Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Uremia refers specifically to the constellation of symptoms that occur with severe renal dysfunction. The etiologies of AKI are classified as prerenal, intrinsic renal, or post-renal, and there is a varied clinical presentation depending on the severity of kidney dysfunction. Acute kidney injury is diagnosed initially by a change in serum creatinine levels, and then the etiology is determined by clinical history, lab testing, imaging, and possibly kidney biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. The management of AKI depends on the etiology; however, attention Attention Focusing on certain aspects of current experience to the exclusion of others. It is the act of heeding or taking notice or concentrating. Psychiatric Assessment to the individual's volume status Volume Status ACES and RUSH: Resuscitation Ultrasound Protocols and serum electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes is always important. If management is unsuccessful and AKI progresses to CKD CKD Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease, then renal replacement therapy with dialysis Dialysis Renal replacement therapy refers to dialysis and/or kidney transplantation. Dialysis is a procedure by which toxins and excess water are removed from the circulation. Hemodialysis and peritoneal dialysis (PD) are the two types of dialysis, and their primary difference is the location of the filtration process (external to the body in hemodialysis versus inside the body for PD). Peritoneal Dialysis and Hemodialysis or kidney transplantation Kidney Transplantation The transference of a kidney from one human or animal to another. Organ Transplantation is necessary.
Last updated: May 17, 2024
Acute kidney injury refers to an abrupt decrease in kidney function, manifested by an increase in serum creatinine level, with or without reduced urine output.
Previously there had been more than 30 definitions of “acute renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome” in the literature, and these have been updated to the term AKI.
The causes of AKI are commonly organized into prerenal, intrinsic renal, or postrenal etiologies. With prerenal and postrenal causes, the kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy have normal anatomy and the injury is due to the effects of the inciting factor.
Acute kidney injury can present with a wide range of symptoms, from being asymptomatic with only laboratory abnormalities to being comatose Comatose A profound state of unconsciousness associated with depressed cerebral activity from which the individual cannot be aroused. Coma generally occurs when there is dysfunction or injury involving both cerebral hemispheres or the brain stem reticular formation. Hyponatremia due to severe uremia.
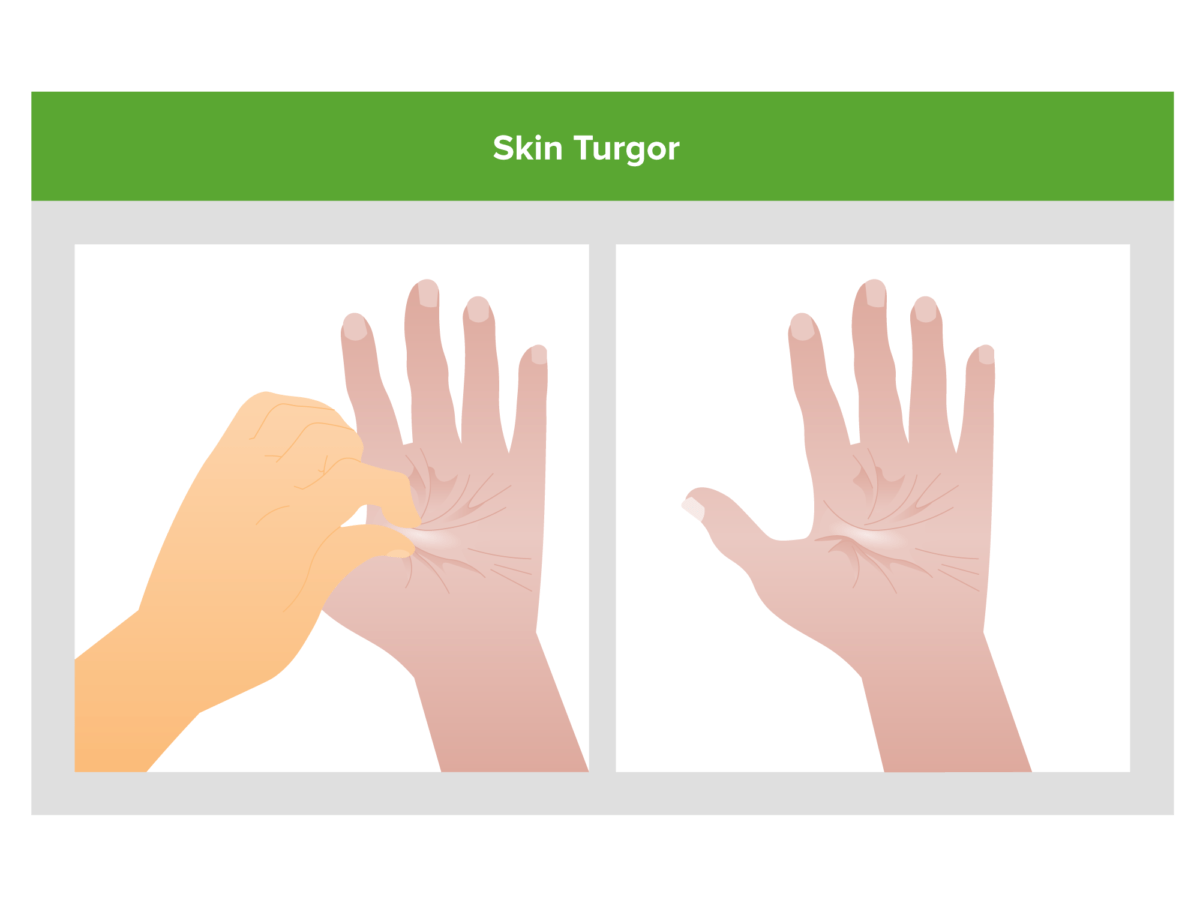
Poor skin turgor (skin remains tented after being pinched) is a potential clue that volume depletion may be the cause of an individual’s acute kidney injury.
Image by Lecturio.
Lower extremity edema: may be seen in individuals presenting with hypervolemia as a result of acute kidney injury
Image: “Leg Edema 01” by Wang Kai-feng, Pan Hong-ming, Lou Hai-zhou, Shen Li-rong, Zhu Xi-yan. License: CC BY 2.0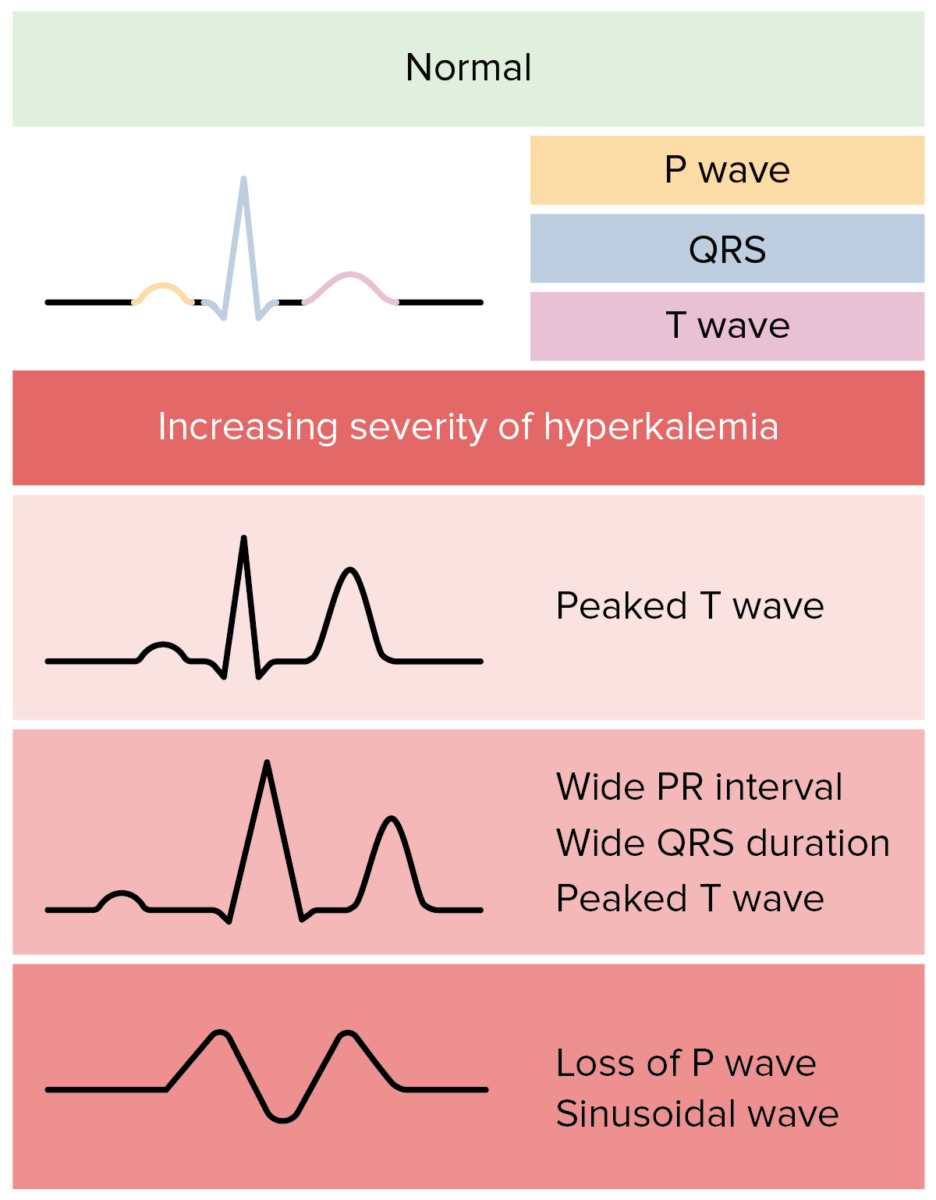
Possible ECG changes due to hyperkalemia in individuals with acute kidney injury:
In reality, ECG changes in hyperkalemia are more variable and less predictable.
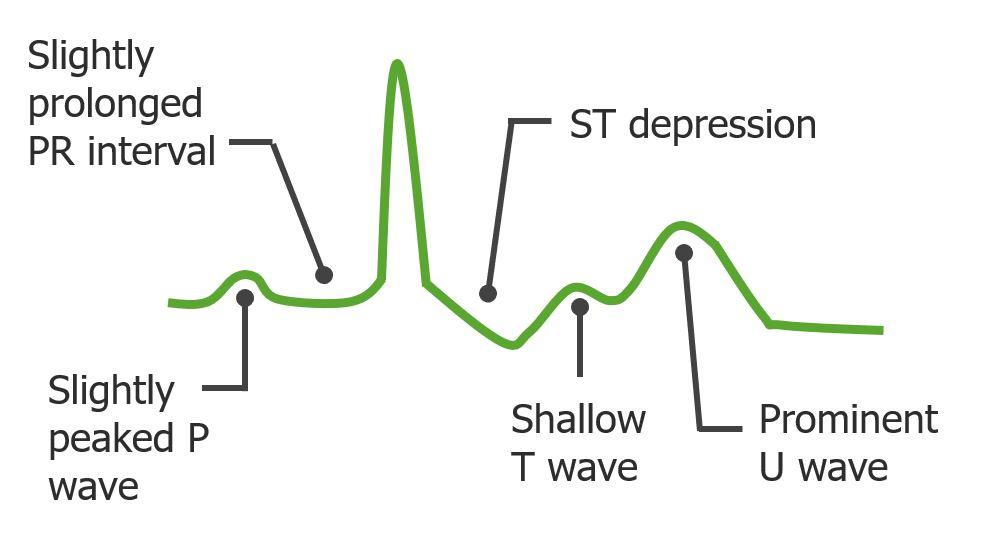
Possible ECG changes in individuals with acute kidney injury presenting with hypokalemia
Image by Lecturio. License: CC BY-NC-SA 4.0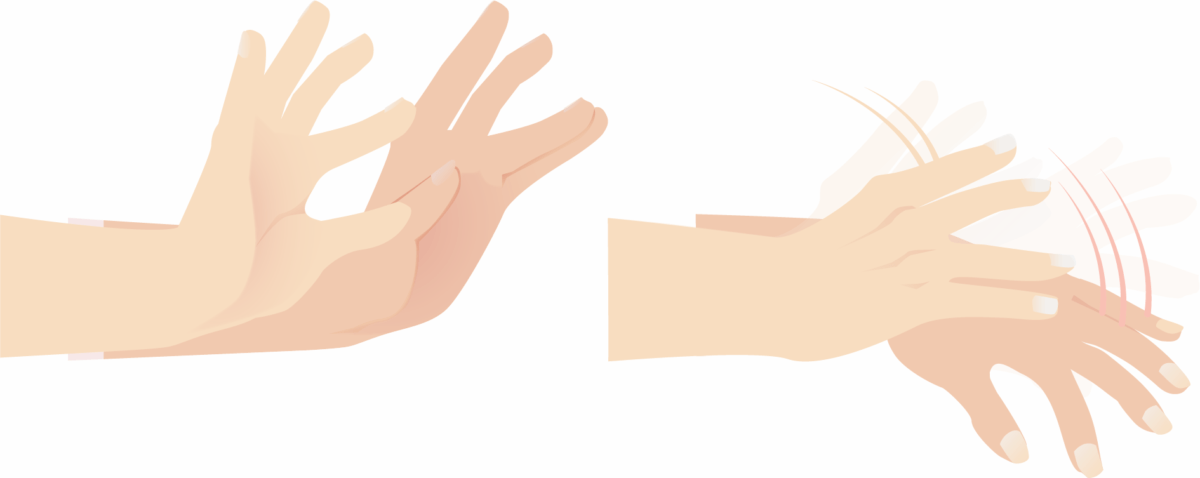
Asterixis: a potential examination finding in an individual with uremia from acute kidney injury
Image by Lecturio.
Variable-sized macules and patches of erythematous on an individual with acute interstitial nephritis
Image: “F1: Gross and microscopic exam of the skin.” by Ha Yeon Kim, Sung Sun Kim, Soo Hyeon Bae, Eun Hui Bae, Seong Kwon Ma & Soo Wan Kim. License: CC BY 4.0, cropped by Lecturio.Acute tubular necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage follows a characteristic clinical course involving 3 phases.
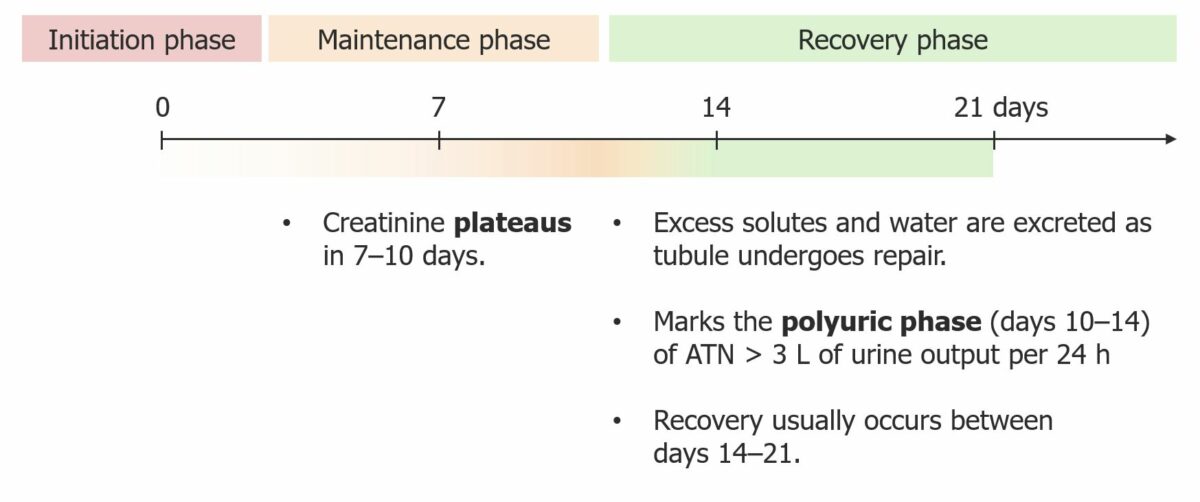
Clinical course of acute tubular necrosis (ATN)
Image by Lecturio. License CC BY-NC-SA 4.0The diagnosis of AKI includes identifying inciting factors and determining if the etiology is prerenal, intrarenal, or postrenal, in order to plan appropriate treatment.
Consider other specific testing for less common etiologies:
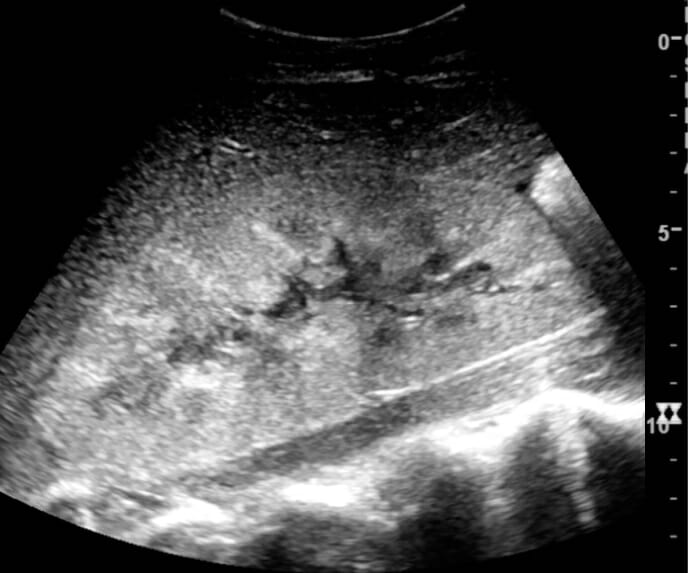
Ultrasound image showing increased cortical echogenicity and enlarged kidney:
Further biopsy showed acute tubular necrosis.

Ultrasound image showing hydronephrosis of the left kidney due to a ureteral stone
Image: “Hydro” by morning2k. License: CC BY 2.5| Prerenal | Renal (ATN) | |
|---|---|---|
| Specific gravity | ≥ 1.020 | ≤ 1.010 |
| Urine osmolality Osmolality Plasma osmolality refers to the combined concentration of all solutes in the blood. Renal Sodium and Water Regulation (mOsm/kg) | > 500 | < 350 |
| Urine sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia (mEq/L) | < 20 | > 20 |
| FENa | < 1% | > 1% |
| Urine protein | Minimal | Minimal to severe, depending on etiology |
| Finding | Significance |
|---|---|
| Renal tubular cells | Acute tubular injury |
| RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology | Nonglomerular bleeding/anywhere in the urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy |
| Dysmorphic red cells | Glomerular disease |
| Red cell casts | Diagnostic of glomerular disease |
| Leukocytes Leukocytes White blood cells. These include granular leukocytes (basophils; eosinophils; and neutrophils) as well as non-granular leukocytes (lymphocytes and monocytes). White Myeloid Cells: Histology/WBCs | Urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy infection |
| White cell casts | Renal infection |
| Hyaline casts | Any type of renal disease |
| Granular casts | More significant renal disease |
| “Muddy brown cast” | Necrotic tubular cells/acute tubular injury |
The etiology of AKI dictates the treatment; further testing with biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma may be indicated after appropriate workup and treatment for hypovolemia Hypovolemia Sepsis in Children or fluid overload are completed.