Malaria Malaria Malaria is an infectious parasitic disease affecting humans and other animals. Most commonly transmitted via the bite of a female Anopheles mosquito infected with microorganisms of the Plasmodium genus. Patients present with fever, chills, myalgia, headache, and diaphoresis. Plasmodium/Malaria, a vector-borne parasitic disease caused by Plasmodium spp., is transmitted via injection of sporozoites or immature forms of the parasite into a person's bloodstream. Sporozoites then infect the hepatocytes Hepatocytes The main structural component of the liver. They are specialized epithelial cells that are organized into interconnected plates called lobules. Liver: Anatomy and differentiate into schizonts Schizonts Multinucleate cells or a stage in the development of sporozoan protozoa. It is exemplified by the life cycle of Plasmodium falciparum in the malaria infection cycle. Plasmodium/Malaria, which subsequently rupture, and merozoites Merozoites Uninuclear cells or a stage in the life cycle of sporozoan protozoa. Merozoites, released from ruptured multinucleate schizonts, enter the bloodstream and infect the erythrocytes. Plasmodium/Malaria invade red blood cells Red blood cells Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology. As such, pharmacotherapy for malaria Malaria Malaria is an infectious parasitic disease affecting humans and other animals. Most commonly transmitted via the bite of a female Anopheles mosquito infected with microorganisms of the Plasmodium genus. Patients present with fever, chills, myalgia, headache, and diaphoresis. Plasmodium/Malaria targets exoerythrocytic and erythrocytic forms of schizonts Schizonts Multinucleate cells or a stage in the development of sporozoan protozoa. It is exemplified by the life cycle of Plasmodium falciparum in the malaria infection cycle. Plasmodium/Malaria. Collectively, these agents are classified as schizonticides.
Last updated: Mar 28, 2025
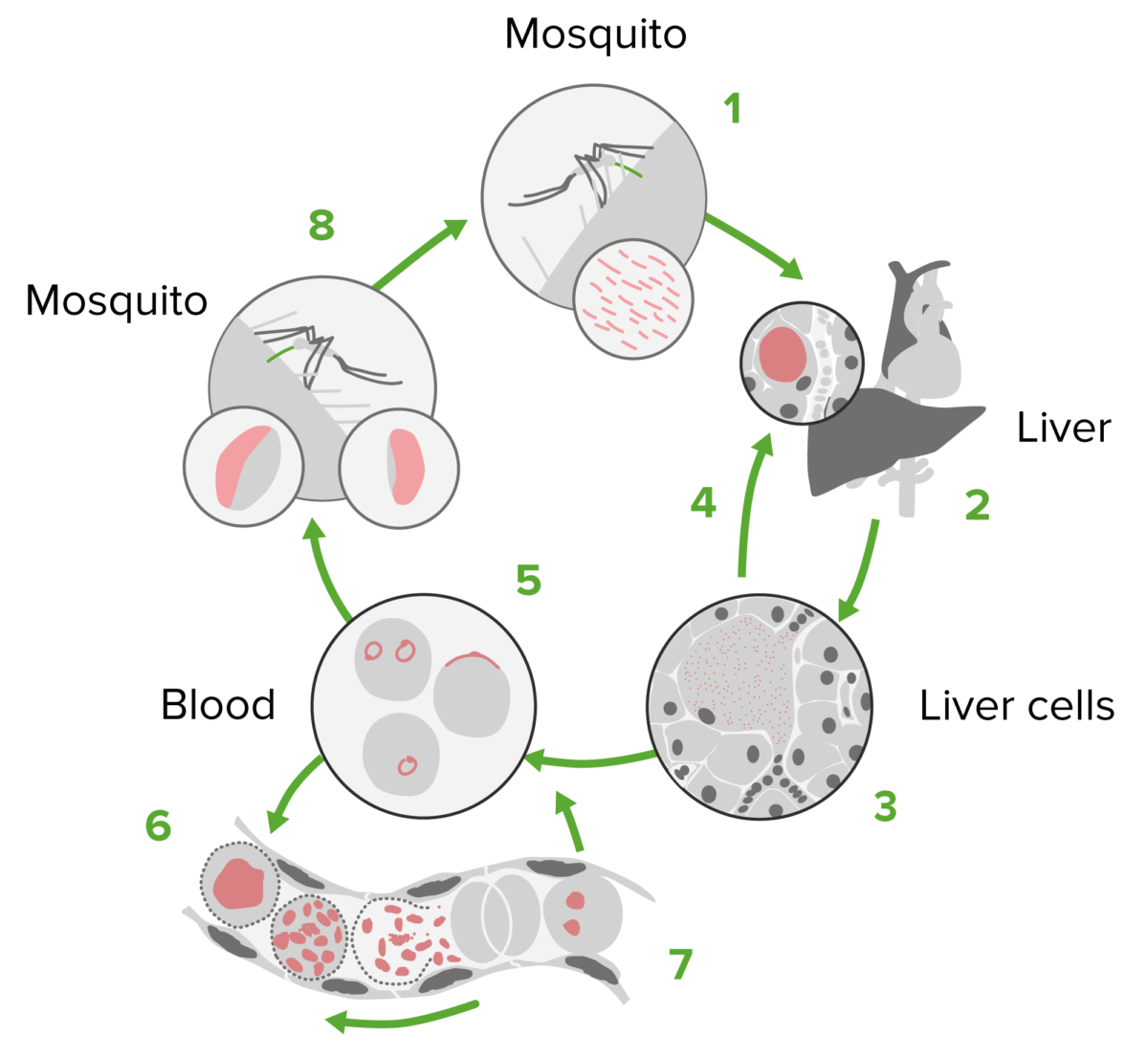
Plasmodium life cycle
Image by Lecturio.The treatment of malaria Malaria Malaria is an infectious parasitic disease affecting humans and other animals. Most commonly transmitted via the bite of a female Anopheles mosquito infected with microorganisms of the Plasmodium genus. Patients present with fever, chills, myalgia, headache, and diaphoresis. Plasmodium/Malaria is targeted at different stages of the Plasmodium life cycle:
Treatment consists of 3 steps:
Malaria Malaria Malaria is an infectious parasitic disease affecting humans and other animals. Most commonly transmitted via the bite of a female Anopheles mosquito infected with microorganisms of the Plasmodium genus. Patients present with fever, chills, myalgia, headache, and diaphoresis. Plasmodium/Malaria prophylaxis Prophylaxis Cephalosporins and prevention
Gametocidal + schizonticidal:
| Drug | Adverse effects |
|---|---|
| Artemether-lumefantrine (Coartem®) | Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, dizziness Dizziness An imprecise term which may refer to a sense of spatial disorientation, motion of the environment, or lightheadedness. Lateral Medullary Syndrome (Wallenberg Syndrome), anorexia Anorexia The lack or loss of appetite accompanied by an aversion to food and the inability to eat. It is the defining characteristic of the disorder anorexia nervosa. Anorexia Nervosa, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics/ vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, weakness, arthralgia Arthralgia Pain in the joint. Rheumatic Fever, myalgia Myalgia Painful sensation in the muscles. Ion Channel Myopathy |
| Artesunate | Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, dizziness Dizziness An imprecise term which may refer to a sense of spatial disorientation, motion of the environment, or lightheadedness. Lateral Medullary Syndrome (Wallenberg Syndrome), anorexia Anorexia The lack or loss of appetite accompanied by an aversion to food and the inability to eat. It is the defining characteristic of the disorder anorexia nervosa. Anorexia Nervosa, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics/ vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia |
| Atovaquone-proguanil (Malarone®) | Abdominal pain Abdominal Pain Acute Abdomen, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics/ vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, cough in children |
| Chloroquine |
|
| Hydroxychloroquine Hydroxychloroquine A chemotherapeutic agent that acts against erythrocytic forms of malarial parasites. Hydroxychloroquine appears to concentrate in food vacuoles of affected protozoa. It inhibits plasmodial heme polymerase. Immunosuppressants | GI upset, headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, rash Rash Rocky Mountain Spotted Fever, visual changes |
| Doxycycline | Photosensitivity Photosensitivity Tetracyclines, GI upset (mitigated by taking with food), permanent tooth discoloration in children < 8 years |
| Mefloquine |
|
| Primaquine | GI upset, headaches, methemoglobinemia Methemoglobinemia Methemoglobinemia is a condition characterized by elevated levels of methemoglobin in the blood. Methemoglobin is the oxidized form of hemoglobin, where the heme iron has been converted from the usual ferrous (Fe2+) to the ferric (Fe3+) form. The Fe3+ form of iron cannot bind O2, and, thus, leads to tissue hypoxia. Methemoglobinemia, hemolysis (due to G6PD G6PD Pentose Phosphate Pathway deficiency) |
| Quinidine Quinidine An optical isomer of quinine, extracted from the bark of the cinchona tree and similar plant species. This alkaloid dampens the excitability of cardiac and skeletal muscles by blocking sodium and potassium currents across cellular membranes. It prolongs cellular action potentials, and decreases automaticity. Quinidine also blocks muscarinic and alpha-adrenergic neurotransmission. Class 1 Antiarrhythmic Drugs (Sodium Channel Blockers) |
|
| Tafenoquine |
|
| Drug | Classification | Mechanism of action | Usage | Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation |
|---|---|---|---|---|
| Artemether-lumefantrine (Coartem®) |
|
Metabolized in plasmodial food vacuole to toxic free radicals Free radicals Highly reactive molecules with an unsatisfied electron valence pair. Free radicals are produced in both normal and pathological processes. They are proven or suspected agents of tissue damage in a wide variety of circumstances including radiation, damage from environment chemicals, and aging. Natural and pharmacological prevention of free radical damage is being actively investigated. Ischemic Cell Damage |
|
|
| Artesunate |
|
Metabolized in plasmodial food vacuole to toxic free radicals Free radicals Highly reactive molecules with an unsatisfied electron valence pair. Free radicals are produced in both normal and pathological processes. They are proven or suspected agents of tissue damage in a wide variety of circumstances including radiation, damage from environment chemicals, and aging. Natural and pharmacological prevention of free radical damage is being actively investigated. Ischemic Cell Damage |
|
Known hypersensitivity to artemisinins |
| Atovaquone-proguanil (Malarone®) |
|
|
|
Severe renal impairment (CrCl < 30 mL/minute) |
| Chloroquine |
|
Enters the food vacuoles of Plasmodia and disrupts heme polymerization | Prophylaxis Prophylaxis Cephalosporins in areas with chloroquine-sensitive malaria Malaria Malaria is an infectious parasitic disease affecting humans and other animals. Most commonly transmitted via the bite of a female Anopheles mosquito infected with microorganisms of the Plasmodium genus. Patients present with fever, chills, myalgia, headache, and diaphoresis. Plasmodium/Malaria |
|
| Hydroxychloroquine Hydroxychloroquine A chemotherapeutic agent that acts against erythrocytic forms of malarial parasites. Hydroxychloroquine appears to concentrate in food vacuoles of affected protozoa. It inhibits plasmodial heme polymerase. Immunosuppressants | Blood schizonticide | Known hypersensitivity to 4-aminoquinolone derivatives | ||
| Doxycycline |
|
Inhibits protein synthesis Synthesis Polymerase Chain Reaction (PCR) in the plasmodial apicoplast |
|
|
| Mefloquine |
|
Enters the food vacuoles of Plasmodia and disrupts heme polymerization | Prophylaxis Prophylaxis Cephalosporins in areas with chloroquine-sensitive malaria Malaria Malaria is an infectious parasitic disease affecting humans and other animals. Most commonly transmitted via the bite of a female Anopheles mosquito infected with microorganisms of the Plasmodium genus. Patients present with fever, chills, myalgia, headache, and diaphoresis. Plasmodium/Malaria or chloroquine-resistant areas |
|
| Primaquine |
|
|
Prophylaxis
Prophylaxis
Cephalosporins in
P. vivax
P. vivax
A protozoan parasite that causes vivax malaria. This species is found almost everywhere malaria is endemic and is the only one that has a range extending into the temperate regions.
Plasmodium/Malaria predominant areas
|
|
| Quinidine Quinidine An optical isomer of quinine, extracted from the bark of the cinchona tree and similar plant species. This alkaloid dampens the excitability of cardiac and skeletal muscles by blocking sodium and potassium currents across cellular membranes. It prolongs cellular action potentials, and decreases automaticity. Quinidine also blocks muscarinic and alpha-adrenergic neurotransmission. Class 1 Antiarrhythmic Drugs (Sodium Channel Blockers) IV |
|
|
Discontinued in the United States | |
| Quinine |
|
|
|
|
| Tafenoquine |
|
Interferes with heme polymerization |
Prophylaxis
Prophylaxis
Cephalosporins in all areas
|
|