The gram-negative bacterium Escherichia coli is a key component of the human gut microbiota. Most strains of E. coli are avirulent, but occasionally they escape the GI tract, infecting the urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy and other sites. Less common strains of E. coli are able to cause disease within the GI tract, most commonly presenting as abdominal pain Abdominal Pain Acute Abdomen and diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea. E. coli is transmitted via a fecal–oral route, which can occur with unsanitary food preparation, contamination of meat or produce by manure, irrigating or washing crops/fruits with contaminated water, and consumption of contaminated water.
Last updated: Apr 22, 2025
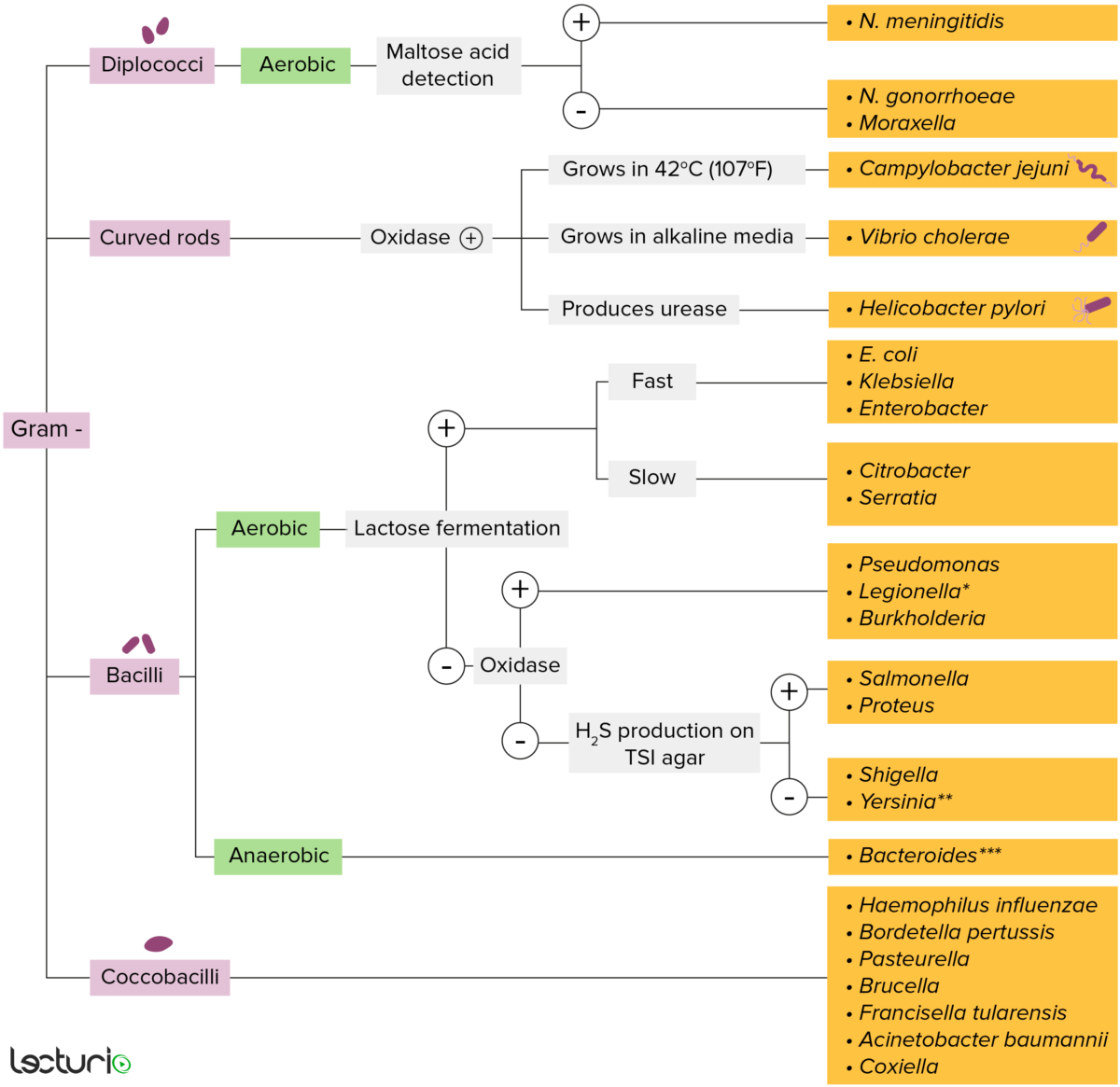
Gram-negative bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thin layer of peptidoglycan do not retain the crystal violet stain utilized in Gram staining. These bacteria do, however, retain the safranin counterstain and thus appear as pinkish-red on the stain, making them gram negative. These bacteria can be further classified according to morphology (diplococci, curved rods, bacilli, and coccobacilli) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The bacteria can be more narrowly identified by growing them on specific media (triple sugar iron (TSI) agar) where their enzymes can be identified (urease, oxidase) and their ability to ferment lactose can be tested.
* Stains poorly on Gram stain
** Pleomorphic rod/coccobacillus
*** Require special transport media
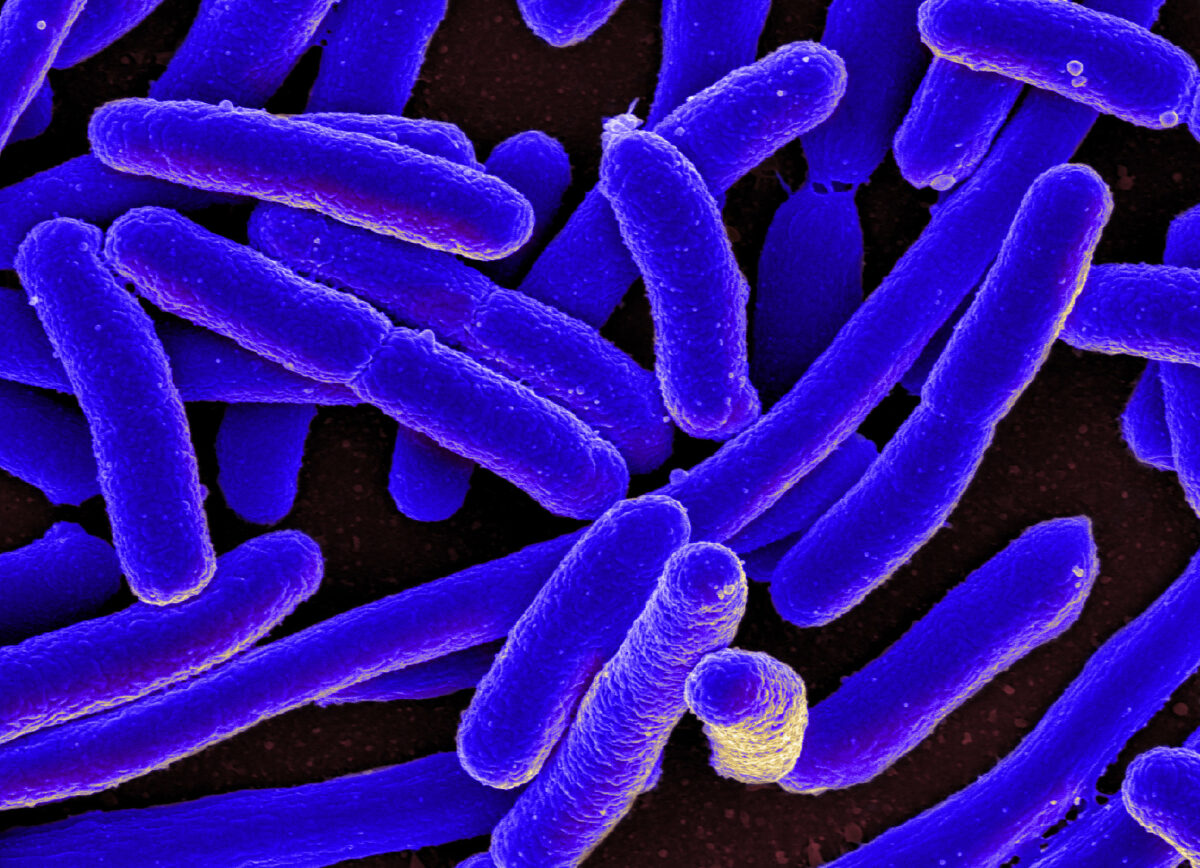
Photomicrograph of Escherichia coli
Image: “E. coli Bacteria” by NIAID. License: CC BY 2.0| Pathogen | Pathogenesis/ Virulence Virulence The degree of pathogenicity within a group or species of microorganisms or viruses as indicated by case fatality rates and/or the ability of the organism to invade the tissues of the host. The pathogenic capacity of an organism is determined by its virulence factors. Proteus factor | Signs and Symptoms |
|---|---|---|
| ETEC |
|
No inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation or invasion → traveler’s diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea (watery) |
| EPEC |
|
Mild inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation → watery diarrhea Watery diarrhea Rotavirus with mucus |
| EAEC |
|
Mild inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation → watery diarrhea Watery diarrhea Rotavirus |
| EHEC |
|
Severe inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation → dysentery Dysentery Acute inflammation of the intestine associated with infectious diarrhea of various etiologies, generally acquired by eating contaminated food containing toxins, biological derived from bacteria or other microorganisms. Dysentery is characterized initially by watery feces then by bloody mucoid stools. It is often associated with abdominal pain; fever; and dehydration. Gastroenteritis ( bloody diarrhea Bloody diarrhea Diarrhea) |
| EIEC | Direct invasion of the intestinal epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology and formation of enterotoxins → necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage and inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation | Severe inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation → dysentery Dysentery Acute inflammation of the intestine associated with infectious diarrhea of various etiologies, generally acquired by eating contaminated food containing toxins, biological derived from bacteria or other microorganisms. Dysentery is characterized initially by watery feces then by bloody mucoid stools. It is often associated with abdominal pain; fever; and dehydration. Gastroenteritis ( bloody diarrhea Bloody diarrhea Diarrhea) similar to Shigella Shigella Shigella is a genus of gram-negative, non-lactose-fermenting facultative intracellular bacilli. Infection spreads most commonly via person-to-person contact or through contaminated food and water. Humans are the only known reservoir. Shigella |

ETEC attaches via colonization factor antigen or CFA (adhesion). The heat stable (ST) enterotoxin causes cGMP accumulation in cells, and secretion of fluid and electrolytes into the intestinal lumen. The heat labile (LT) enterotoxin acts like cholera toxin, which increases cAMP by activating adenylyl cyclase (AC). General effect is water and chloride hypersecretion and inhibited sodium reabsorption. Non-invasive enterotoxins remain within the intestinal lumen and do not invade the epithelial cells.
Image by Lecturio.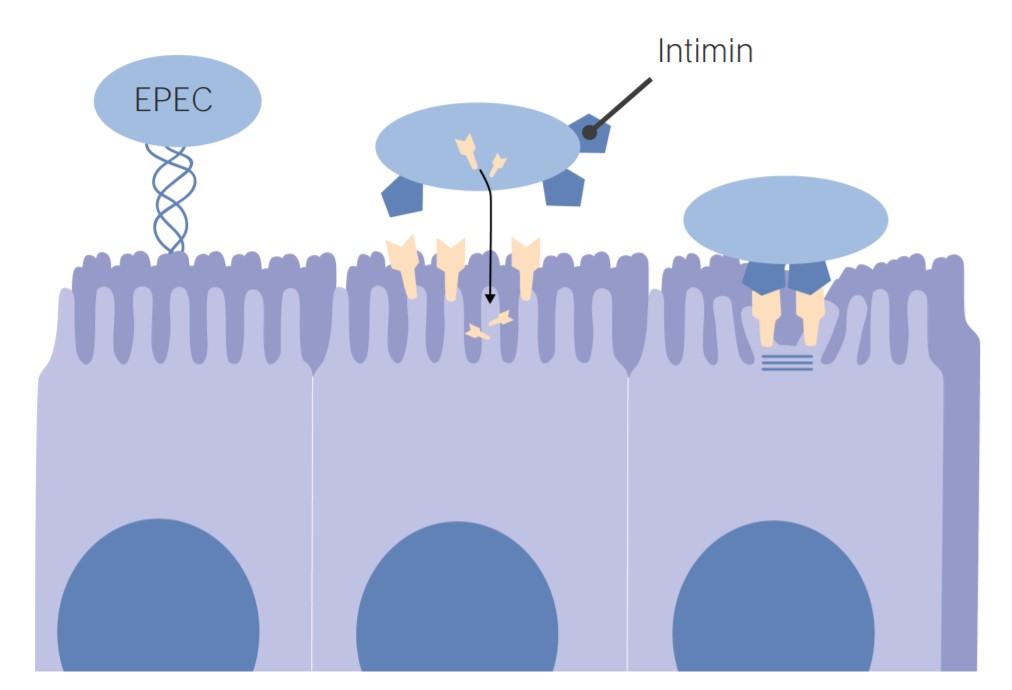
EPEC Pathogenesis:
EPEC uses intimin adhesion molecules to adhere to the intestinal cells. Binding causes cell deformation (brush border degeneration and loss of microvilli).The characteristic effect of attachment and effacement is thought to be the primary cause of diarrhea.