African trypanosomiasis, or African sleeping sickness, is a parasitic infection caused by the protozoa Protozoa Nitroimidazoles Trypanosoma brucei. There are 2 notable subtypes, T. brucei gambiense and T. brucei rhodesiense. Transmission is primarily vector borne through the tsetse fly. Initial infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease present with localized inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation ( chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis), cervical lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy, intermittent fevers, and other nonspecific findings. If untreated, CNS involvement occurs, which is characterized by sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep disturbances, behavioral changes, coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma, and death. Diagnosis is confirmed by the identification Identification Defense Mechanisms of trypanosomes on blood smear Blood smear Myeloperoxidase Deficiency or serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus. Treatment is dependent on the subtype and stage of the disease. Early treatment and prevention are key in preventing long-term sequelae and death.
Last updated: Sep 19, 2022
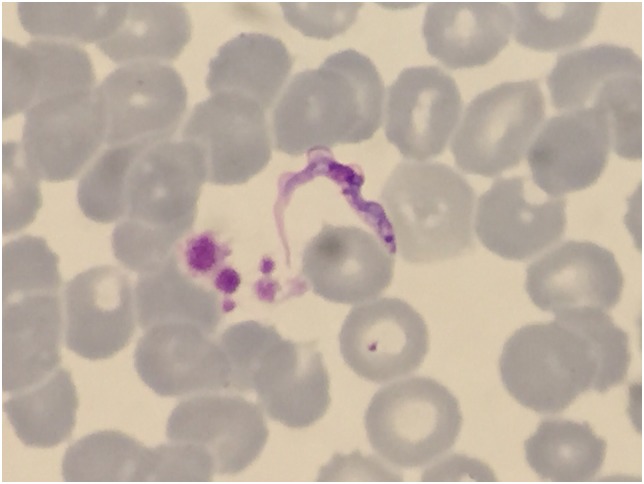
Trypanosomes in a Giemsa-stained thin blood film from a traveler returning from Tanzania
Image: “Trypanosomes in a Giemsa-stained thin blood film from a Spanish traveler returning from Tanzania” by Joan Gómez-Junyent et al. License: CC BY 4.0T. brucei causes African trypanosomiasis, also known as African sleeping sickness.
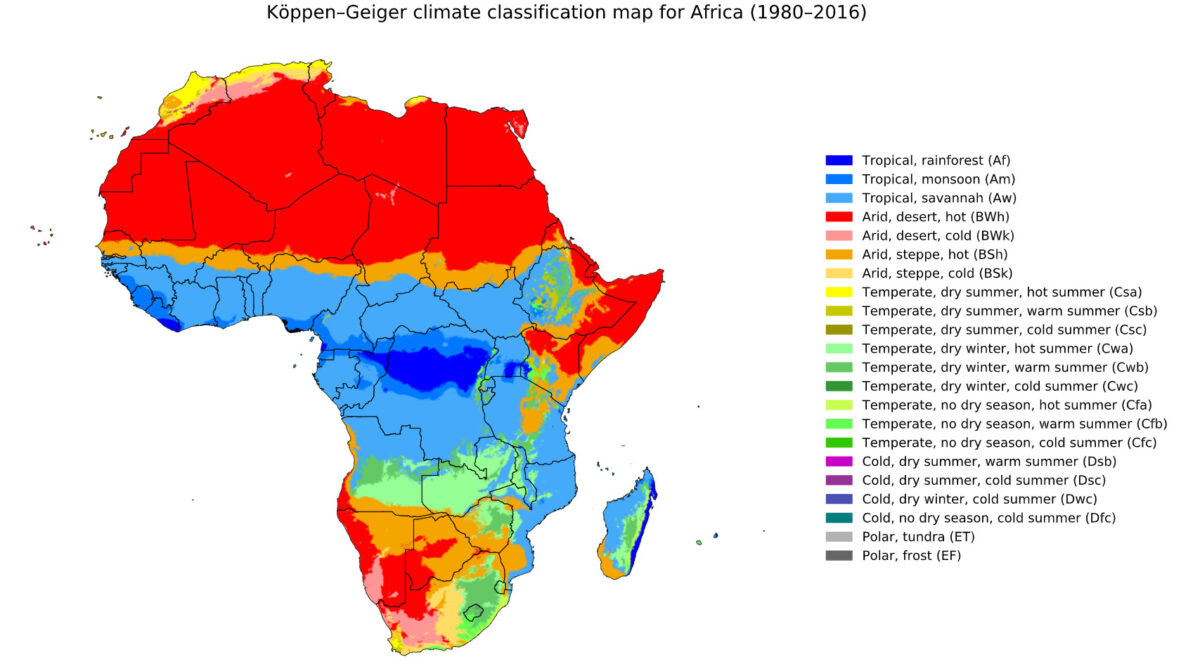
Geographic distribution of African trypanosomiasis: T. brucei is only found in the blue areas.
Image: “T. brucei is only found in the blue areas” by Beck, H.E. et al. License: CC BY 4.0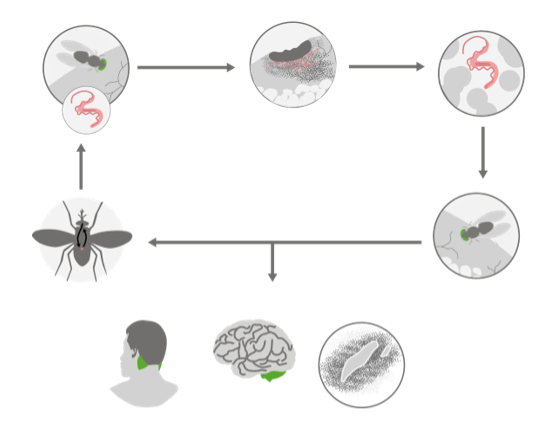
Image illustrating the pathogenesis of African trypanosomiasis
Image by Lecturio. License: CC BY-NC-SA 4.0African trypanosomiasis has 2 stages: the hemolymphatic stage and the neurologic stage
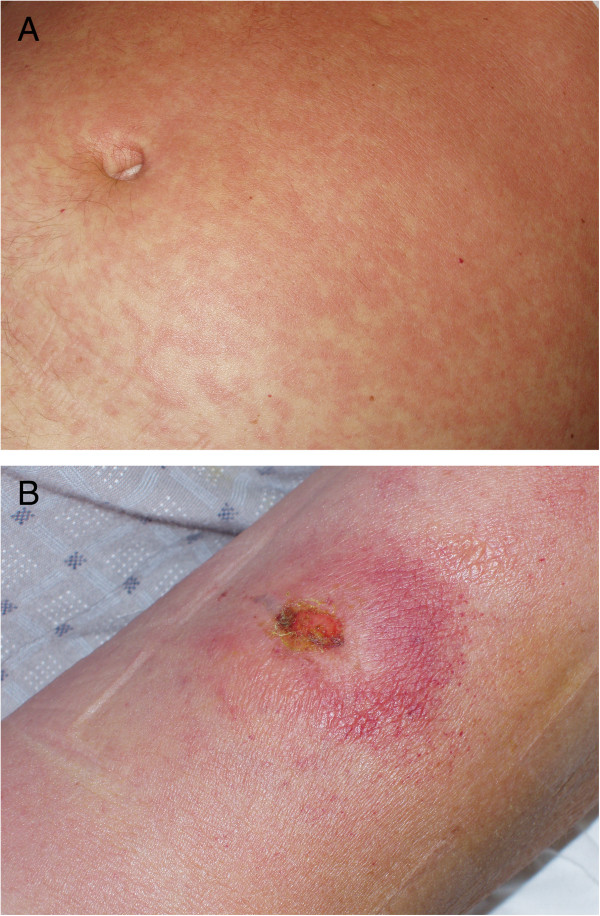
Cutaneous manifestations of African trypanosomiasis:
A: a fine, pink rash on the abdomen
B: trypanosomal chancre on the patient’s left arm that occurs at the site of inoculation
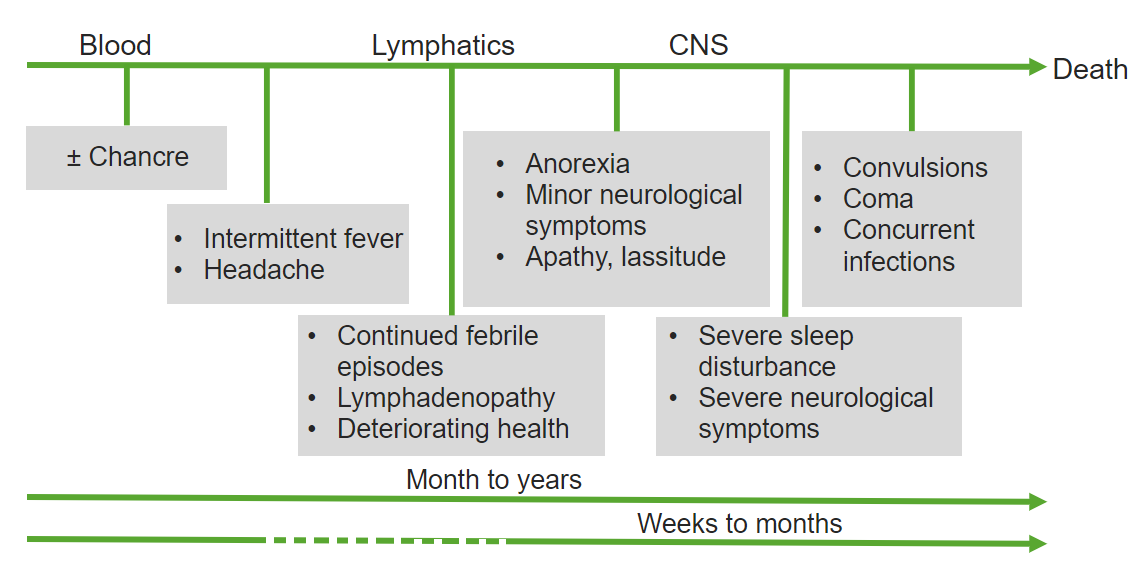
Image showing the time course of African trypanosomiasis from initial infection to chronic illness months to years later (depending on the subspecies involved)
Image by Lecturio. License: CC BY-NC-SA 4.0| Protozoa Protozoa Nitroimidazoles | Giardia Giardia A genus of flagellate intestinal eukaryotes parasitic in various vertebrates, including humans. Characteristics include the presence of four pairs of flagella arising from a complicated system of axonemes and cysts that are ellipsoidal to ovoidal in shape. Nitroimidazoles | Leishmania Leishmania Leishmania species are obligate intracellular parasites that are transmitted by an infected sandfly. The disease is endemic to Asia, the Middle East, Africa, the Mediterranean, and South and Central America. Clinical presentation varies, dependent on the pathogenicity of the species and the host’s immune response. Leishmania/Leishmaniasis | Trypanosoma | Trichomonas Trichomonas A genus of parasitic flagellate eukaryotes distinguished by the presence of four anterior flagella, an undulating membrane, and a trailing flagellum. Nitroimidazoles |
|---|---|---|---|---|
| Characteristics |
|
|
|
|
| Forms |
|
|
|
|
| Transmission |
|
|
|
|
| Clinical |
|
|
|
|
| Diagnosis |
|
|
|
|
| Treatment |
|
Depends on the clinical syndrome:
|
Depends on the clinical disease:
|
|
| Prevention |
|
|
|
|
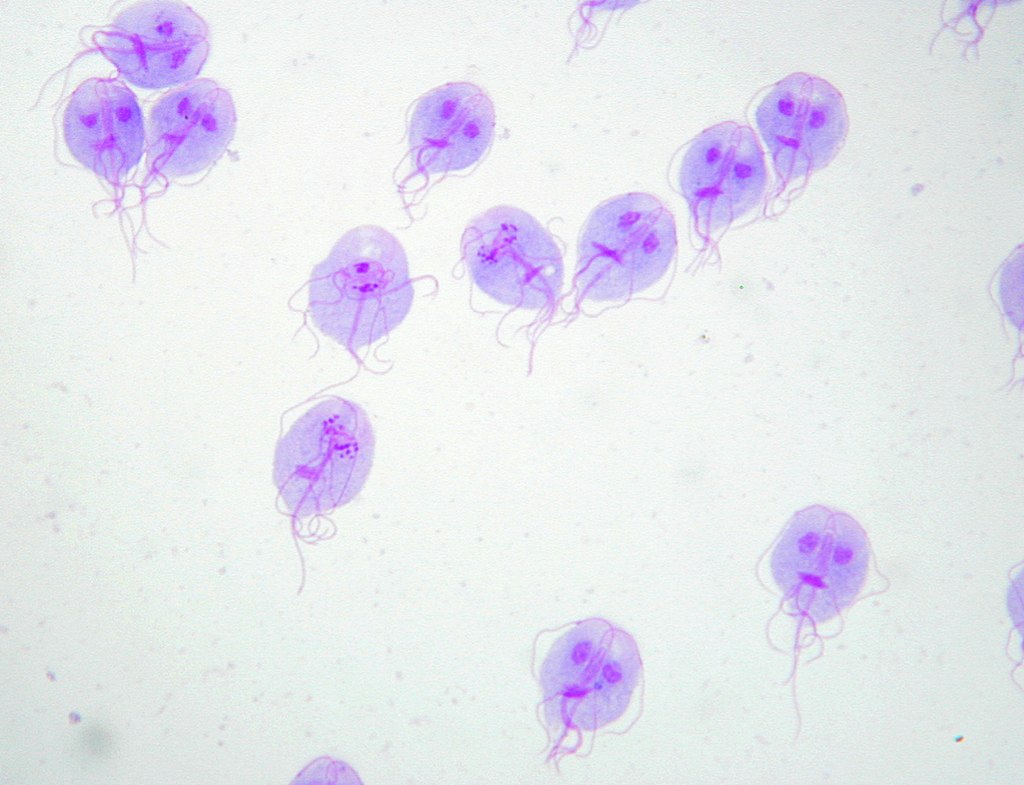
Giemsa staining of Giardia lamblia trophozoites
Image: “Trophozoites of Giardia lamblia” by Eva Nohýnková, Department of Tropical Medicine, 1st Faculty of Medicine, Charles University in Prague and Hospital Bulovka, Czech Republic. License: CC BY 4.0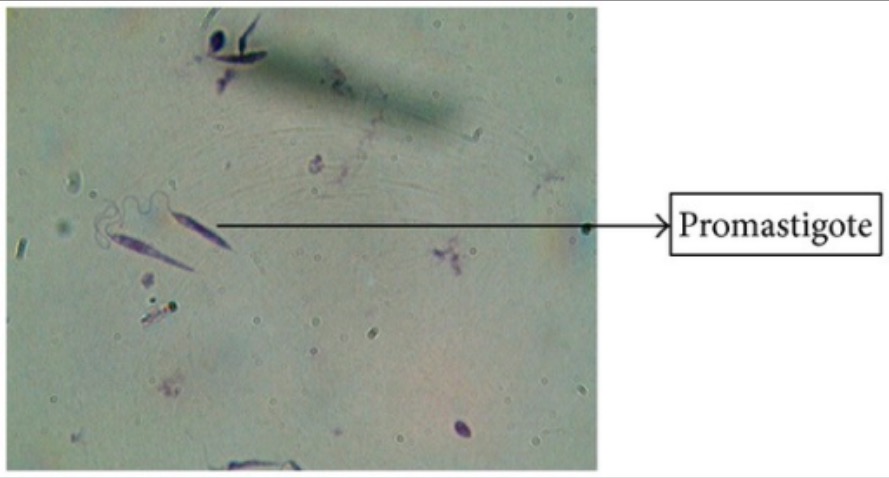
Giemsa staining of Leishmania promastigotes
Image: “Giemsa stain” by Arriyadh Community College, King Saud University, P.O. Box 28095, Riyadh 11437, Saudi Arabia. License: CC BY 3.0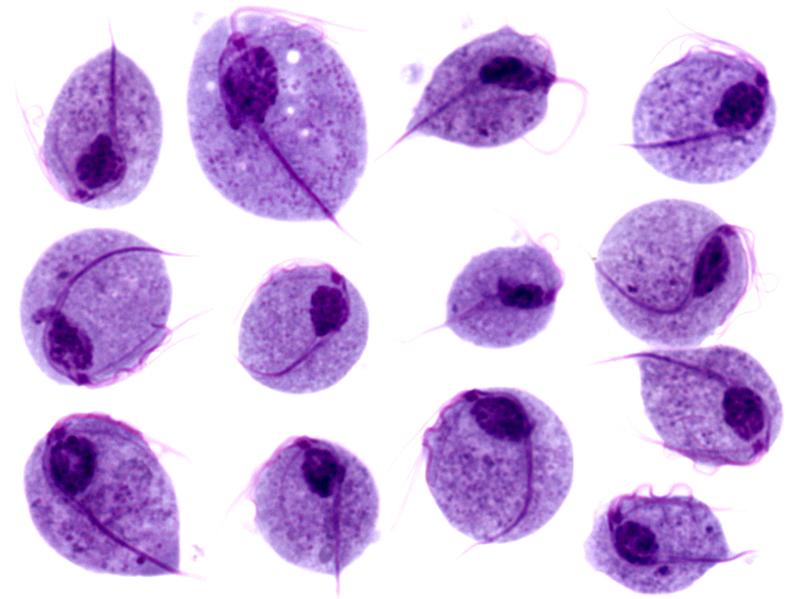
Microscopy images of Trichomonas vaginalis trophozoites
Image: “Trichomonas protozoa” by isis325. License: CC BY 2.0.