Human cells are primarily reliant on aerobic metabolism. Therefore, it is of vital importance to efficiently obtain oxygen from the environment and bring it to the tissues, while excreting the by-product of cellular respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal) (carbon dioxide). Respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal) involves both the respiratory and circulatory systems. There are 4 processes that supply the body with O2 and dispose of CO2. The respiratory system is involved in pulmonary ventilation and external respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal), while the circulatory system is responsible for transport and internal respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal). Pulmonary ventilation (breathing) represents movement of air into and out of the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy. External respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal) is represented by the O2 and CO2 exchange between the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy and the blood.
Last updated: Dec 5, 2022
Ventilation, or breathing, involves the action and movements of structures found in the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess and thoracic cavity belonging to the pulmonary, musculoskeletal, and cardiac systems.
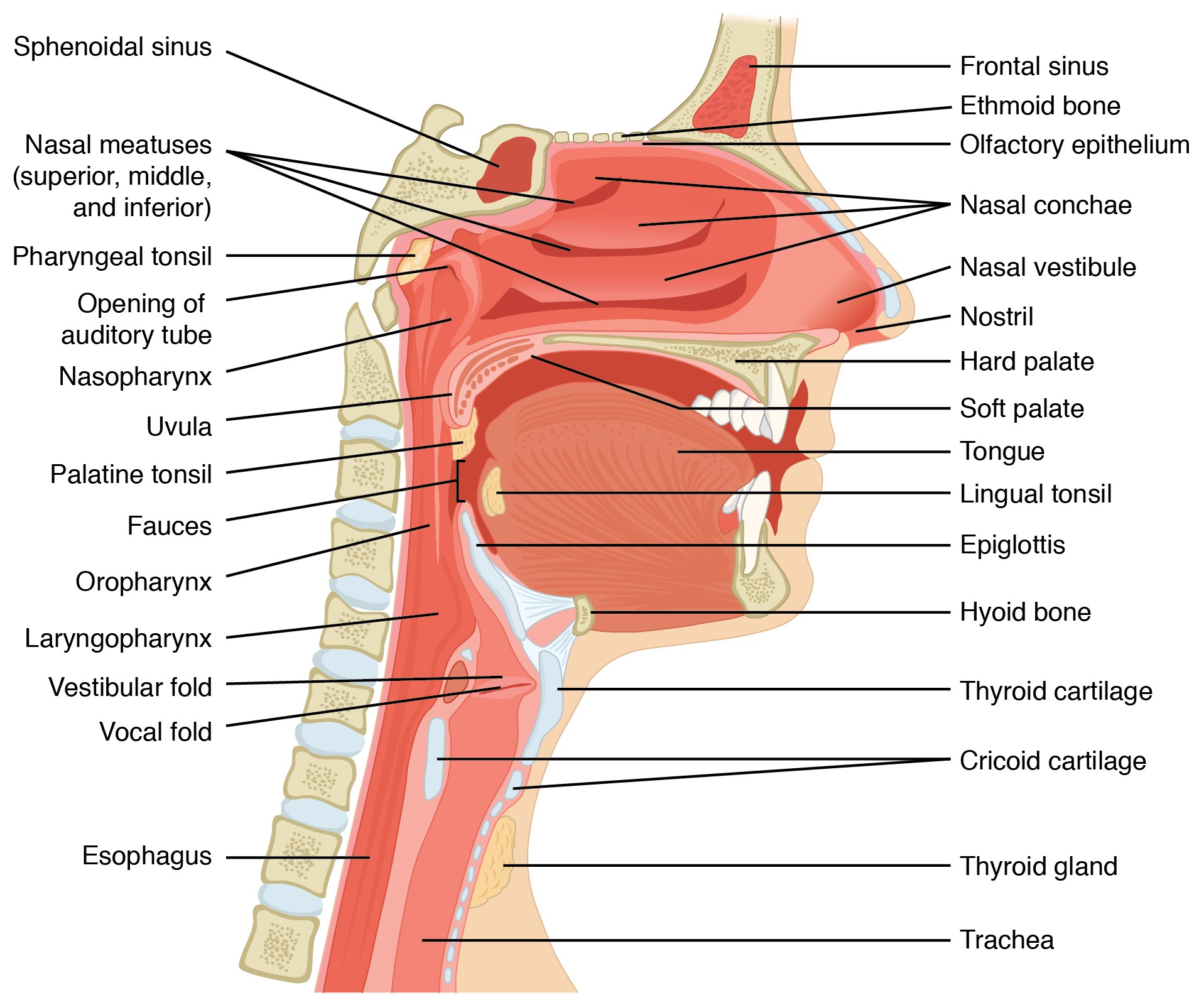
The anatomy of the upper respiratory tract and adjacent structures
Image: “2303 Anatomy of Nose-Pharynx-Mouth-Larynx” by OpenStax College. License: CC BY 3.0, edited by Lecturio.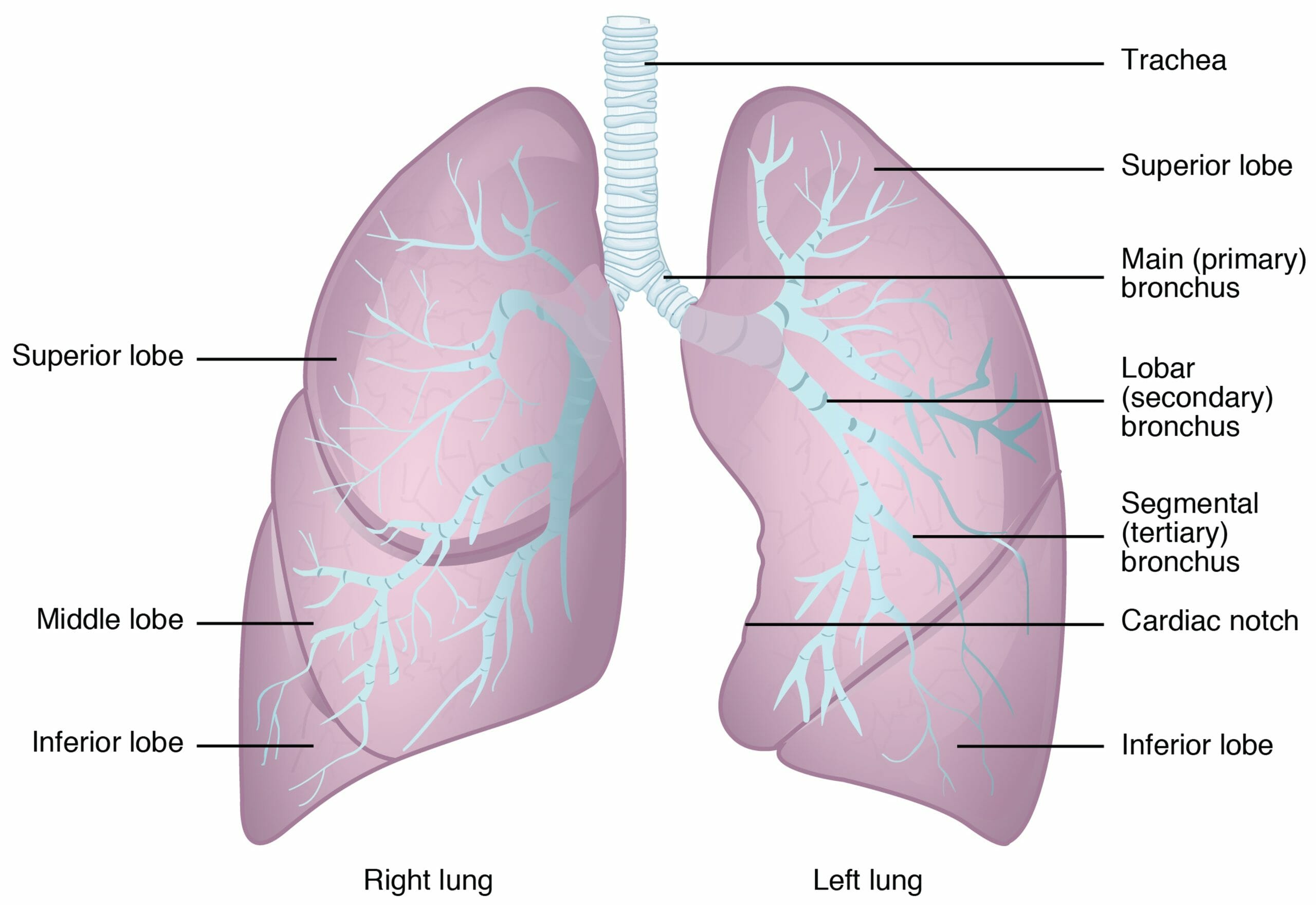
The anatomy of the lower respiratory tract
Image by Lecturio.Breathing consists of 2 phases:
Inspiration and expiration:
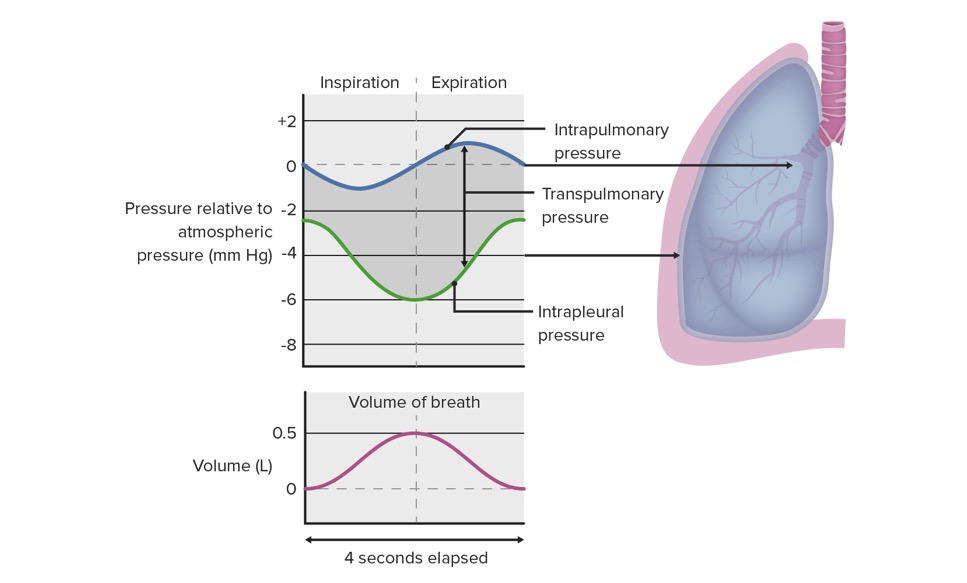
Changes in pressure relationships in the thoracic cavity during respiration:
During inspiration, muscles move to create negative intrapleural pressure (green line). This negative pressure is transferred to the lungs, making intrapulmonary pressure more negative (blue line) in relation to atmospheric pressure. Air flows into the lungs down this pressure gradient, increasing the breath volume (purple line). With exhalation, the process reverses, leading to airflow out of the lungs.
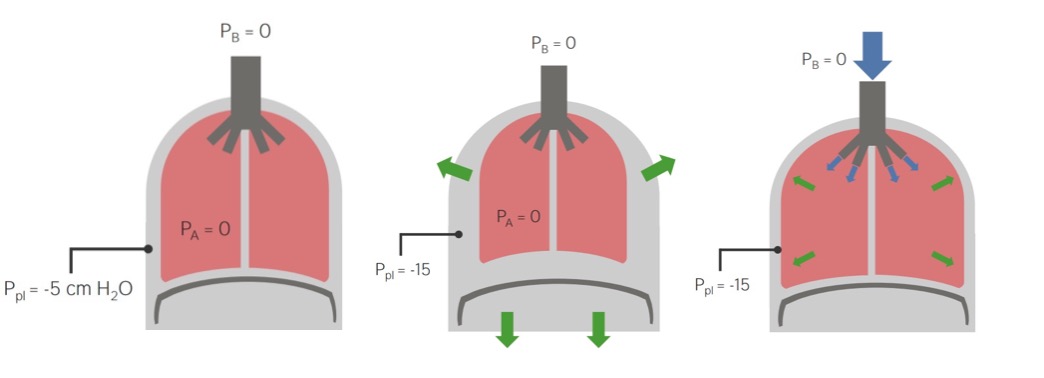
Diagram showing the mechanics of breathing
PA: Alveolar pressure
PB: Barometric pressure
Ppl: Pleural pressure
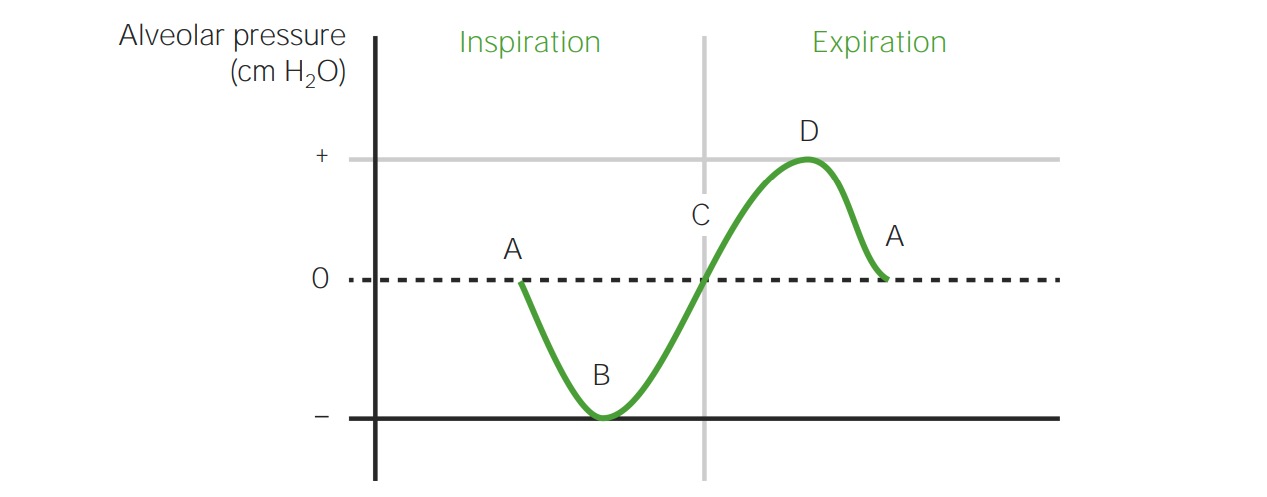
Chart showing alveolar pressure throughout the respiratory cycle:
Note the need for negative pressure during inspiration for air to be drawn in.
Inspiration is an active process:
Expiration (at rest) is a passive process:
Lung volumes are specific volumes of air contained by different portions of lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy at specific points in the respiratory cycle.
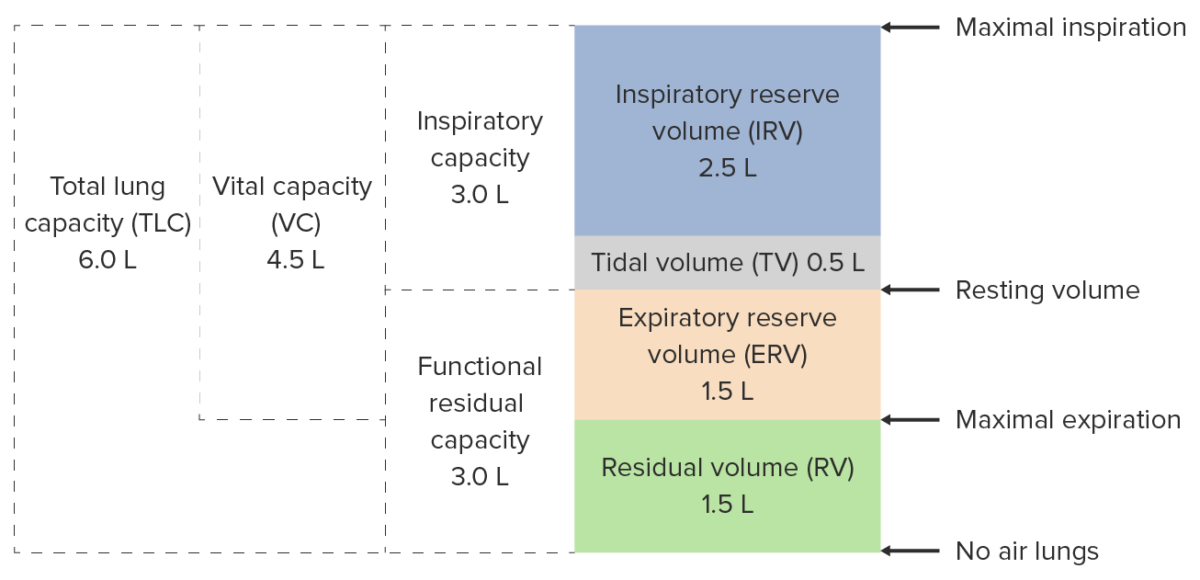
Lung volumes and capacities
Image by Lecturio. License: CC BY-NC-SA 4.0Lung capacities are a combination of 2 or more volumes.
Dead space is air that enters and exits lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy but does not make it to areas where gas exchange Gas exchange Human cells are primarily reliant on aerobic metabolism. The respiratory system is involved in pulmonary ventilation and external respiration, while the circulatory system is responsible for transport and internal respiration. Pulmonary ventilation (breathing) represents movement of air into and out of the lungs. External respiration, or gas exchange, is represented by the O2 and CO2 exchange between the lungs and the blood. Gas Exchange can occur.
Ventilation is the process of moving air in and out.
The work of breathing Work of breathing Respiratory muscle contraction during inhalation. The work is accomplished in three phases: lung compliance work, that required to expand the lungs against its elastic forces; tissue resistance work, that required to overcome the viscosity of the lung and chest wall structures; and airway resistance work, that required to overcome airway resistance during the movement of air into the lungs. Work of breathing does not refer to expiration, which is entirely a passive process caused by elastic recoil of the lung and chest cage. Pulmonary Examination is the amount of energy a person needs to breathe.
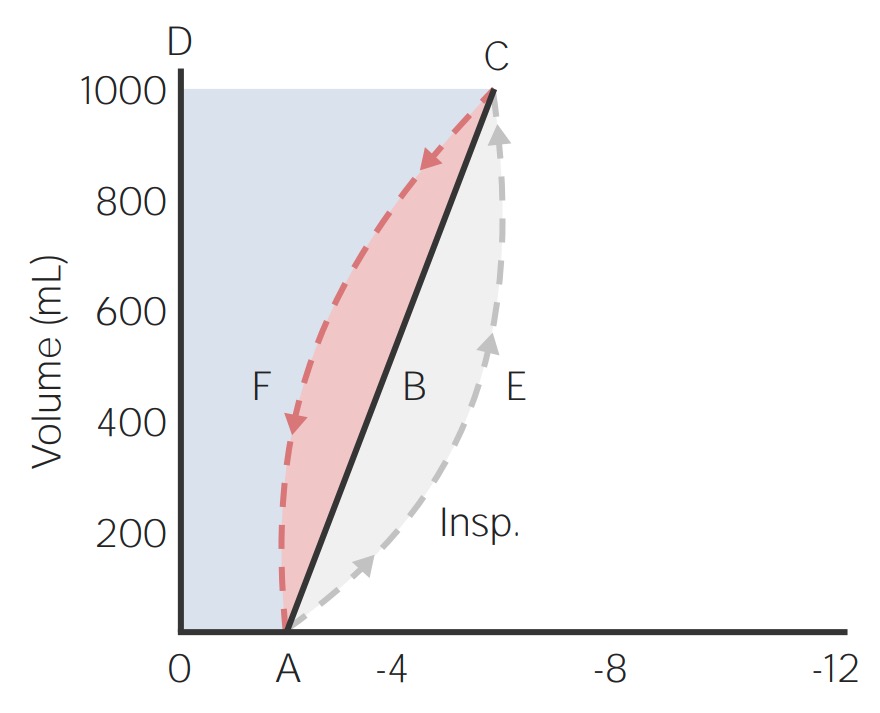
Work of breathing in a healthy lung:
Pressure can be seen on the x-axis and volume in liters on the y-axis. The order in inhalation is AECBA. The order in exhalation is ABCFA.
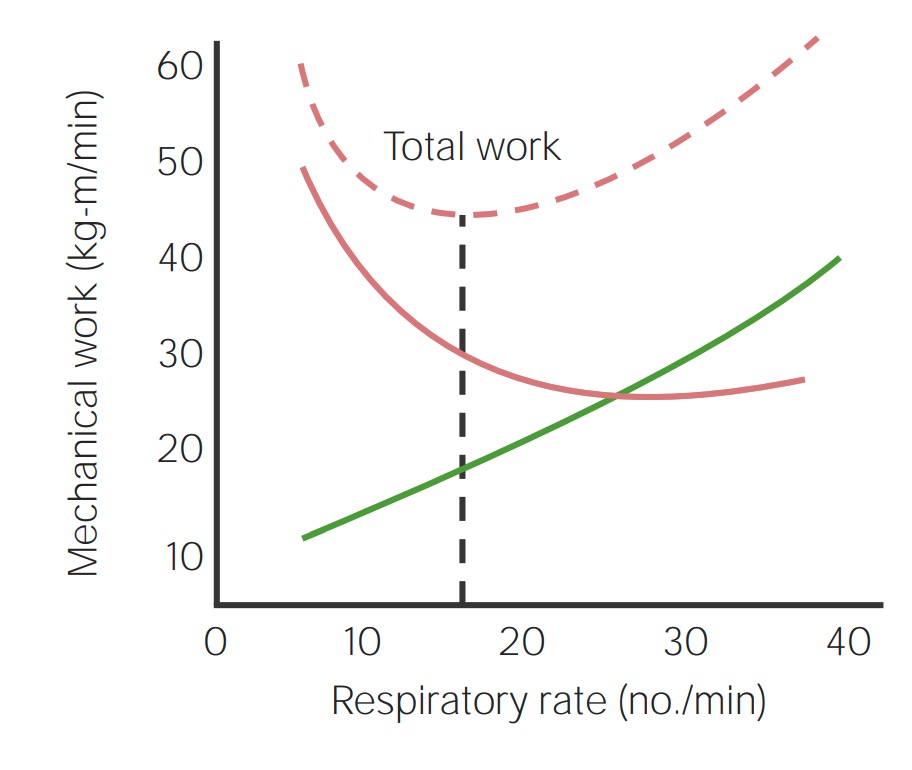
Total work of breathing is a composite of elastic and nonelastic work within the lungs:
Respiratory rate is seen on the x-axis and mechanical work is seen on the y-axis. The respiratory rate of an individual will correspond to the least amount of work needed to breathe. The dashed line shows the relationship between the lowest amount of total work and its corresponding respiratory rate in most individuals (< 25 breaths per minute). A person with a restrictive pulmonary disease would have the line shifted to the right.

Work of breathing in a normal lung (left) compared to a lung with obstructive pulmonary disease (right):
Because the flow of air is being obstructed, the person has to do great work to breathe in and even greater work to breathe out (push out) the air.

Work of breathing in a normal lung (left) compared to a lung with restrictive pulmonary disease (right):
Because its compliance is decreased, the restrictive lung requires more negative pressure to be inflated, thereby increasing the amount of work needed to breathe.
Aside from the pressures that the thoracic musculature is capable of creating, ventilation is limited by the physical properties of the structures of the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy. The most important physical properties to be taken into account are:
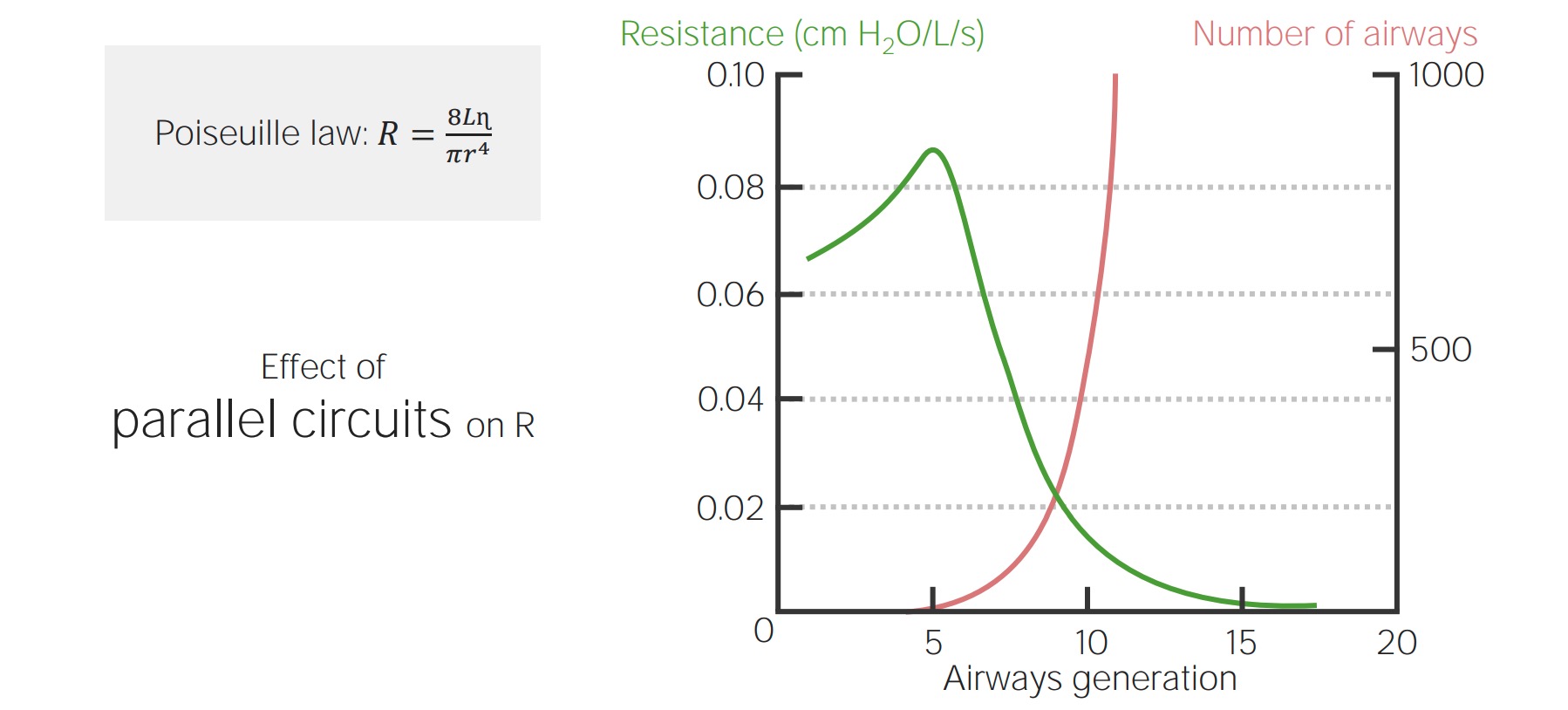
Chart describing the inverse proportion between airway resistance and the number of airways:
Resistance decreases as the number of airways increases. Poiseulle’s law describes this relationship (seen at the top left corner).
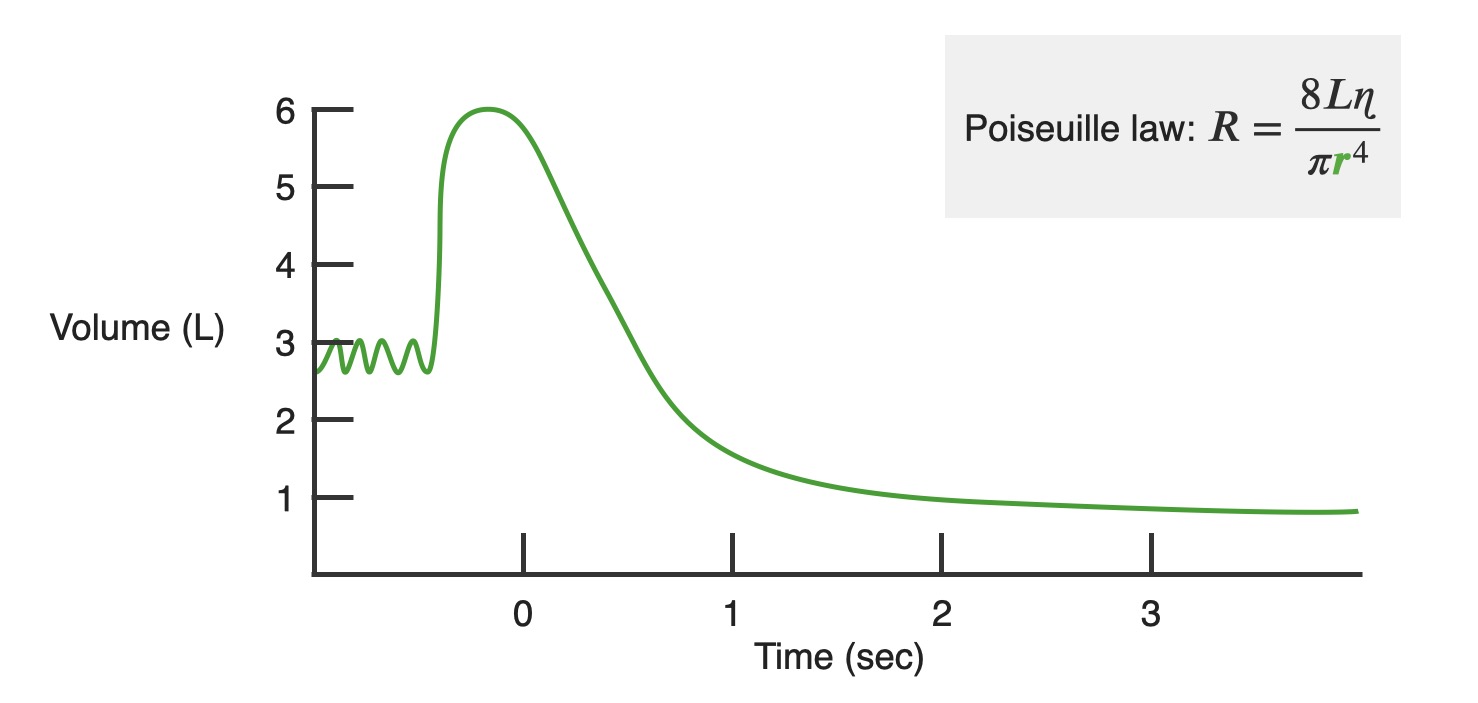
Chart showing normal changes in air volume
Image by Lecturio. License: CC BY-NC-SA 4.0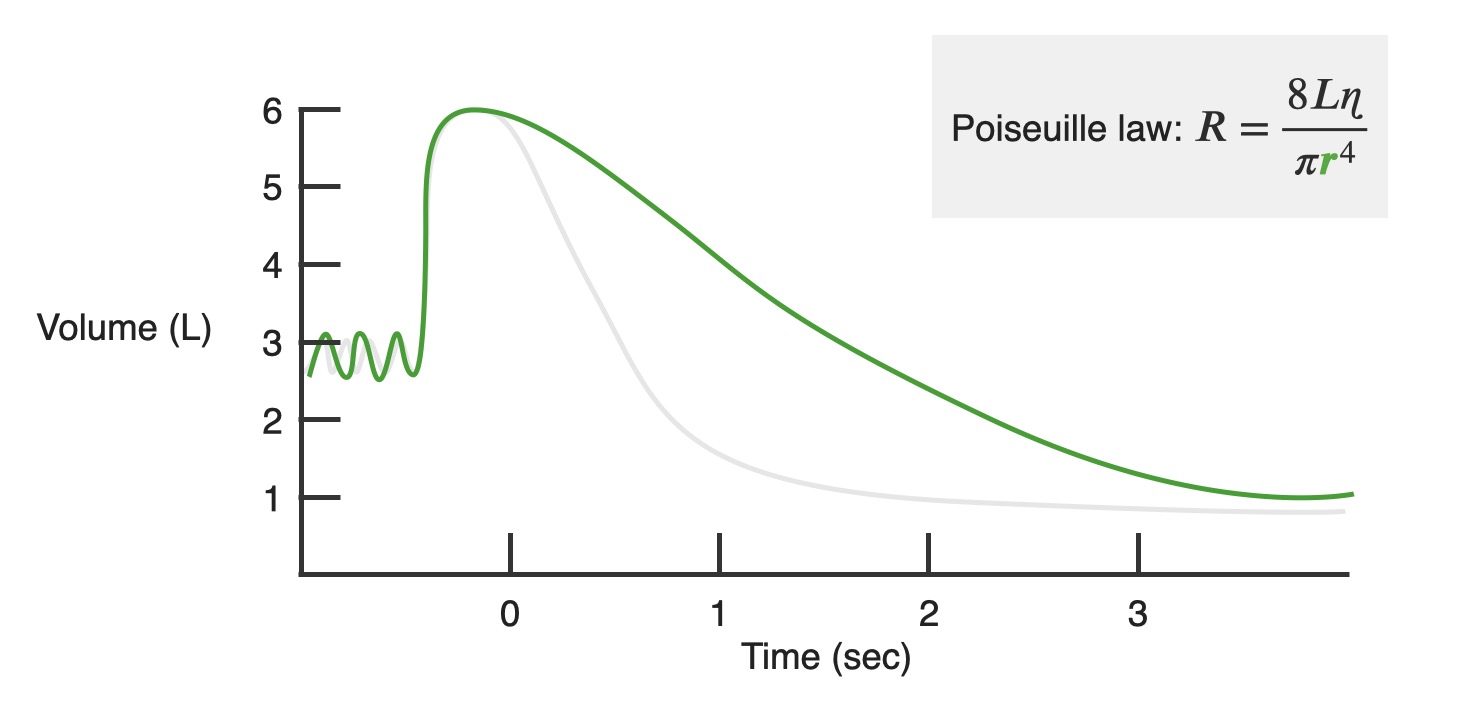
Chart showing changes in air volume demonstrated by a person with obstructive lung disease:
Note how the increase in resistance impedes properly timed outflow of air.
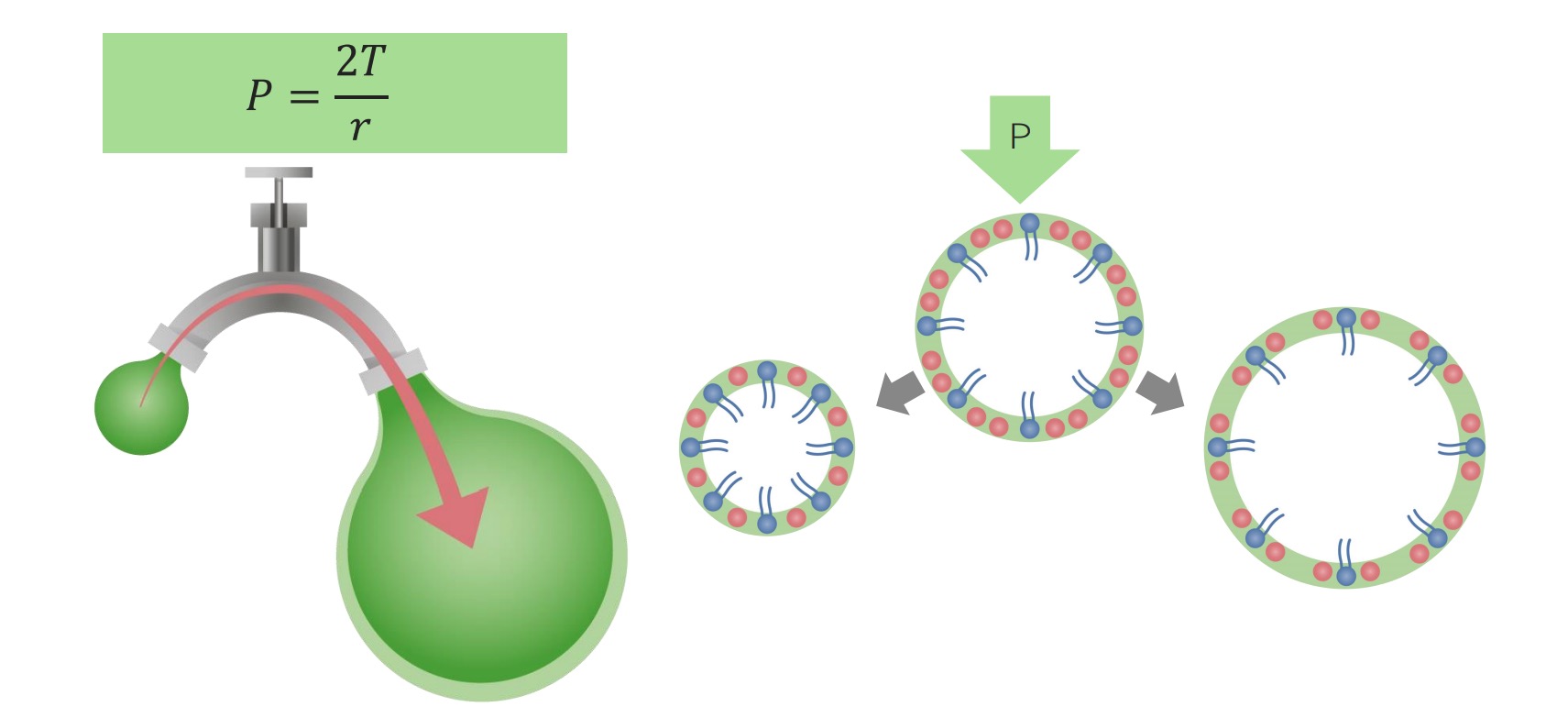
Pulmonary surfactant annuls the Law of Laplace:
Without pulmonary surfactant, a scenario like the one shown on the left will occur: Larger air sacs will fill up more easily owing to their reduced surface tension. With pulmonary surfactant, all surface tension is reduced and, therefore, all alveoli inflate to their respective capacities.

Reduction of surface tension by pulmonary surfactant:
The polar heads of the phospholipids in the pulmonary surfactant stand between the water molecules and reduce the surface tension.
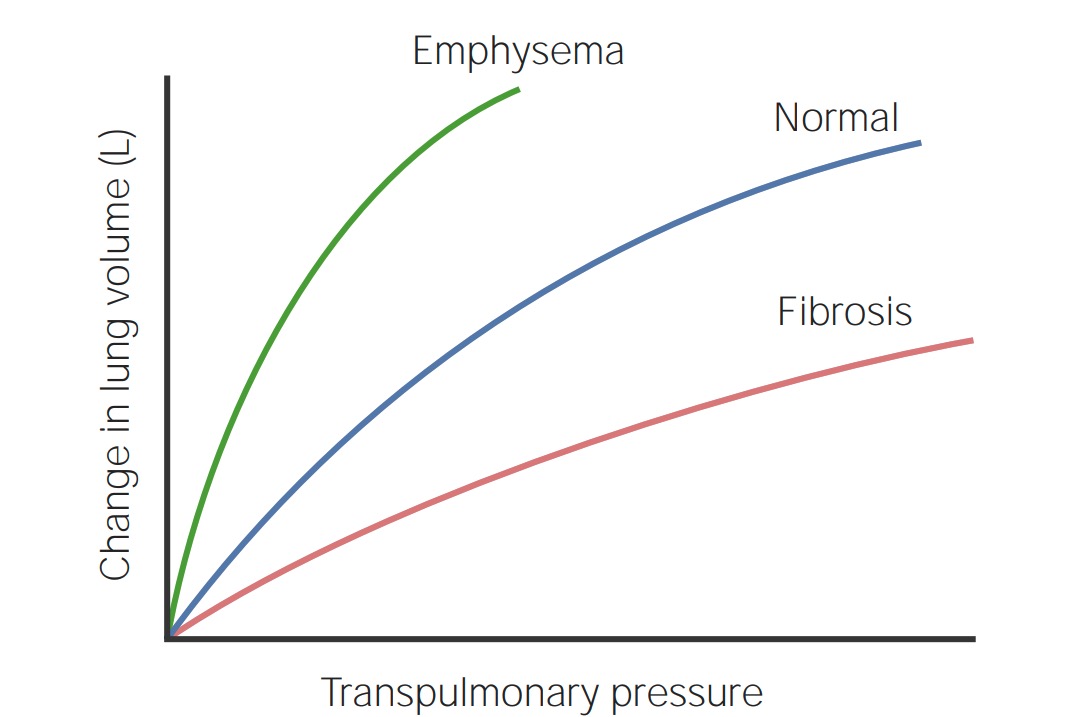
Chart of transpulmonary pressure (x-axis) and change in lung volume in liters (y-axis):
This chart compares the normal compliance of a healthy lung with the increased compliance seen in pulmonary emphysema and the reduced compliance of pulmonary fibrosis.
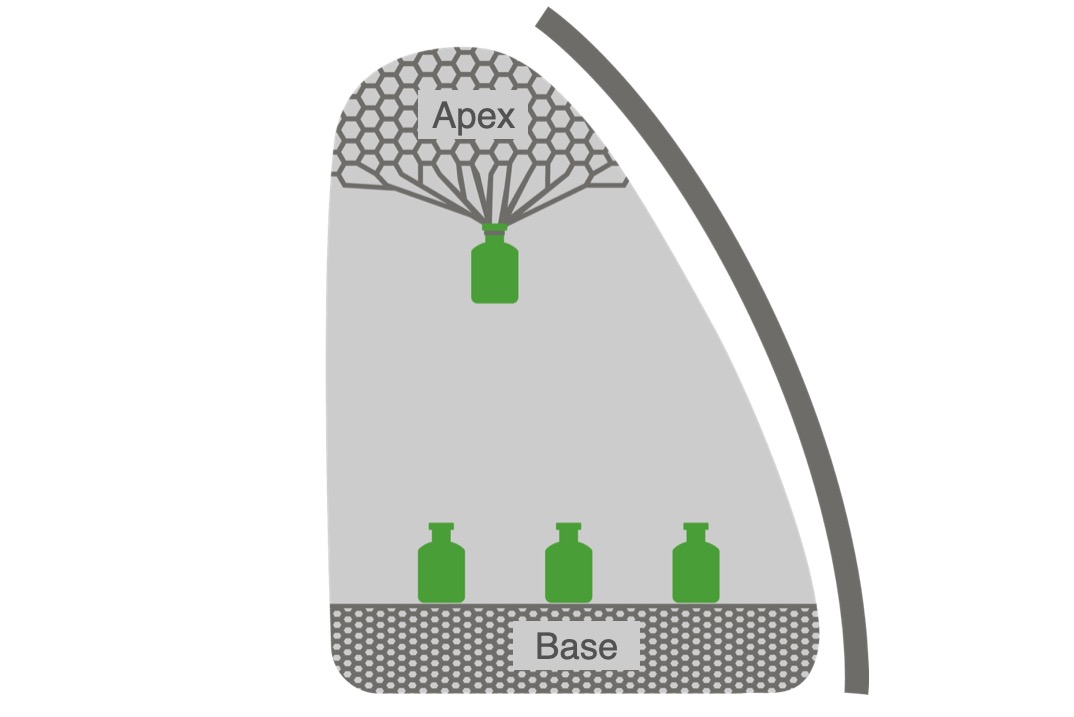
Influence of gravity on lung compliance:
The apex of the lung is less compliant owing to gravity stretching its elastic fibers, while the base is more compliant owing to the same pull of gravity and the limits of the thoracic cavity that compress its elastic fibers.