Since human cells are primarily reliant on aerobic metabolism, it is of vital importance to efficiently obtain oxygen from the environment and bring it to the tissues while excreting the byproduct of cellular respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal) (CO2). Respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal) involves both the respiratory and circulatory systems. There are 4 processes that supply the body with O2 and dispose of CO2. The respiratory system is involved in pulmonary ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing and external respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal), while the circulatory system is responsible for transport and internal respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal). Pulmonary ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing (breathing) represents movement of air into and out of the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy. External respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal), or gas exchange, is represented by the O2 and CO2 exchange between the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy and the blood.
Last updated: Dec 5, 2022
Gas exchange occurs at the level of the alveoli Alveoli Small polyhedral outpouchings along the walls of the alveolar sacs, alveolar ducts and terminal bronchioles through the walls of which gas exchange between alveolar air and pulmonary capillary blood takes place. Acute Respiratory Distress Syndrome (ARDS) in the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy and capillaries Capillaries Capillaries are the primary structures in the circulatory system that allow the exchange of gas, nutrients, and other materials between the blood and the extracellular fluid (ECF). Capillaries are the smallest of the blood vessels. Because a capillary diameter is so small, only 1 RBC may pass through at a time. Capillaries: Histology of the pulmonary circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment.
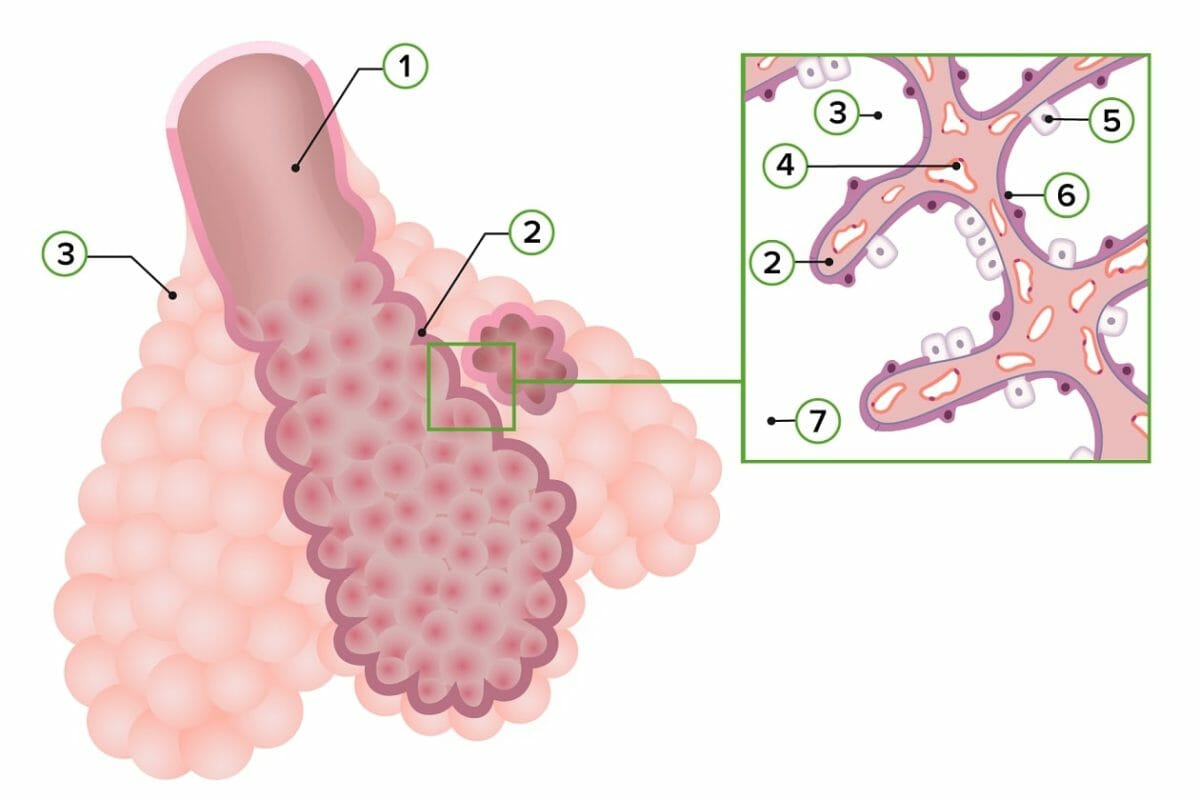
Schematic diagram of the structure of the respiratory zone of the lower respiratory tract:
Note the composition of the alveolar wall:
1) Respiratory bronchiole
2) Primary interalveolar septum
3) Alveolar sac
4) Capillaries
5) Type II pneumocyte
6) Type I pneumocyte
7) Alveolar duct
During gas exchange, O₂ and CO₂ must cross the pulmonary membrane. This process is driven by multiple complex forces determined by the physical properties of these gases.
The rate of gas exchange is determined by the efficiency of the exchange across the pulmonary membrane and the speed at which it can be brought there from the air (for O₂) or from the body (for CO₂).
O₂ and CO₂ must be transported through the bloodstream to reach sites of gas exchange.
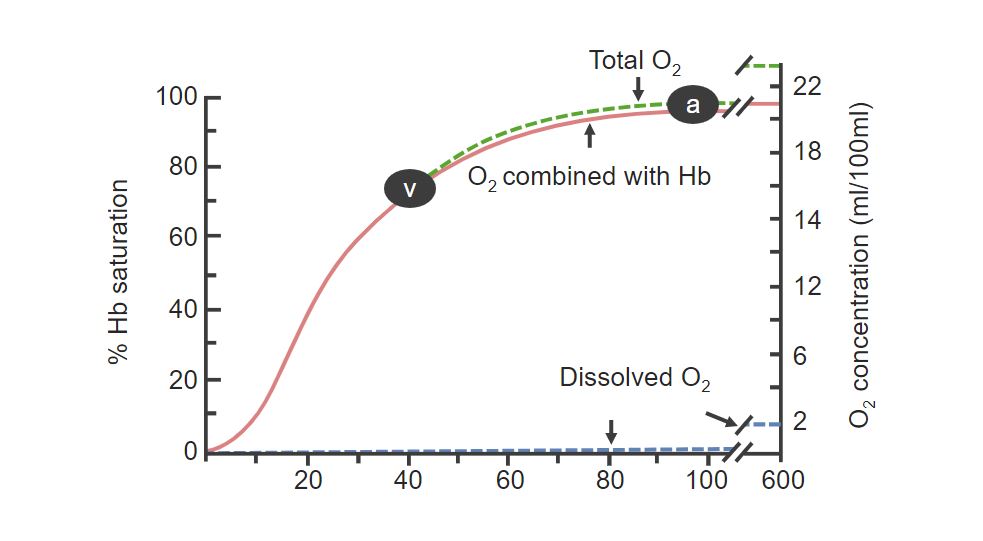
Saturation of Hemoglobin:
Percentage of bound hemoglobin increases with the concentration of O2. Notice the letter A, which signifies the saturation of hemoglobin in arterial blood (close to 99%). The letter V signifies the hemoglobin saturation of venous blood.
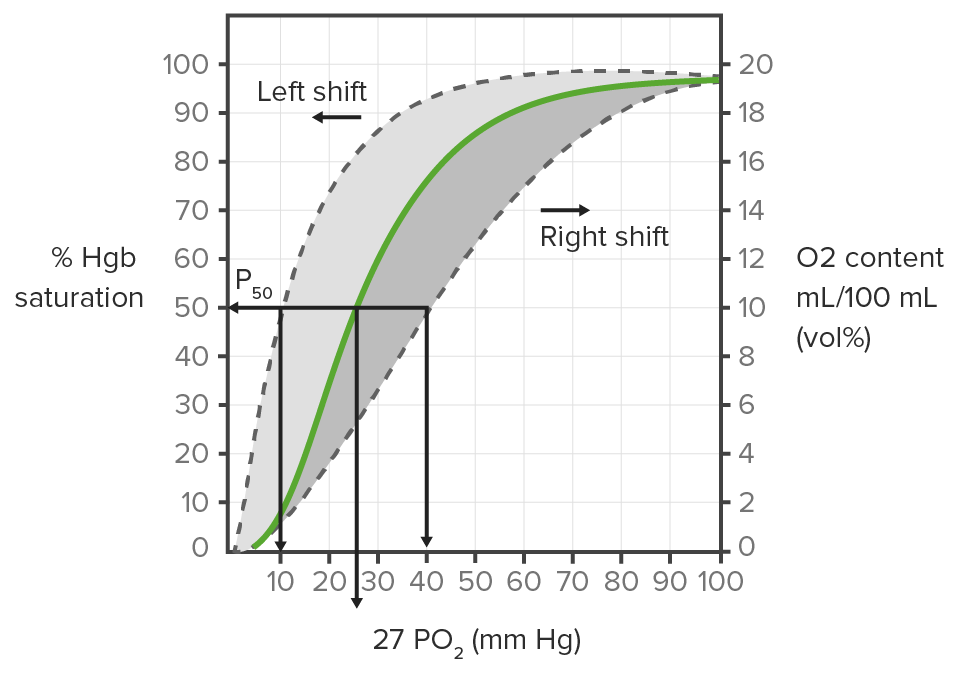
Dissociation curve of Hemoglobin:
Shows the right and left shifts that can occur when oxygen delivery to the tissues is increased or decreased, respectively.
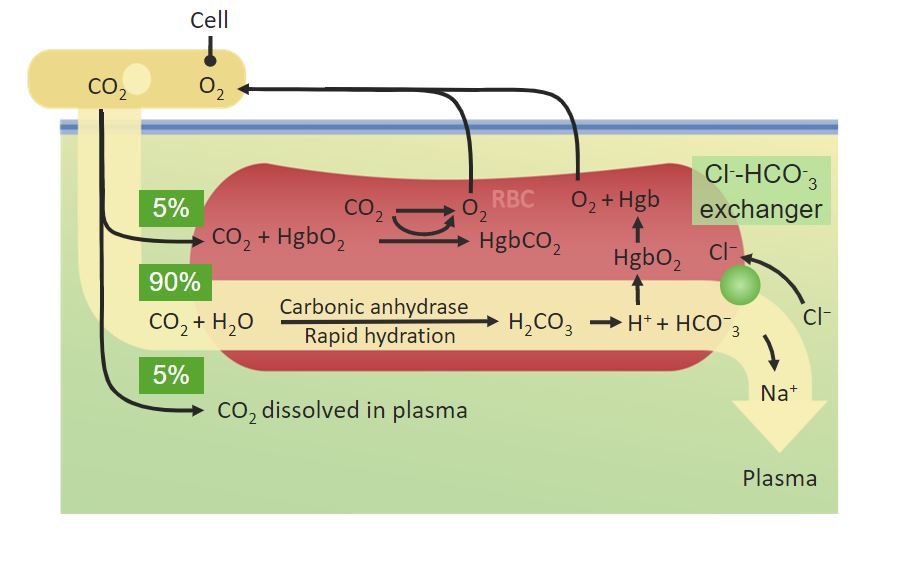
Percentages of CO2 transported in the plasma:
Notice how 90% is converted by the Carbonic anhydrase into HCO3– inside red blood cells.
