The trachea is a tubular structure that forms part of the lower respiratory tract. The trachea is continuous superiorly with the larynx Larynx The larynx, also commonly called the voice box, is a cylindrical space located in the neck at the level of the C3-C6 vertebrae. The major structures forming the framework of the larynx are the thyroid cartilage, cricoid cartilage, and epiglottis. The larynx serves to produce sound (phonation), conducts air to the trachea, and prevents large molecules from reaching the lungs. Larynx: Anatomy and inferiorly becomes the bronchial tree Bronchial tree The collective term "bronchial tree" refers to the bronchi and all of their subsequent branches. The bronchi are the airways of the lower respiratory tract. At the level of the 3rd or 4th thoracic vertebra, the trachea bifurcates into the left and right main bronchi. Both of these bronchi continue to divide into secondary or lobar bronchi that bifurcate further and further. Bronchial Tree: Anatomy within the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy. The trachea consists of a support frame of 16–20 semicircular, or C-shaped, rings made out of hyaline cartilage Hyaline cartilage A type of cartilage characterized by a homogeneous amorphous matrix containing predominantly type II collagen and ground substance. Hyaline cartilage is found in articular cartilage; costal cartilage; laryngeal cartilages; and the nasal septum. Cartilage: Histology and reinforced by collagenous connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology. The posterior wall of the trachea is free of cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology. In this area, the paries membranaceus forms a plate out of smooth tracheal muscle and connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology and forms the border to the dorsally running esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy.
Last updated: Nov 19, 2024
The trachea develops as part of the tracheobronchial tree by budding Budding Mycology off of the foregut Foregut Development of the Abdominal Organs of the embryonic gut tube.
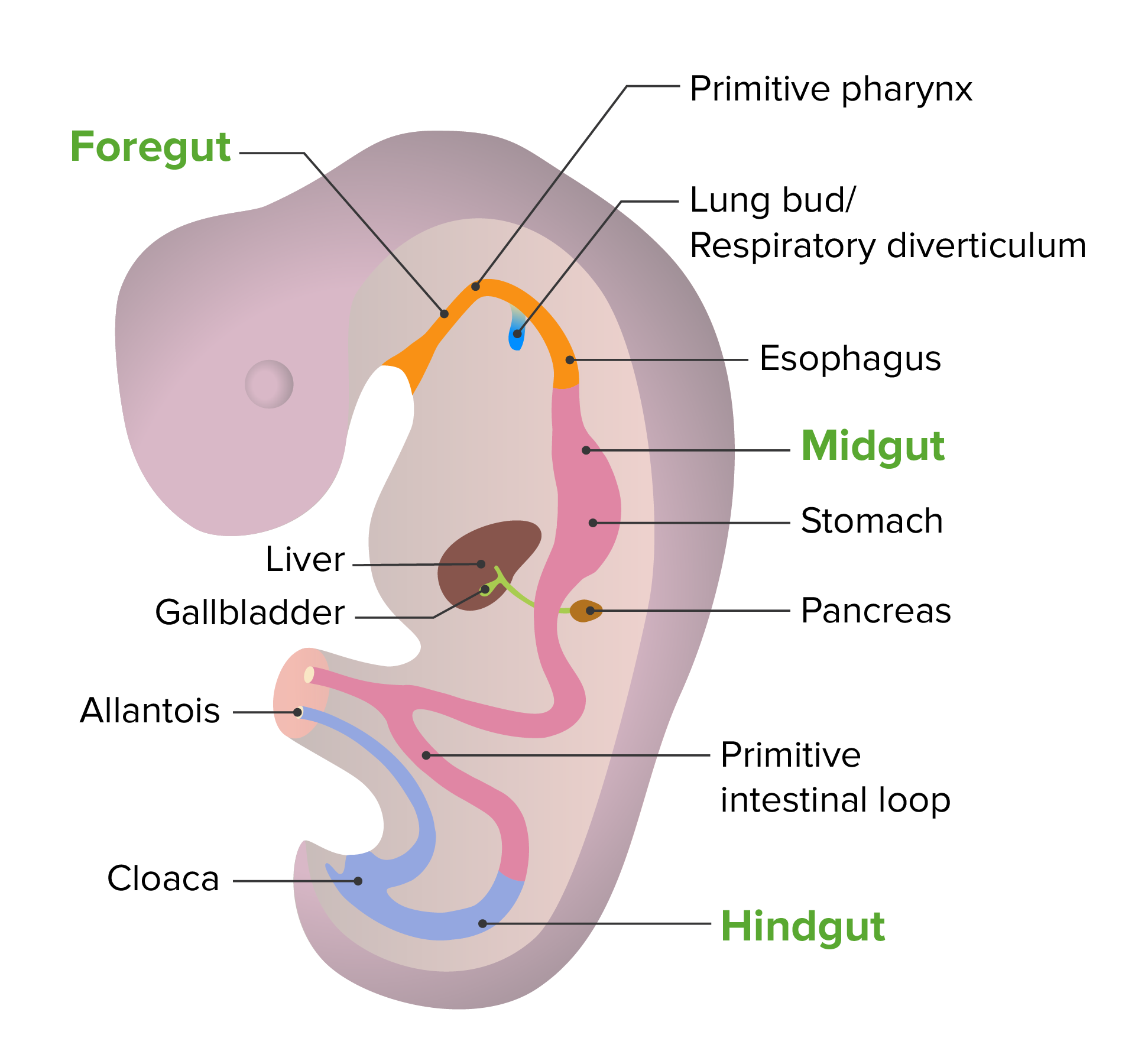
Embryonic development of the gut tube
Image by Lecturio. License: CC BY-NC-SA 4.0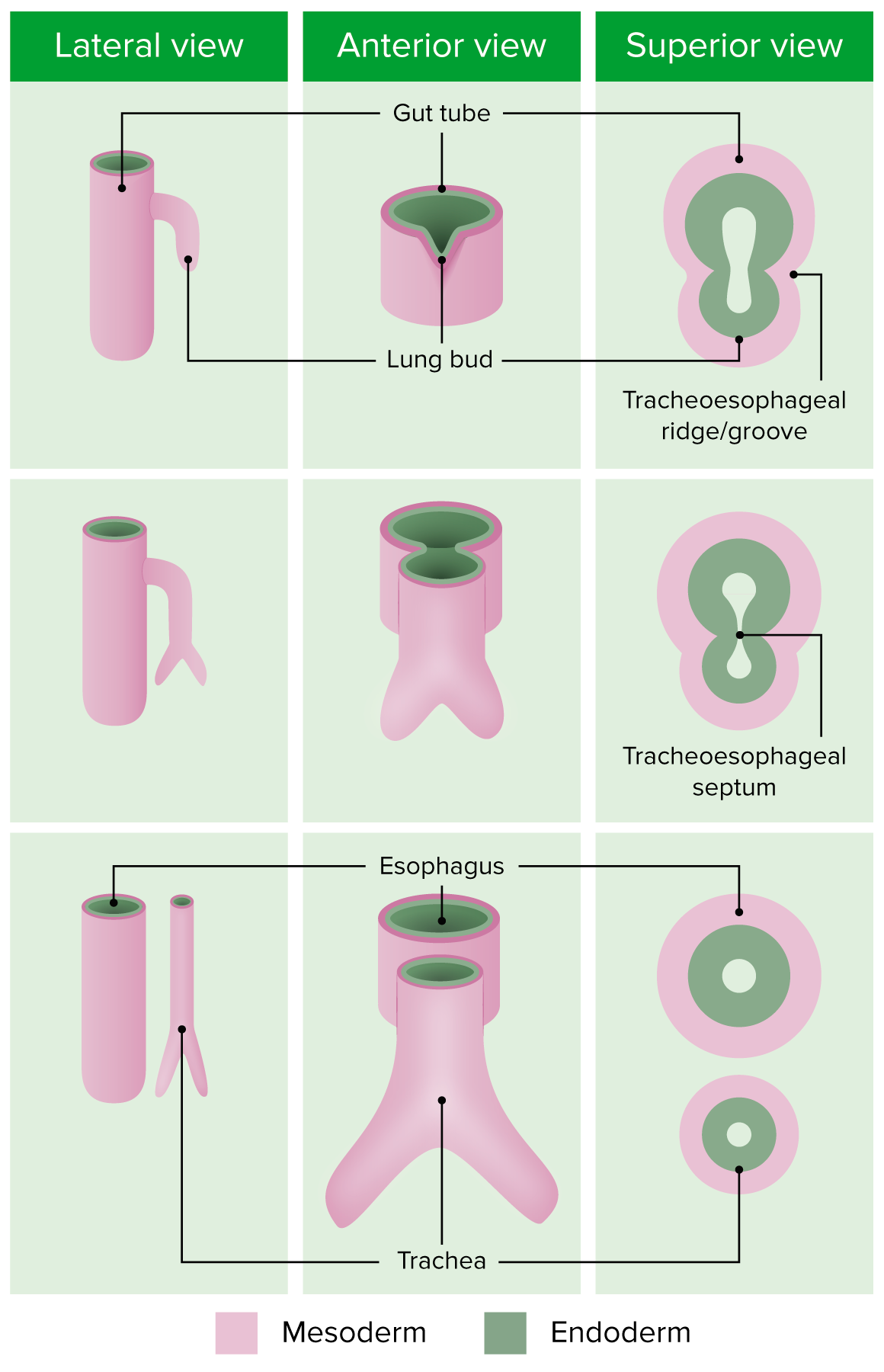
Embryonic development of the bronchial tree
Image by Lecturio. License: CC BY-NC-SA 4.0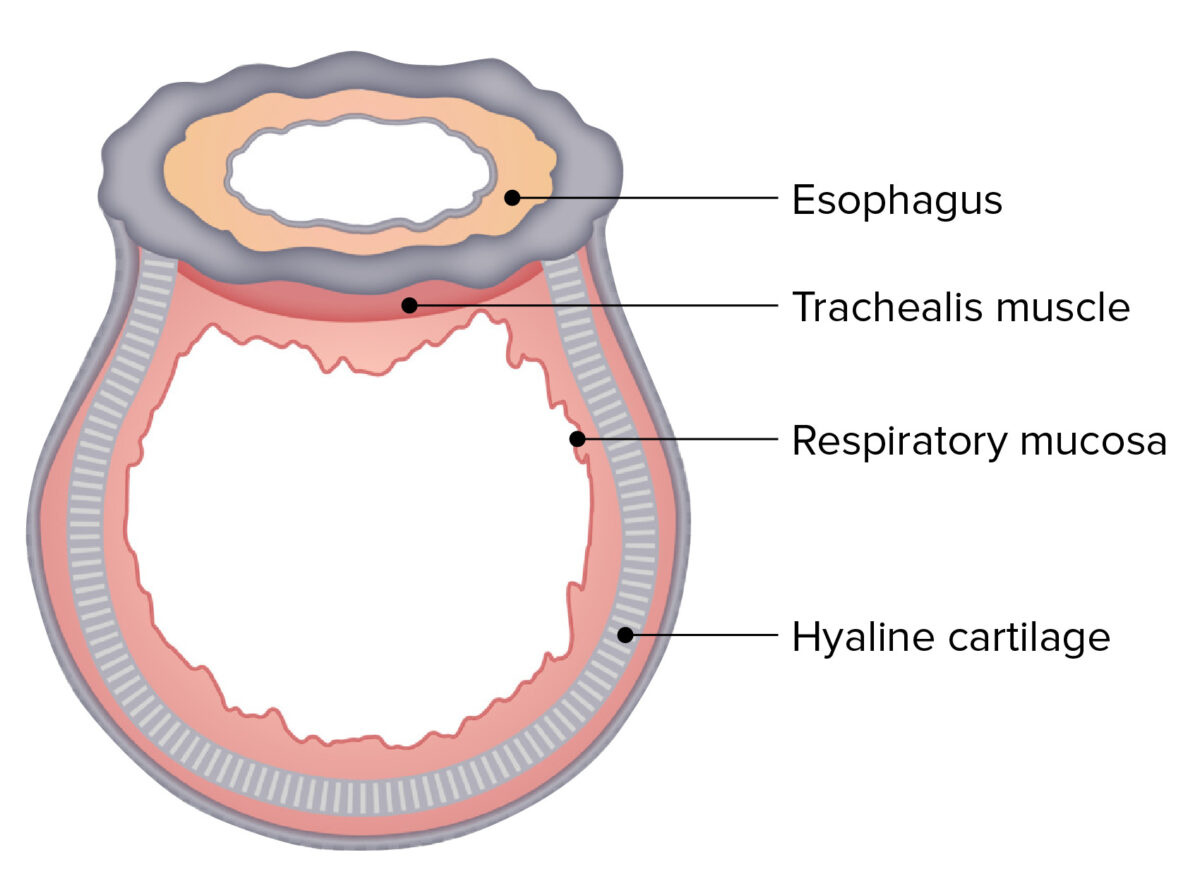
The cross-sectional structure of the trachea:
Note the D-shaped, tubular structure and the close proximity to the esophagus.
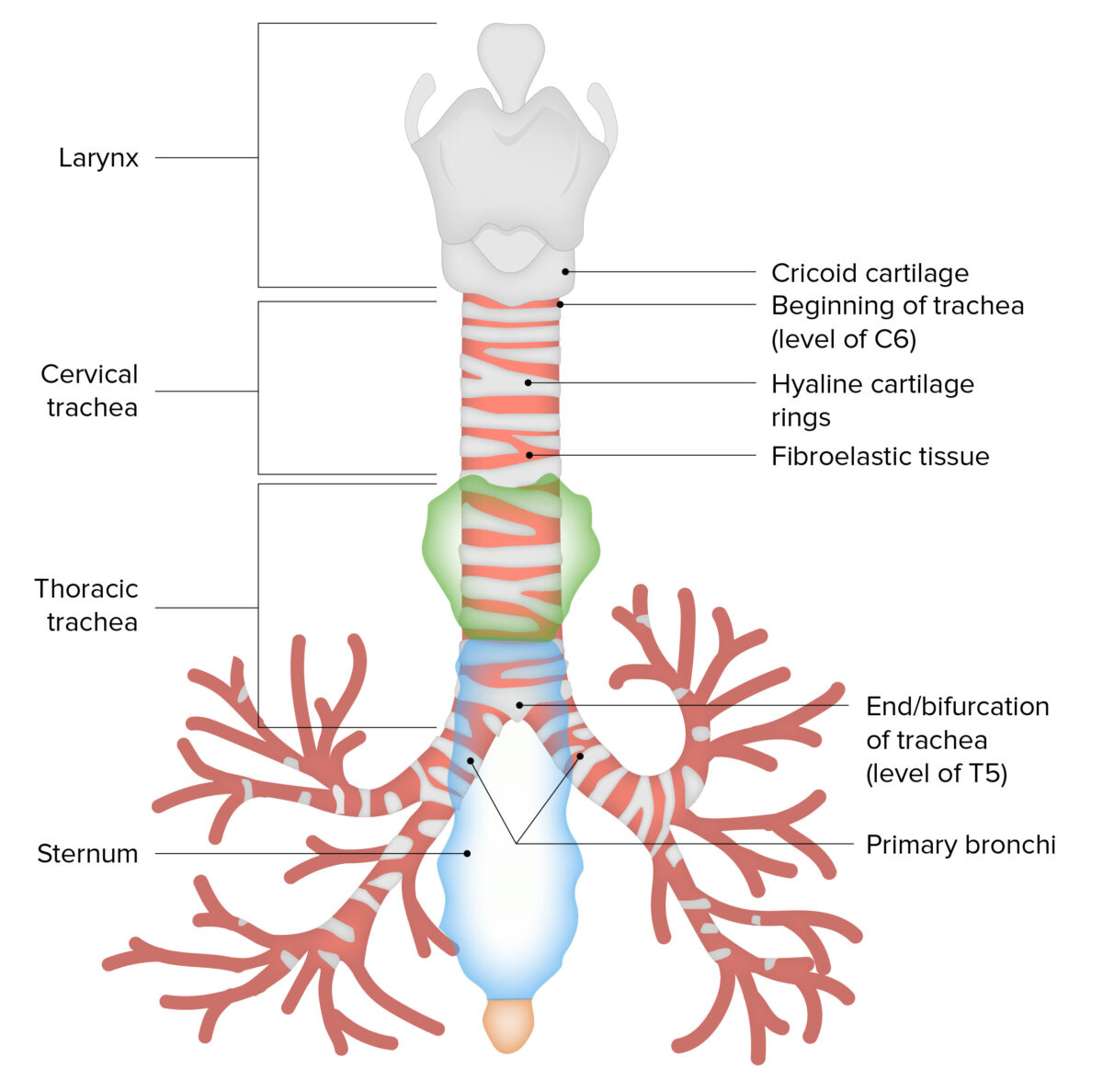
The main structure and portions of the trachea
Image by Lecturio. License: CC BY-NC-SA 4.0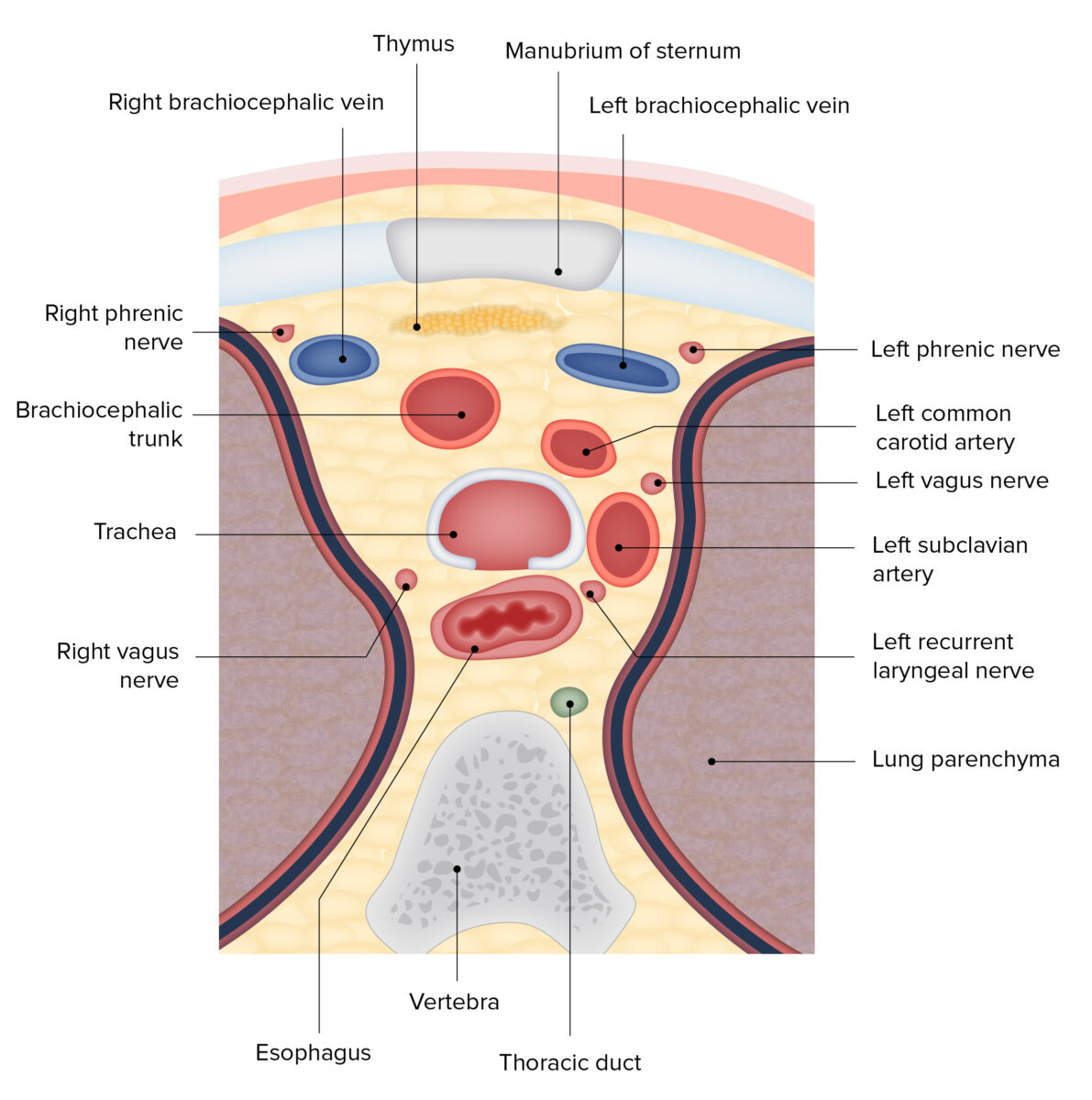
Diagram of a cross section of the superior mediastinum, featuring the spatial relations of the trachea
Image by BioDigital, edited by Lecturio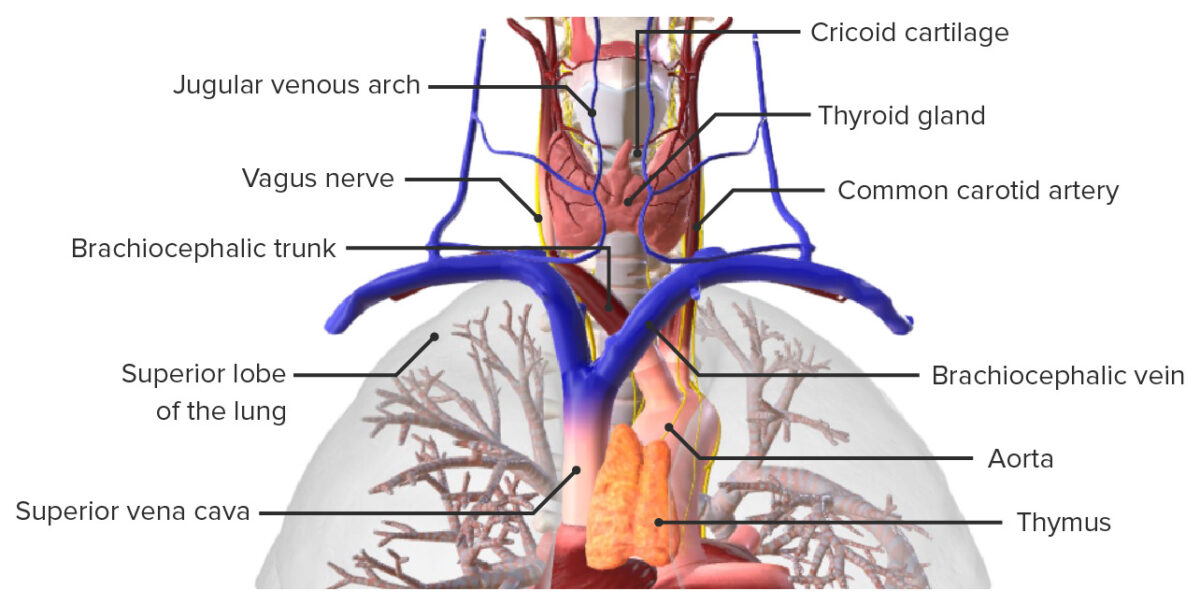
Anterior view of the trachea, featuring its spatial relations to neighboring structures
Image by BioDigital, edited by Lecturio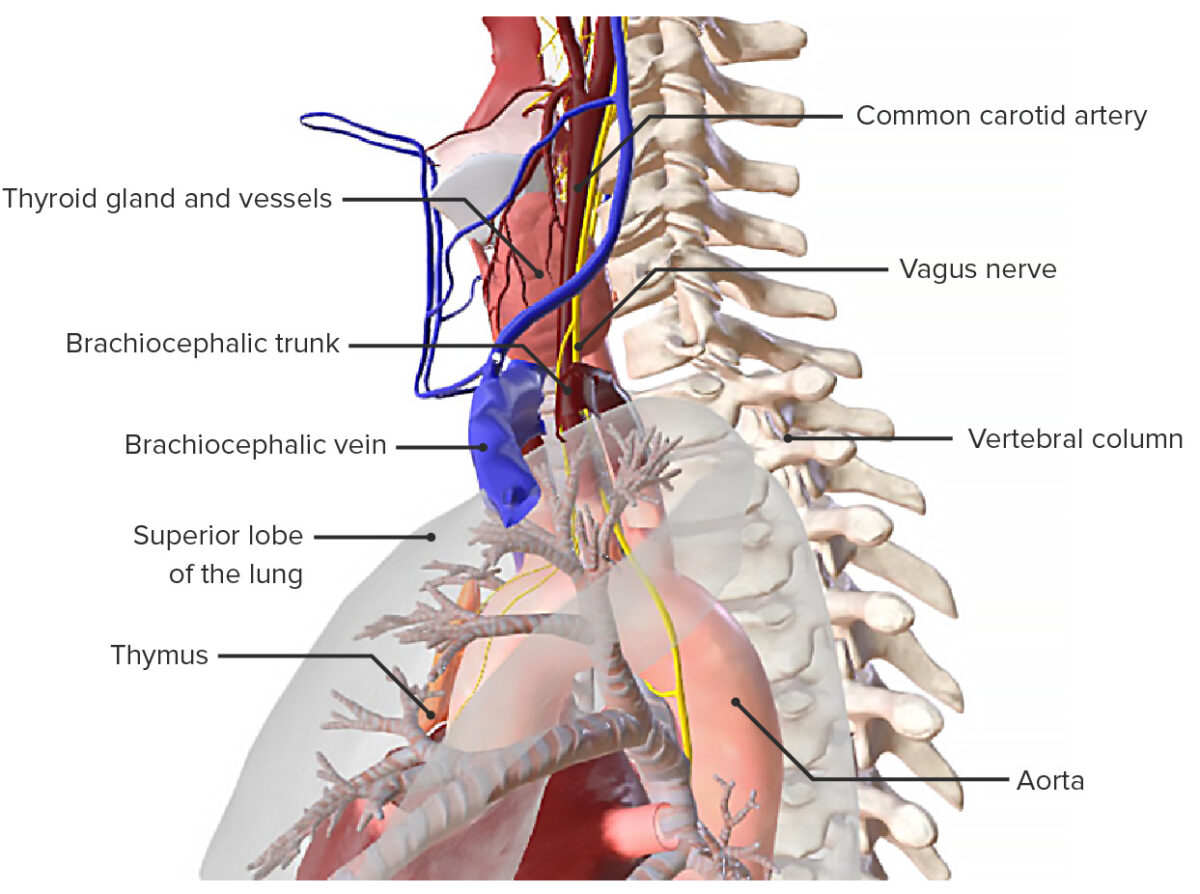
Lateral view of the trachea, featuring its spatial relations to neighboring structures
Image by BioDigital, edited by LecturioThe tracheal wall consists of 4 layers:
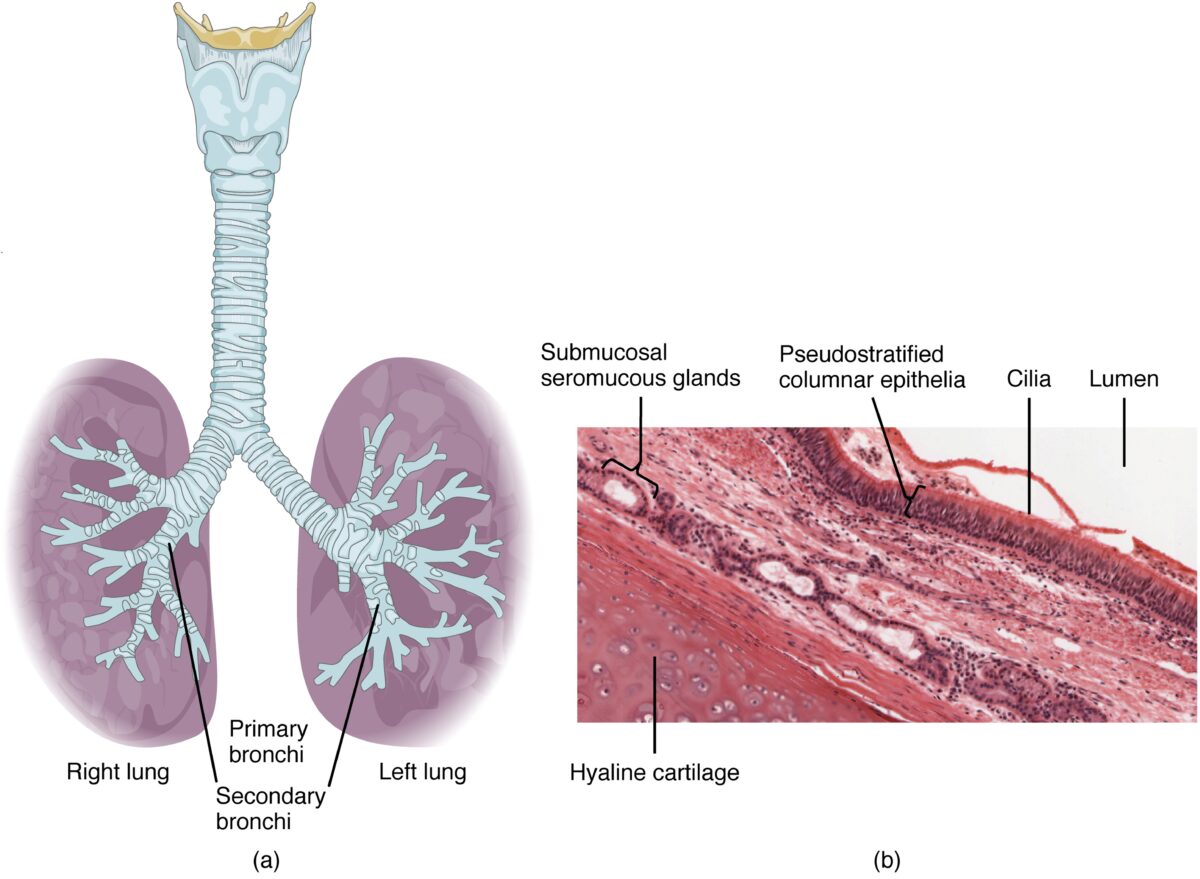
The various layers of tissue that comprise the trachea
Image: “Layers of tissue: trachea and larynx” by Phil Schatz. License: CC BY 4.0, edited by Lecturio.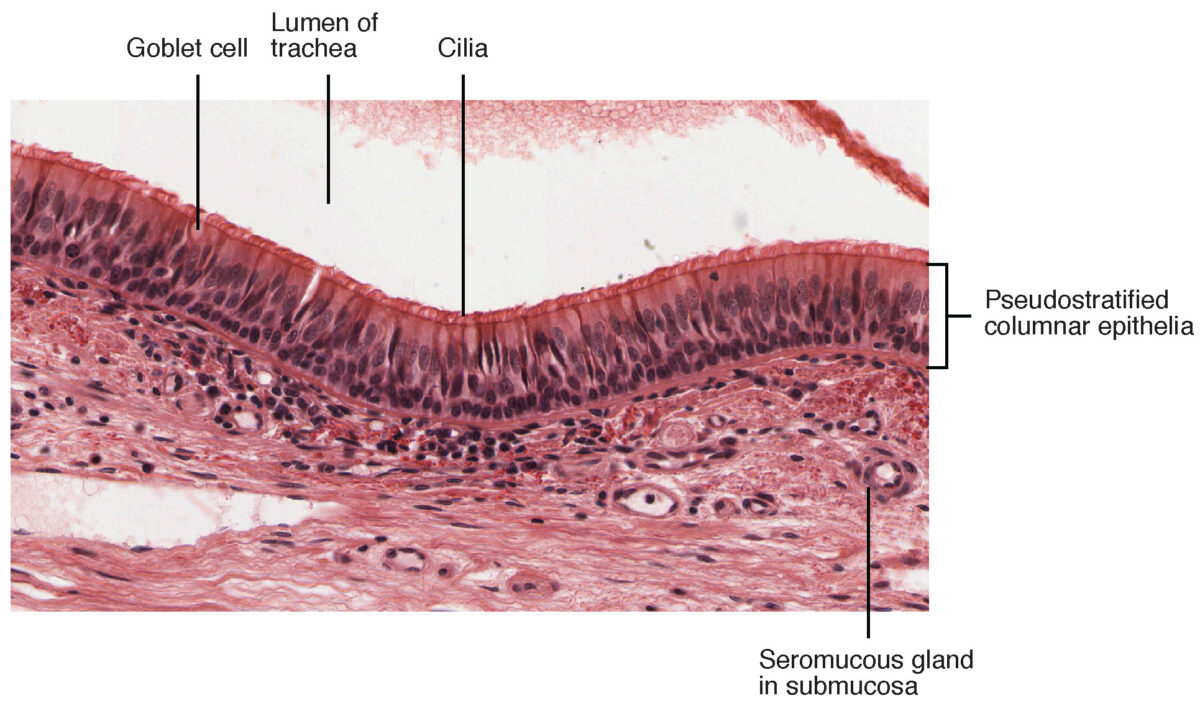
Close-up of the histologic layers of the tracheal lumen
Image: “Pseudostratified Epithelium” by OpenStax College. License: CC BY 3.0The following conditions of various origins can affect the trachea: