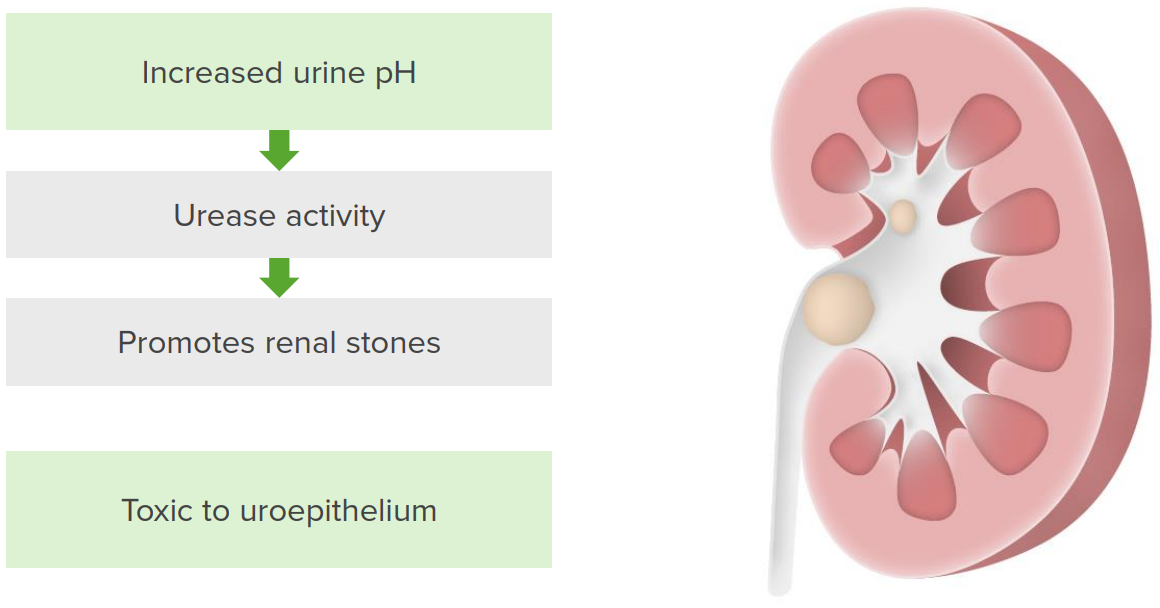
Pathogenesis of Proteus infection
The bacteria increase urine pH by enhancing urease activity. Urease metabolizes urea into ammonia and carbon dioxide. These byproducts increase the pH of the urine, predisposing the patient to struvite stone formation. The stone and bacterial infection lead to uroepithelial damage.
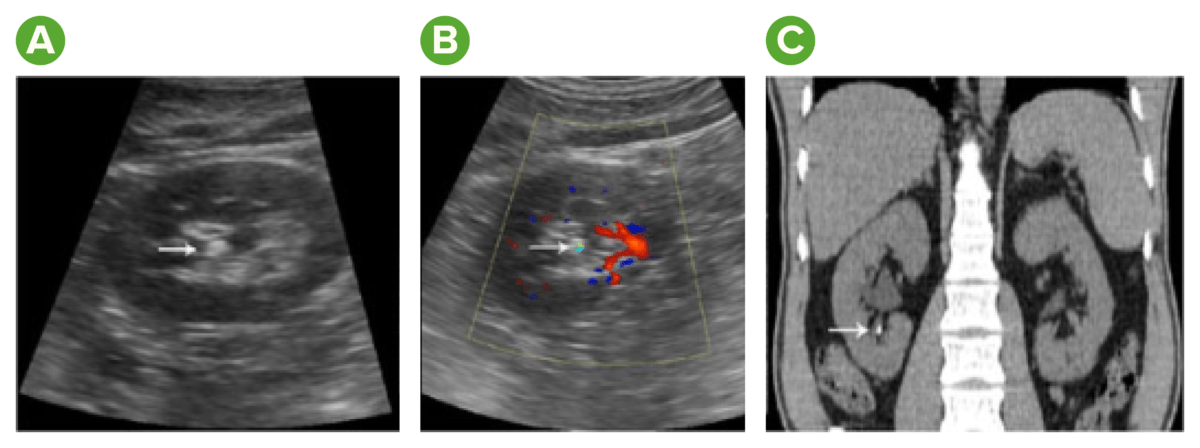
Image:
A) Gray-scale sonogram showing a hyperechoic spot with posterior acoustic shadowing
B) Color Doppler sonogram showing a twinkling sign
C) CT showing renal stones
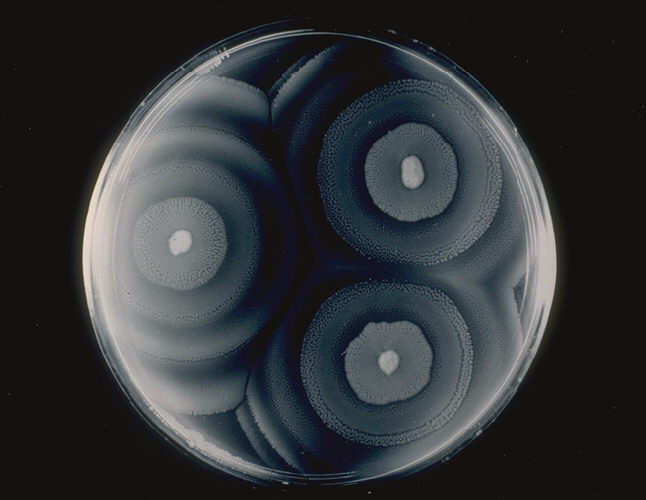
Proteus mirabilis: culture illustrating the swarming phenomenon
Image: “ProteusMirabilis Schwärmen” by the CDC. License: Public domain.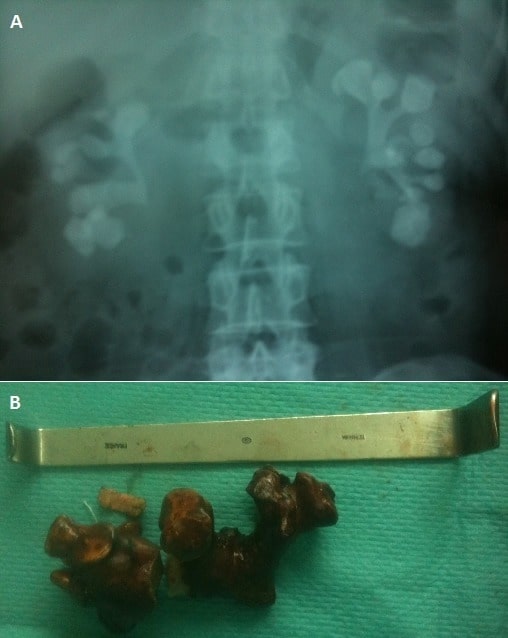
Staghorn calculi from a Proteus infection
A: abdominal X-ray showing bilateral complete staghorn calculi
B: part of the staghorn calculi extracted via open surgery
Escherichia coli Escherichia coli The gram-negative bacterium Escherichia coli is a key component of the human gut microbiota. Most strains of E. coli are avirulent, but occasionally they escape the GI tract, infecting the urinary tract and other sites. Less common strains of E. coli are able to cause disease within the GI tract, most commonly presenting as abdominal pain and diarrhea. Escherichia coli (E. coli) and Proteus spp. are common etiologies of urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy infection.
| Proteus spp. | E. coli | |
|---|---|---|
| Characteristics | Gram-negative bacilli Bacilli Shigella | Gram-negative bacilli Bacilli Shigella |
| Habitat | Intestinal tract | Intestinal tract |
| Lactose fermentation | Non-lactose fermenting | Lactose fermenting |
| Indole | P. mirabilis: negative P. vulgaris: positive | Positive |
| TSI TSI Shigella agar | Produce H2S | Does not produce H2S |
| Infection | UTI UTI Urinary tract infections (UTIs) represent a wide spectrum of diseases, from self-limiting simple cystitis to severe pyelonephritis that can result in sepsis and death. Urinary tract infections are most commonly caused by Escherichia coli, but may also be caused by other bacteria and fungi. Urinary Tract Infections (UTIs) | Most common cause of UTI UTI Urinary tract infections (UTIs) represent a wide spectrum of diseases, from self-limiting simple cystitis to severe pyelonephritis that can result in sepsis and death. Urinary tract infections are most commonly caused by Escherichia coli, but may also be caused by other bacteria and fungi. Urinary Tract Infections (UTIs) |