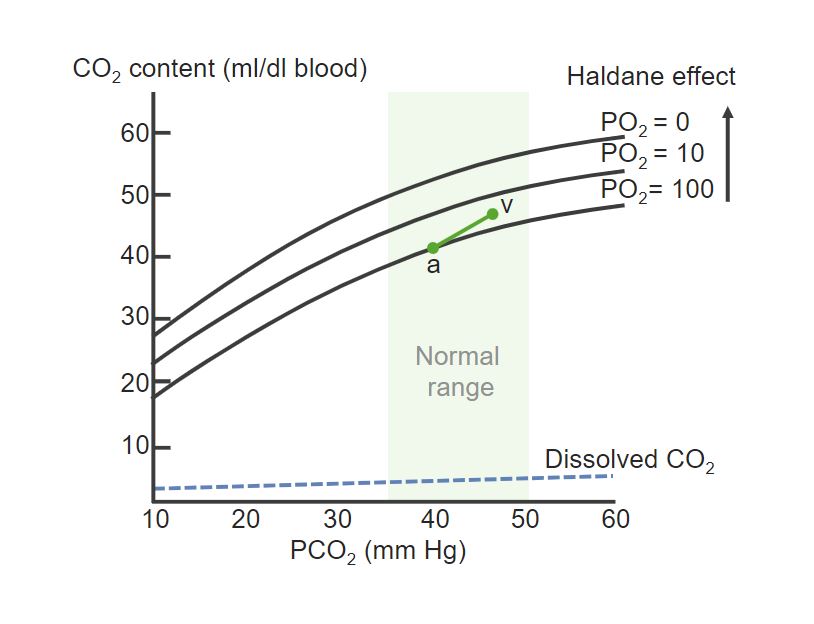
Dissociation curve of Hb and CO2:
Notice how PCO2 increases from the arterial (a) to the venous side (v). The dissociation curve is elevated with the decrease in PO2, referencing the fact that a low O2 concentration allows for more CO2 to be bound to Hb.
Ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing and perfusion are the mechanisms that transport O₂ and CO₂ between the pulmonary membrane and the body’s tissues.
Perfusion is the flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure of blood to pulmonary vasculature.
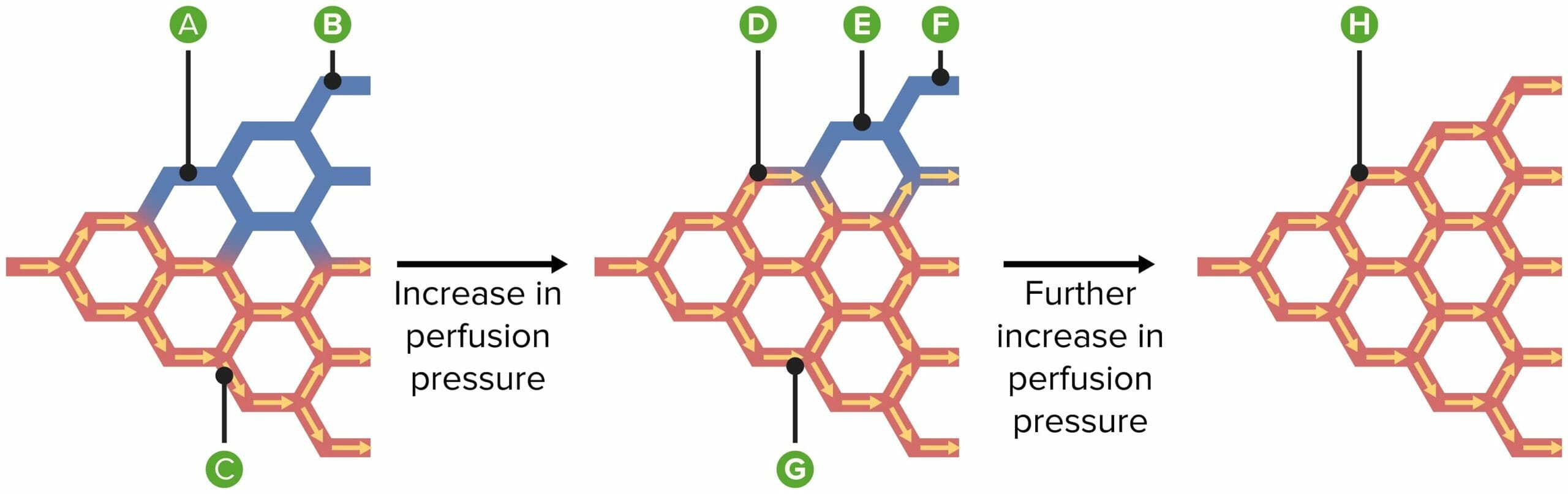
Diagram explaining the mechanisms of recruitment and distension of blood vessels when mean pulmonary arterial blood pressure is increased:
A) Some vessels are open but do not conduct blood.
B) Some vessels are collapsed.
C) Other vessels are open and conduct blood.
D) Previously open, nonconducting vessels now conduct blood.
E) In the 1st stage of recruitment, previously collapsed vessels become patent but do not conduct blood.
F) Later during recruitment, the previously collapsed vessels now conduct blood.
G) Meanwhile, distension widens previously open, blood-conducting vessels.
H) All vessels now dilate, causing resistance to fall.
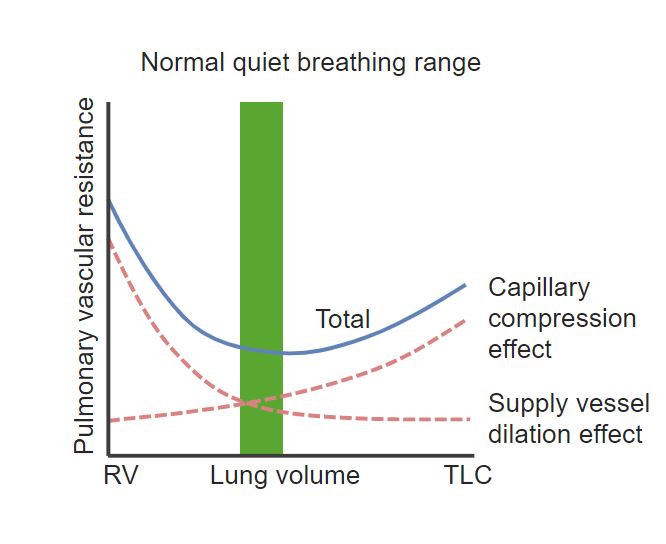
Chart showing the relationship between lung volume (x-axis) and pulmonary vascular resistance (y-axis):
At low lung volume (RV: residual volume) and at very high lung volume (Total Lung Capacity: TLC) vascular resistance increases.
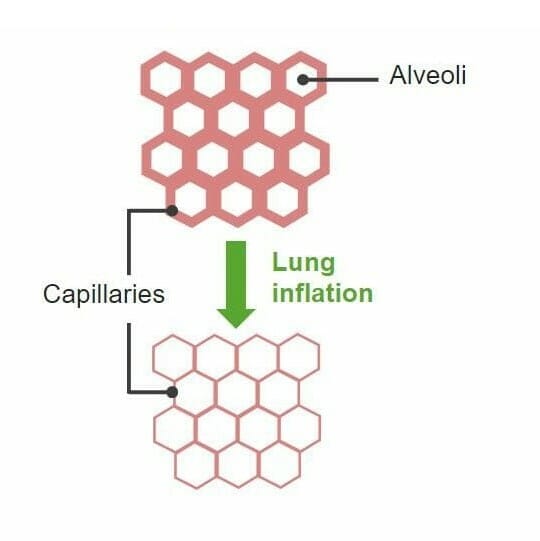
Diagram explaining the mechanisms of recruitment and distension of blood vessels when mean pulmonary arterial blood pressure is increased
Image by Lecturio. License: CC BY-NC-SA 4.0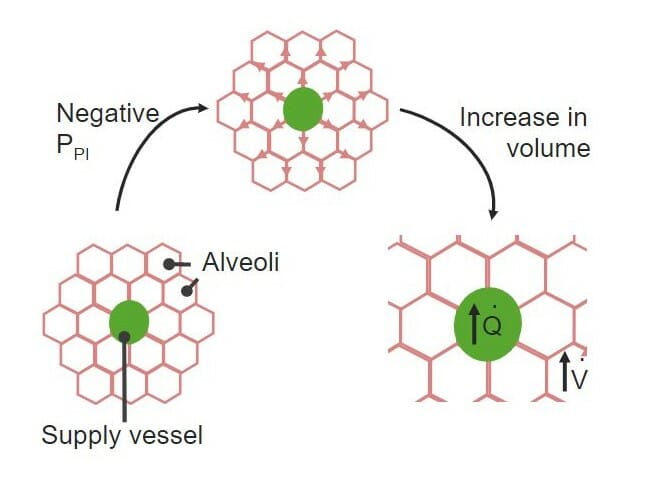
Vessel dilation effect:
The negative pleural pressure exerted on the alveoli stretches the walls of the blood vessels and increases their diameter.
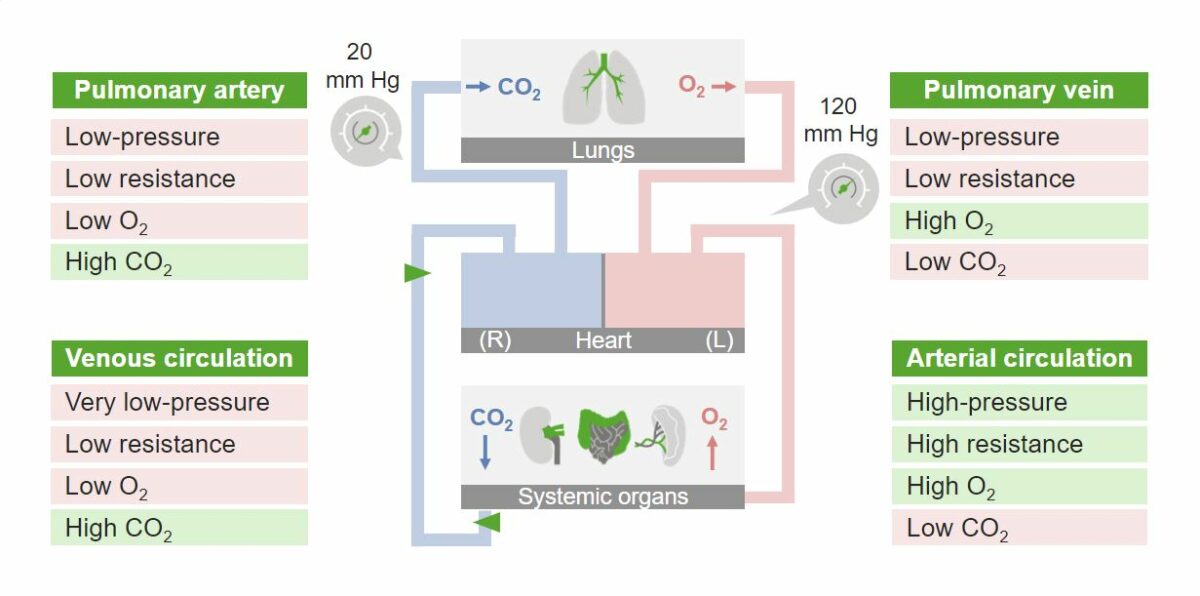
Overview of pulmonary blood flow
Image by Lecturio. License: CC BY-NC-SA 4.0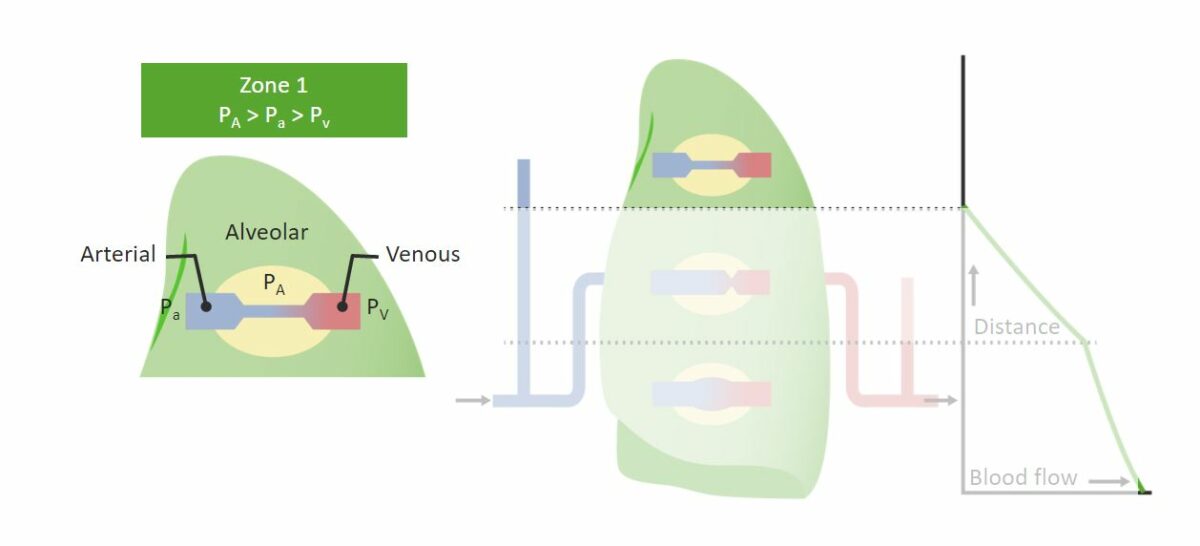
Zone 1 (Apex) of the lung and the effect of gravity on it:
Arterial pressure (Pa) is lower than alveolar pressure (PA), making the flow of blood difficult if not impossible. The relationship between pressures can be seen in the green box.
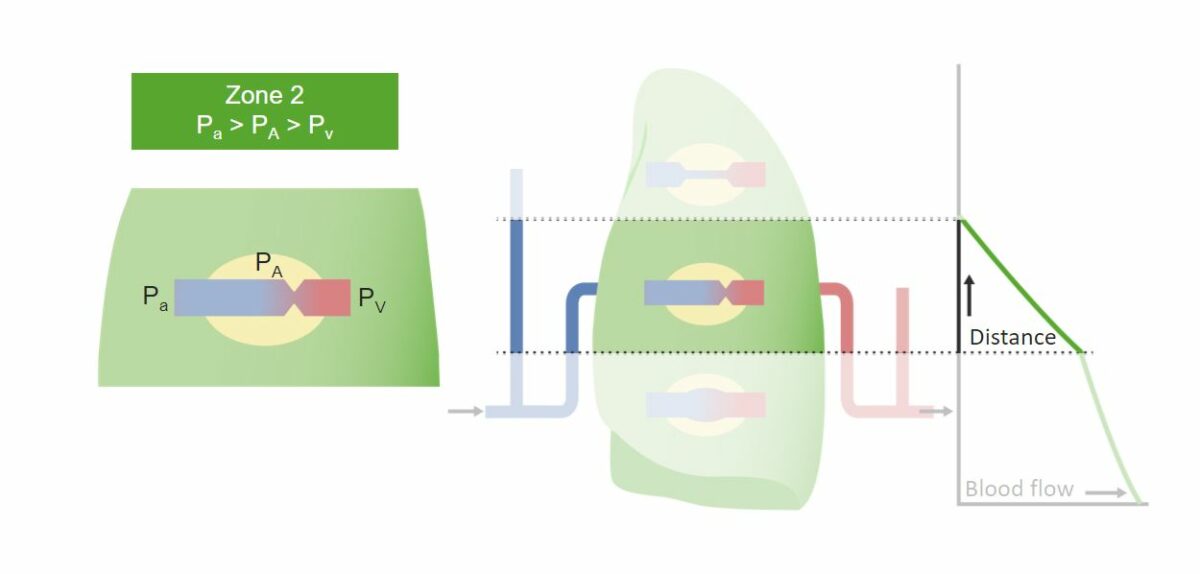
Zone 2 of the lung and the effect of gravity on it:
There’s more blood flow allowed by the increase in arterial blood pressure. The relationship between pressures can be seen in the green box.
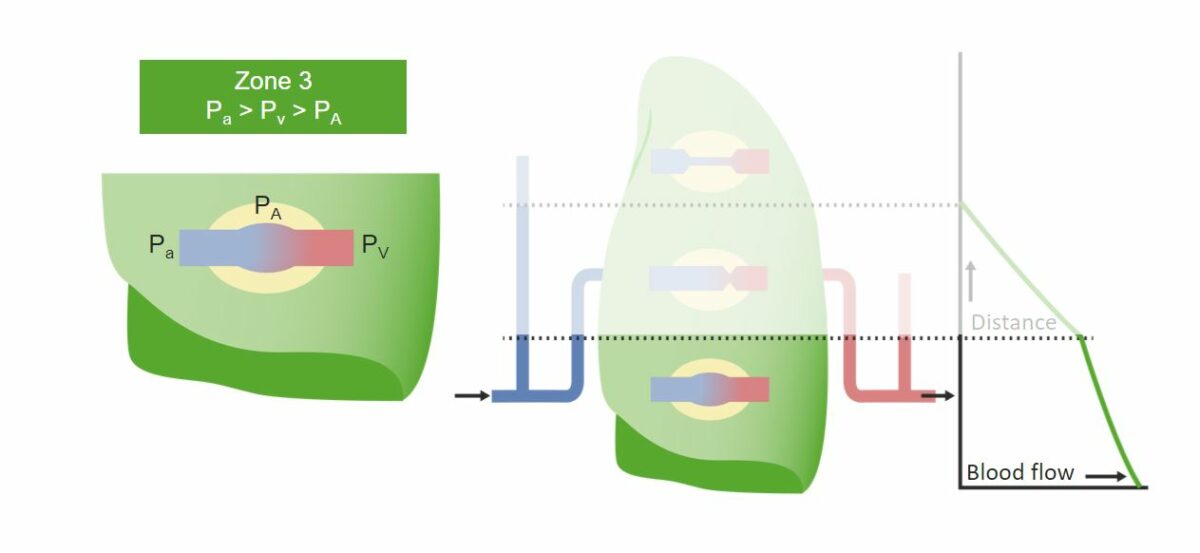
Zone 3 (Base) of the lung and the effect of gravity on it:
It’s the zone with the greatest blood flow in the lung. The pull of gravity makes more blood available and the arterial blood pressure greater than the alveolar pressure. The relationship between pressures can be seen in the green box.
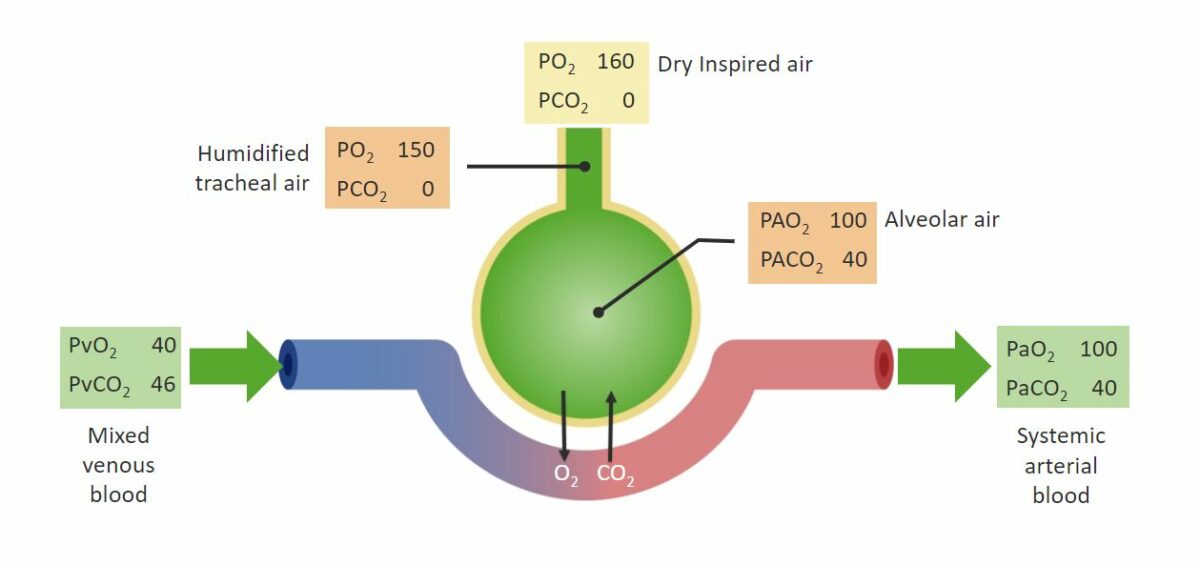
There are 2 important PO₂ differences (gradients):
Arterial-venous (a-v) difference in PO2 between venous and arterial blood:
Pressures of O2 and CO2 in the alveoli and systemic circulation before and after gas exchange.
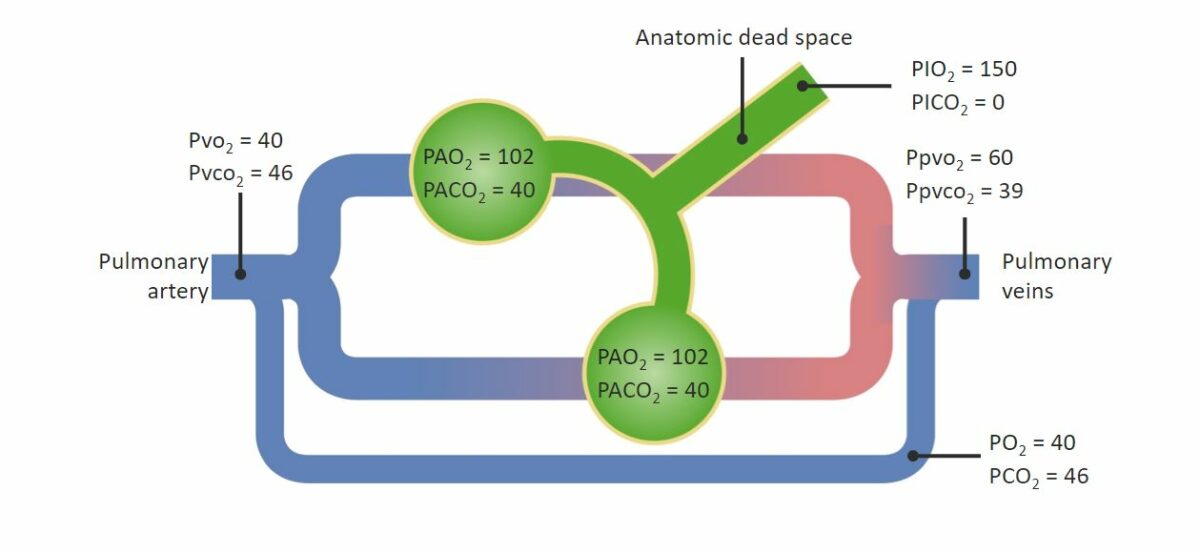
Diagram of a RIGHT-TO-LEFT shunt:
See the communication that allows blood to skip gas exchange and lower the arterial pressure of O2.
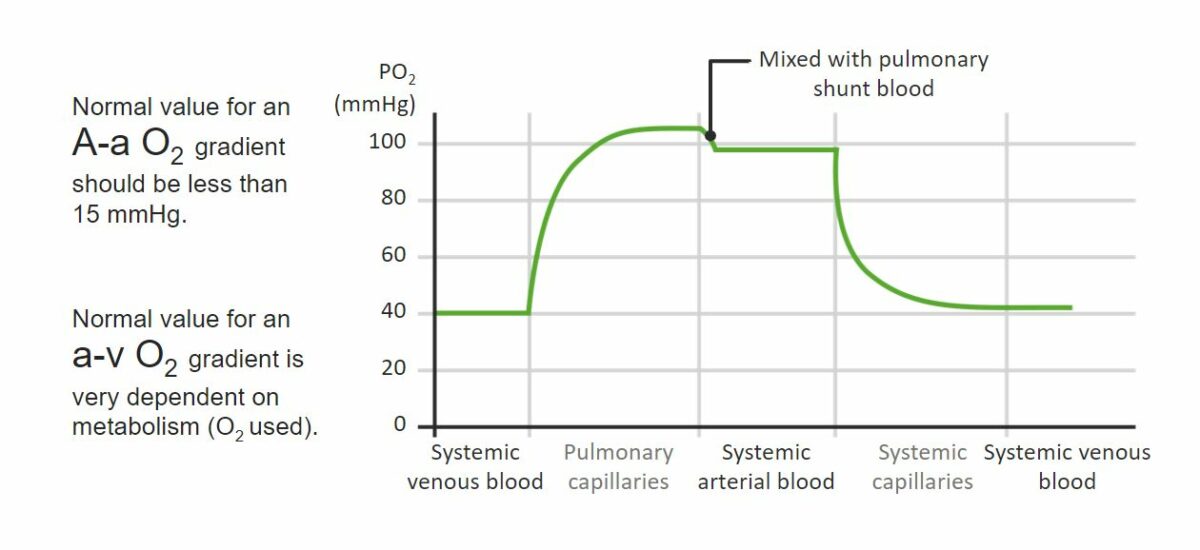
PO2 gradients in pulmonary and systemic circulations:
See the A-a gradient at the point of communication between the pulmonary capillaries and the systemic arterial circulation. The a-v gradient would be the difference between the PO2 of the systemic arterial circulation before the capillaries and the PO2 of the systemic venous circulation after the capillaries.
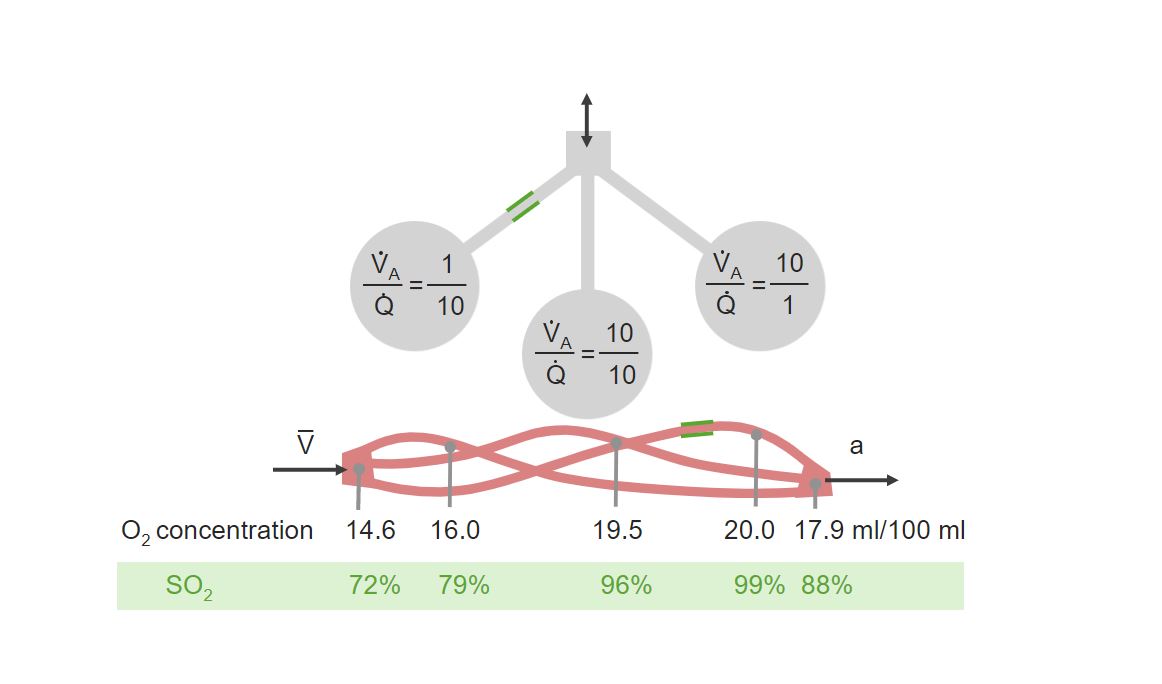
Diagrammatic examples of ventilation (V) to perfusion (Q) mismatch:
On the right, an example of low ventilation to high perfusion can be seen. On the left, an example of high ventilation to low perfusion can be seen. In the center is a normal situation of ventilation to perfusion with a relation of 1 to 1.
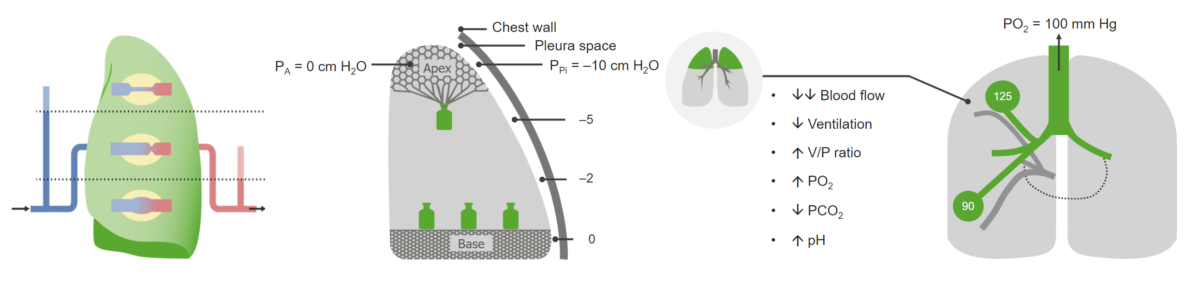
Ventilation/Perfusion relation applied to the apex of the upright lung of a healthy individual:
Reduced perfusion of the Apex (right), the inflating effect of the gravity due to the weight of the lung (center) and the resulting parameters during inspiration (right). Notice the increase of the V/Q (V/P) ratio due to the increased ventilation and the reduced perfusion.
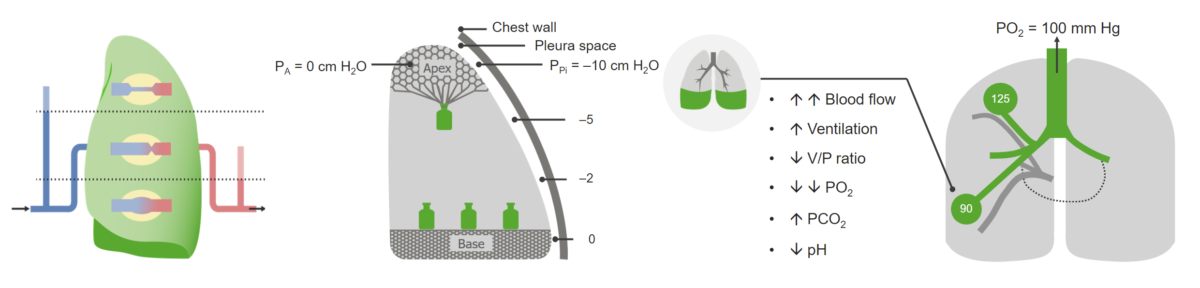
Ventilation/Perfusion relation applied to the base of the upright lung of a healthy individual:
See the increased perfusion of the Base (right), the compressing effect of the gravity due to the weight of the lung (center) and the resulting parameters during inspiration (right). The V/Q (V/P) ratio is decreased due to the increased perfusion.