The collective term “bronchial tree” refers to the bronchi and all of their subsequent branches. The bronchi are the airways of the lower respiratory tract. At the level of the 3rd or 4th thoracic vertebra, the trachea Trachea The trachea is a tubular structure that forms part of the lower respiratory tract. The trachea is continuous superiorly with the larynx and inferiorly becomes the bronchial tree within the lungs. The trachea consists of a support frame of semicircular, or C-shaped, rings made out of hyaline cartilage and reinforced by collagenous connective tissue. Trachea: Anatomy bifurcates into the left and right main bronchi. The right main bronchus is shorter and more vertical in direction than the left. Both of these bronchi continue to divide into secondary or lobar bronchi that bifurcate further and further in order to sufficiently spread the respiratory air completely into the left and right pulmonary lobes. The terminal segment of each bronchus contains millions of alveoli Alveoli Small polyhedral outpouchings along the walls of the alveolar sacs, alveolar ducts and terminal bronchioles through the walls of which gas exchange between alveolar air and pulmonary capillary blood takes place. Acute Respiratory Distress Syndrome (ARDS), the site of gas exchange Gas exchange Human cells are primarily reliant on aerobic metabolism. The respiratory system is involved in pulmonary ventilation and external respiration, while the circulatory system is responsible for transport and internal respiration. Pulmonary ventilation (breathing) represents movement of air into and out of the lungs. External respiration, or gas exchange, is represented by the O2 and CO2 exchange between the lungs and the blood. Gas Exchange.
Last updated: Nov 19, 2024
The development of the tracheobronchial tree and lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy occurs in 5 stages. The tracheobronchial tree and lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy originate from the foregut Foregut Development of the Abdominal Organs of the embryonic gut tube, beginning at week 4 of gestation and ending in childhood.
| Stage | Description | Clinical relevance |
|---|---|---|
| Embryonic period |
|
Defects:
|
| Pseudoglandular period |
|
|
| Canalicular period |
|
|
| Saccular period |
|
Infants born ≥ 32 weeks have a higher survival rate. |
| Alveolar period |
|
|
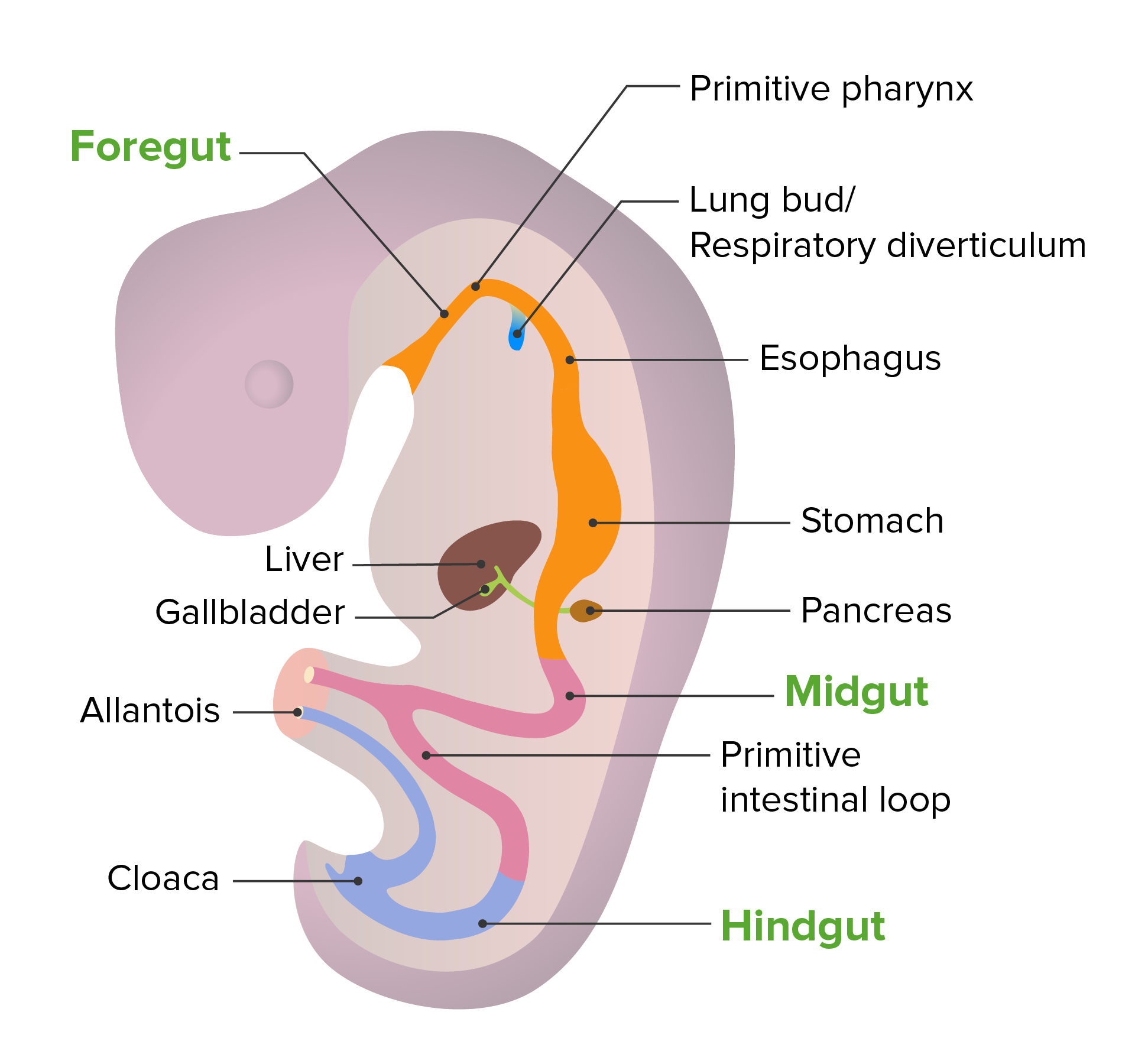
Embryonic development of the gut tube
Image by Lecturio. License: CC BY-NC-SA 4.0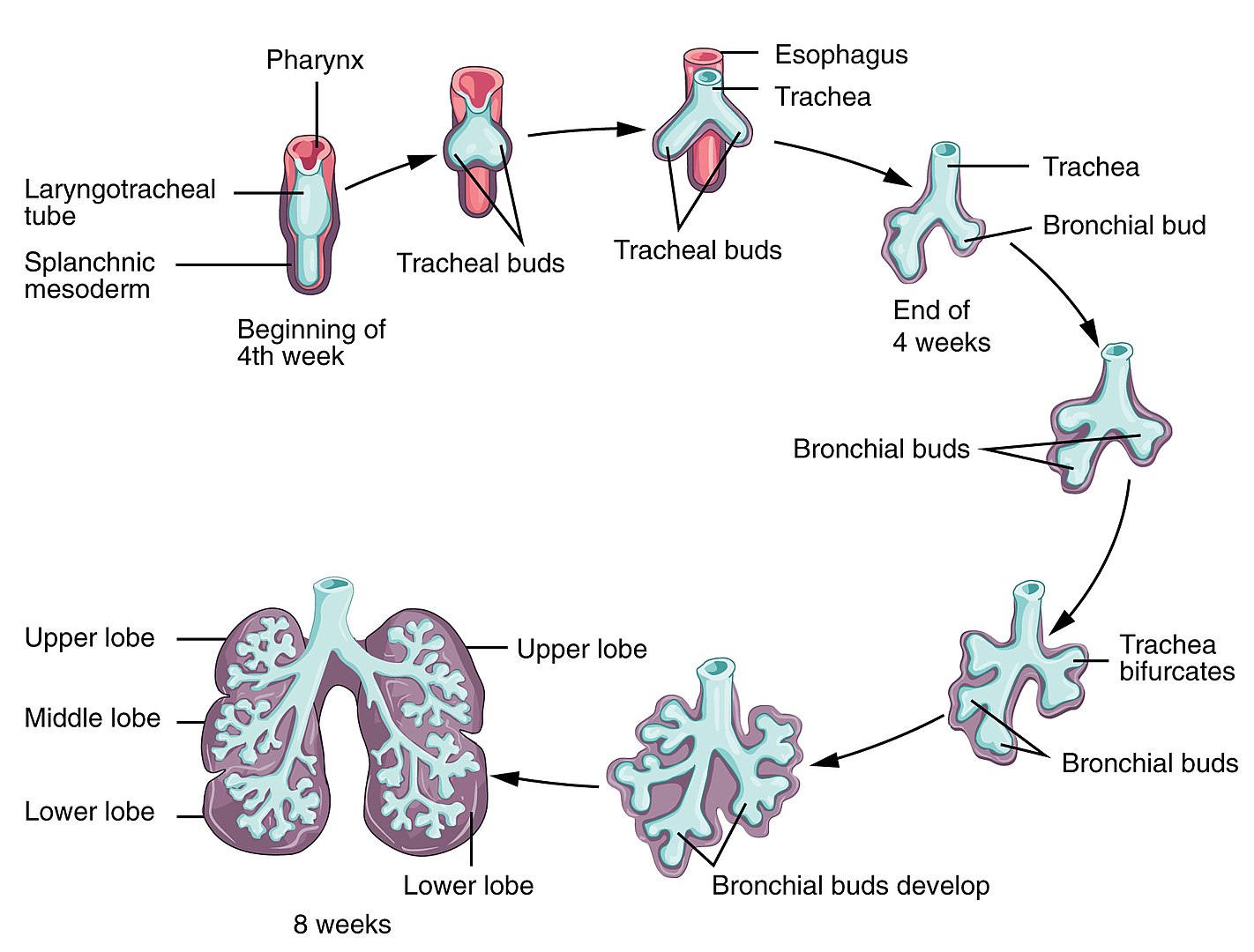
Development of the lungs:
The respiratory system begins development by week 4 of gestation. The olfactory pit forms from the ectoderm, one of the structures to become the nasal cavity. The laryngotracheal bud forms from the primitive pharynx. From this bud, the longitudinal extension becomes the tracheal and bronchial buds.
The process of elongation and branching of buds continues as conducting airways up to 16 weeks of gestation. Major maturation occurs by 24 weeks, with significant alveolar precursors developing and an increased amount of surfactant produced. By 28 weeks of gestation, there usually will be enough mature alveoli.
The bronchial tree begins at the bifurcation of the trachea Trachea The trachea is a tubular structure that forms part of the lower respiratory tract. The trachea is continuous superiorly with the larynx and inferiorly becomes the bronchial tree within the lungs. The trachea consists of a support frame of semicircular, or C-shaped, rings made out of hyaline cartilage and reinforced by collagenous connective tissue. Trachea: Anatomy at the carina, approximately at the level of T5. The trachea Trachea The trachea is a tubular structure that forms part of the lower respiratory tract. The trachea is continuous superiorly with the larynx and inferiorly becomes the bronchial tree within the lungs. The trachea consists of a support frame of semicircular, or C-shaped, rings made out of hyaline cartilage and reinforced by collagenous connective tissue. Trachea: Anatomy bifurcates into the main left and right bronchi, These bronchi continue to branch until they form alveoli Alveoli Small polyhedral outpouchings along the walls of the alveolar sacs, alveolar ducts and terminal bronchioles through the walls of which gas exchange between alveolar air and pulmonary capillary blood takes place. Acute Respiratory Distress Syndrome (ARDS), the site of gas exchange Gas exchange Human cells are primarily reliant on aerobic metabolism. The respiratory system is involved in pulmonary ventilation and external respiration, while the circulatory system is responsible for transport and internal respiration. Pulmonary ventilation (breathing) represents movement of air into and out of the lungs. External respiration, or gas exchange, is represented by the O2 and CO2 exchange between the lungs and the blood. Gas Exchange. Each bronchial segment progressively becomes smaller in diameter and has a thinner wall.
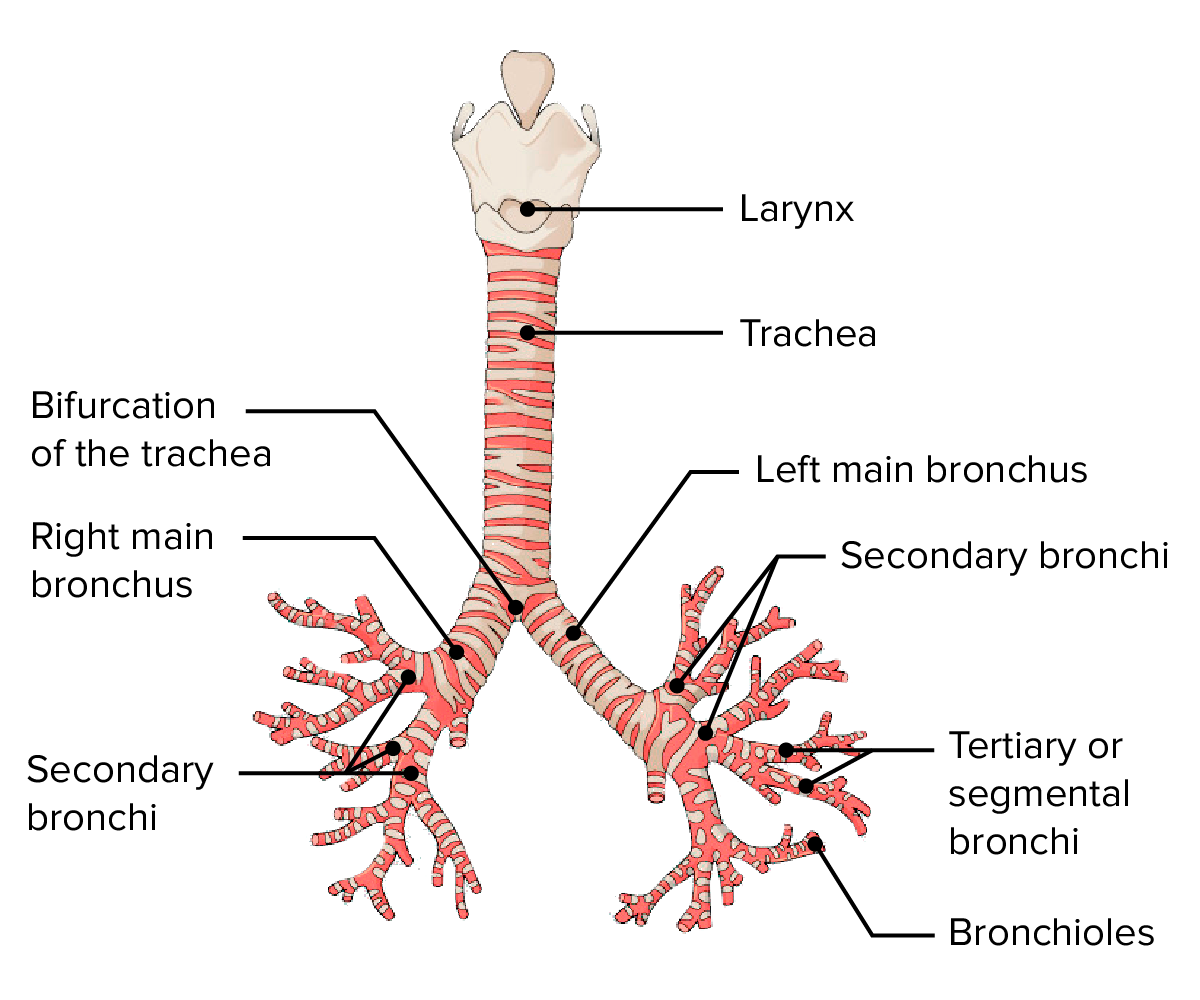
Anterior view of the larynx, trachea, and bronchial tree:
Note the main divisions of the bronchi.
Blood supply:
The bronchial tree is supplied by branches of the left and right bronchial arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology.
Venous drainage:
Innervation:
Innervation is supplied by the pulmonary plexus of the vagus nerve Vagus nerve The 10th cranial nerve. The vagus is a mixed nerve which contains somatic afferents (from skin in back of the ear and the external auditory meatus), visceral afferents (from the pharynx, larynx, thorax, and abdomen), parasympathetic efferents (to the thorax and abdomen), and efferents to striated muscle (of the larynx and pharynx). Pharynx: Anatomy.
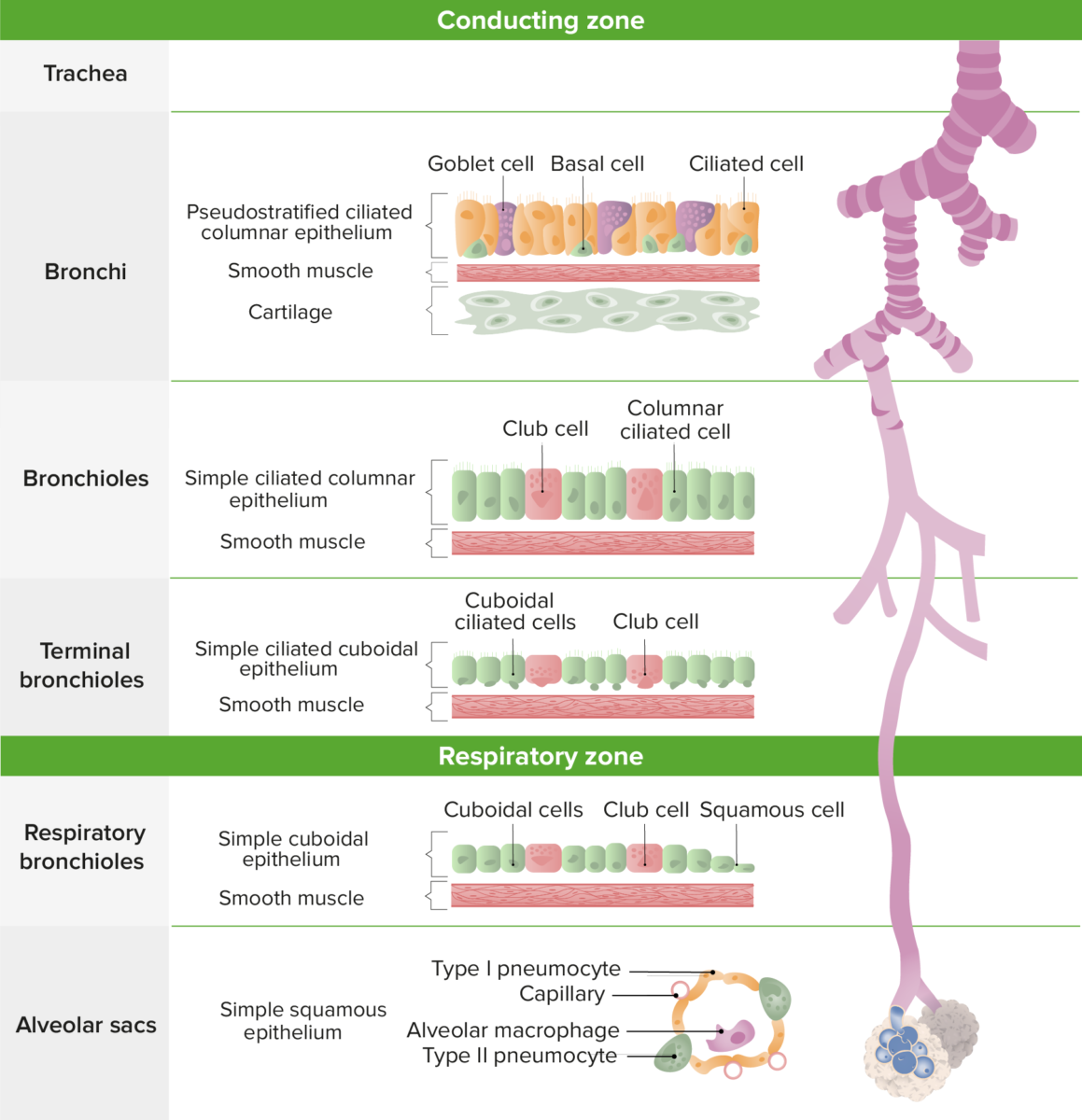
Microscopic anatomy of the lower respiratory tract
Image by Lecturio. License: CC BY-NC-SA 4.0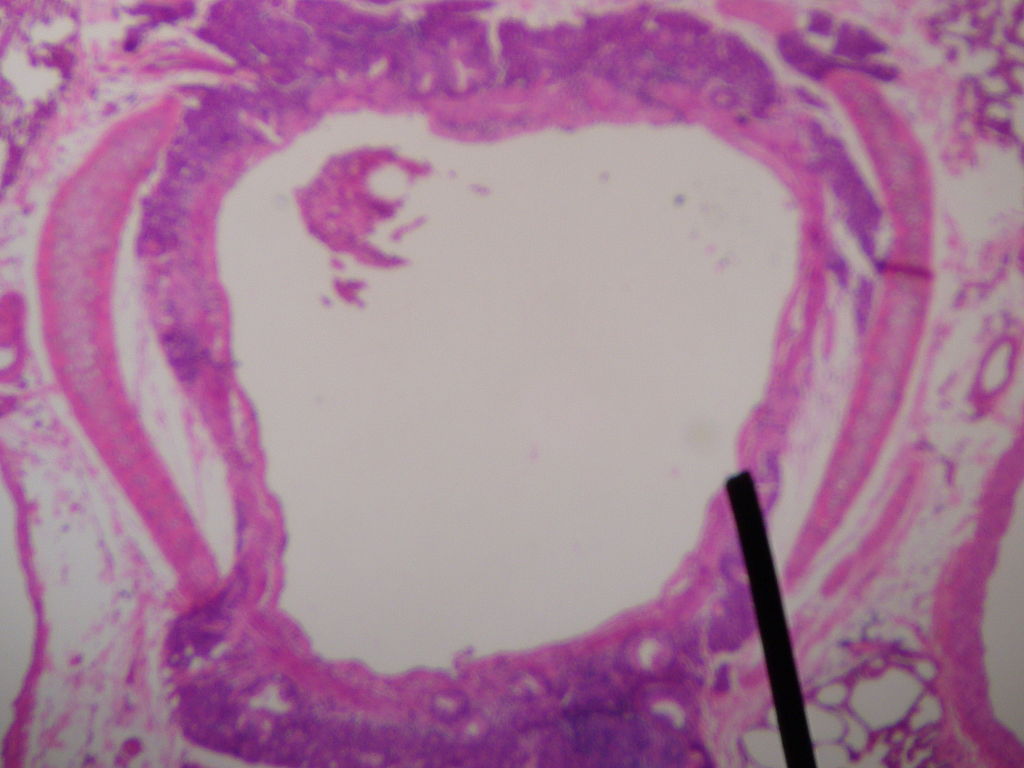
Cross-section of a secondary bronchus
Image: “Cross-section of secondary bronchus” by Jpogi. License: Public Domain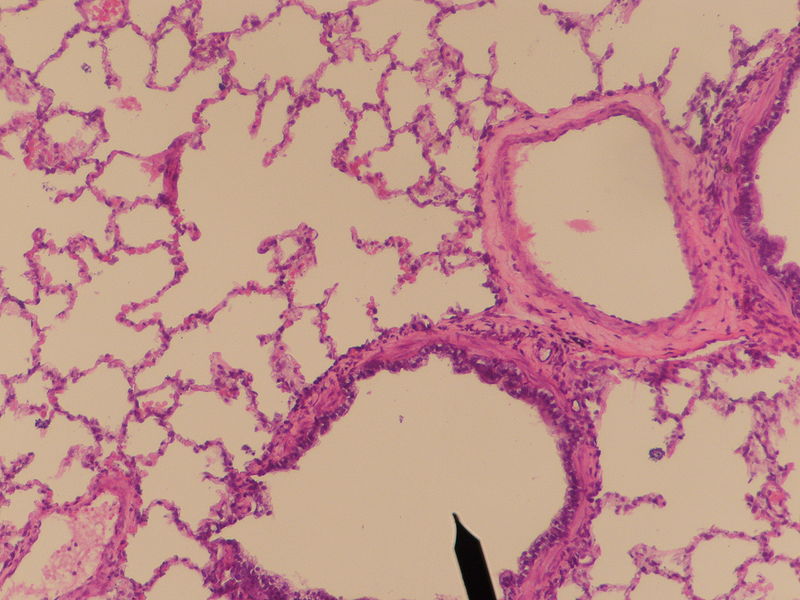
Cross-section of a tertiary bronchus
Image: “Tertiary bronchus” by Jpogi. License: Public Domain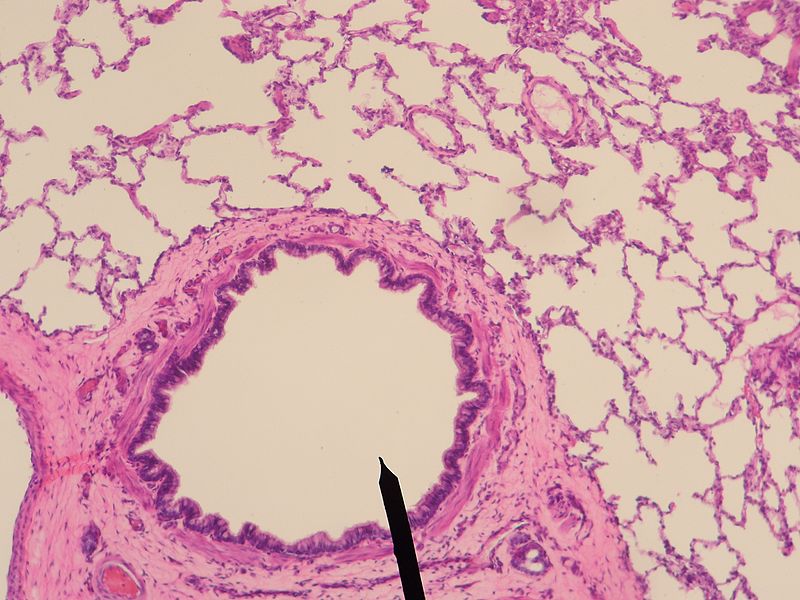
Cross-section of terminal bronchiole
Image: “Terminal bronchiole” by Jpogi. License: Public DomainThe following are conditions that can affect the bronchial tree: