The thyroid gland is one of the largest endocrine glands Endocrine glands Ductless glands that secrete hormones directly into the blood circulation. These hormones influence the metabolism and other functions of cells in the body. Glandular Epithelium: Histology in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess, spanning the regions between the C5 and T1 vertebrae and encircling the anterolateral trachea Trachea The trachea is a tubular structure that forms part of the lower respiratory tract. The trachea is continuous superiorly with the larynx and inferiorly becomes the bronchial tree within the lungs. The trachea consists of a support frame of semicircular, or C-shaped, rings made out of hyaline cartilage and reinforced by collagenous connective tissue. Trachea: Anatomy. The left and right lobes of the thyroid gland are connected by a central isthmus Isthmus Uterus, Cervix, and Fallopian Tubes: Anatomy. Important processes in metabolism, growth, cardiac function, and calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes homeostasis Homeostasis The processes whereby the internal environment of an organism tends to remain balanced and stable. Cell Injury and Death are regulated by the thyroid hormones Thyroid hormones The 2 primary thyroid hormones are triiodothyronine (T3) and thyroxine (T4). These hormones are synthesized and secreted by the thyroid, and they are responsible for stimulating metabolism in most cells of the body. Their secretion is regulated primarily by thyroid-stimulating hormone (TSH), which is produced by the pituitary gland. Thyroid Hormones ( thyroxine Thyroxine The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroid Hormones and triiodothyronine Triiodothyronine A T3 thyroid hormone normally synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4). Most T3 is derived from peripheral monodeiodination of T4 at the 5' position of the outer ring of the iodothyronine nucleus. The hormone finally delivered and used by the tissues is mainly t3. Thyroid Hormones) and calcitonin Calcitonin A peptide hormone that lowers calcium concentration in the blood. In humans, it is released by thyroid cells and acts to decrease the formation and absorptive activity of osteoclasts. Its role in regulating plasma calcium is much greater in children and in certain diseases than in normal adults. Other Antiresorptive Drugs.
Last updated: Nov 19, 2024
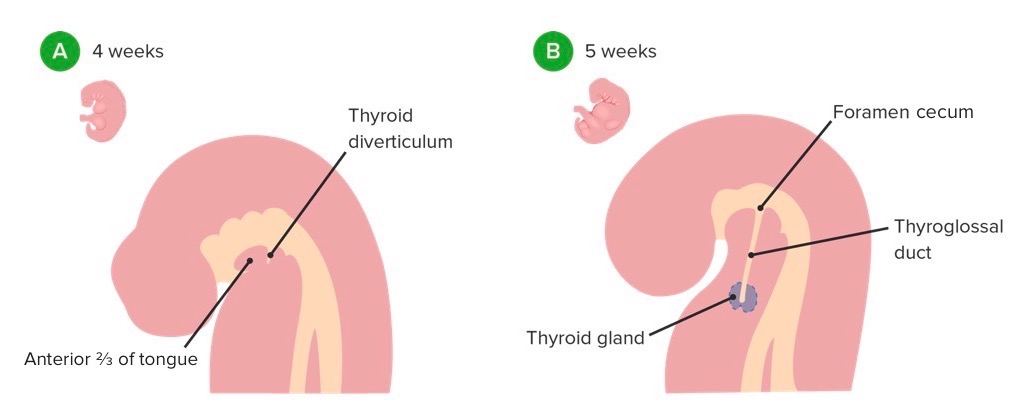
Thyroid diverticulum formation and migration
Image by Lecturio.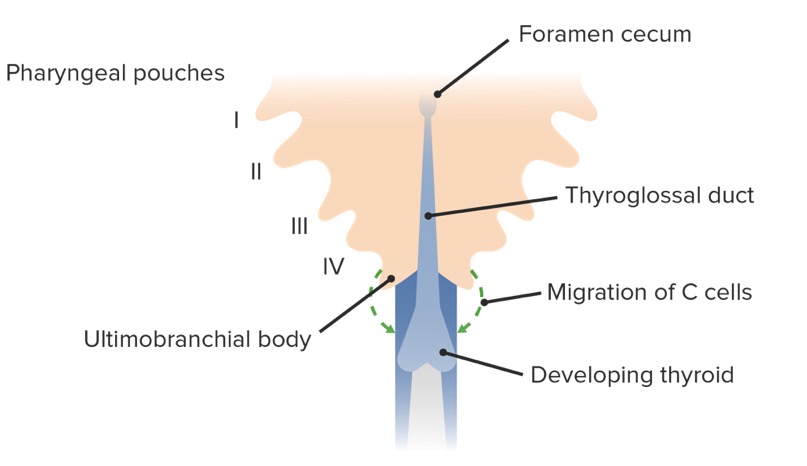
Thyroid gland development and migration of C cells from the ultimobranchial bodies
Image by Lecturio.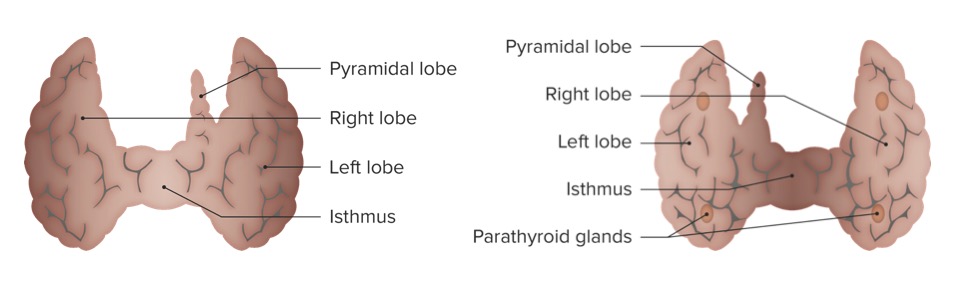
Anterior (left) and posterior (right) views of the thyroid gland
Image by Lecturio.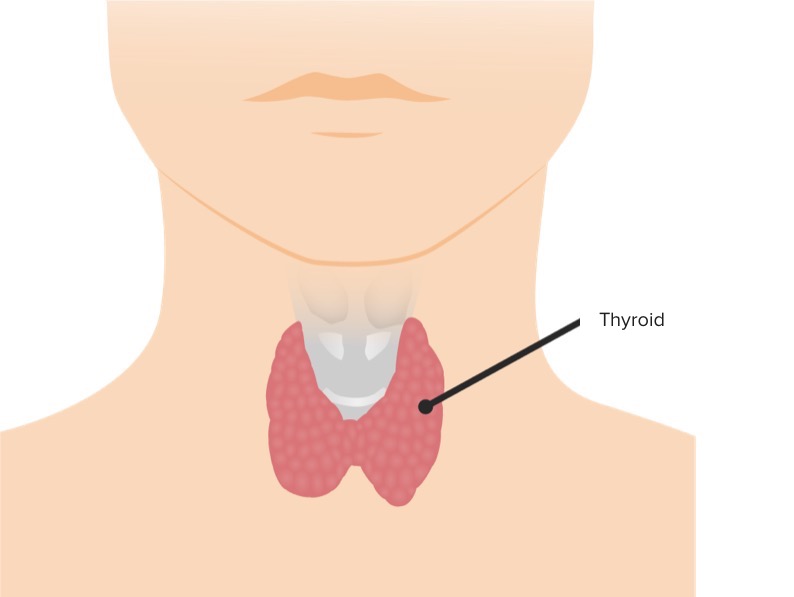
The thyroid gland and its location in relation to the trachea
Image by Lecturio.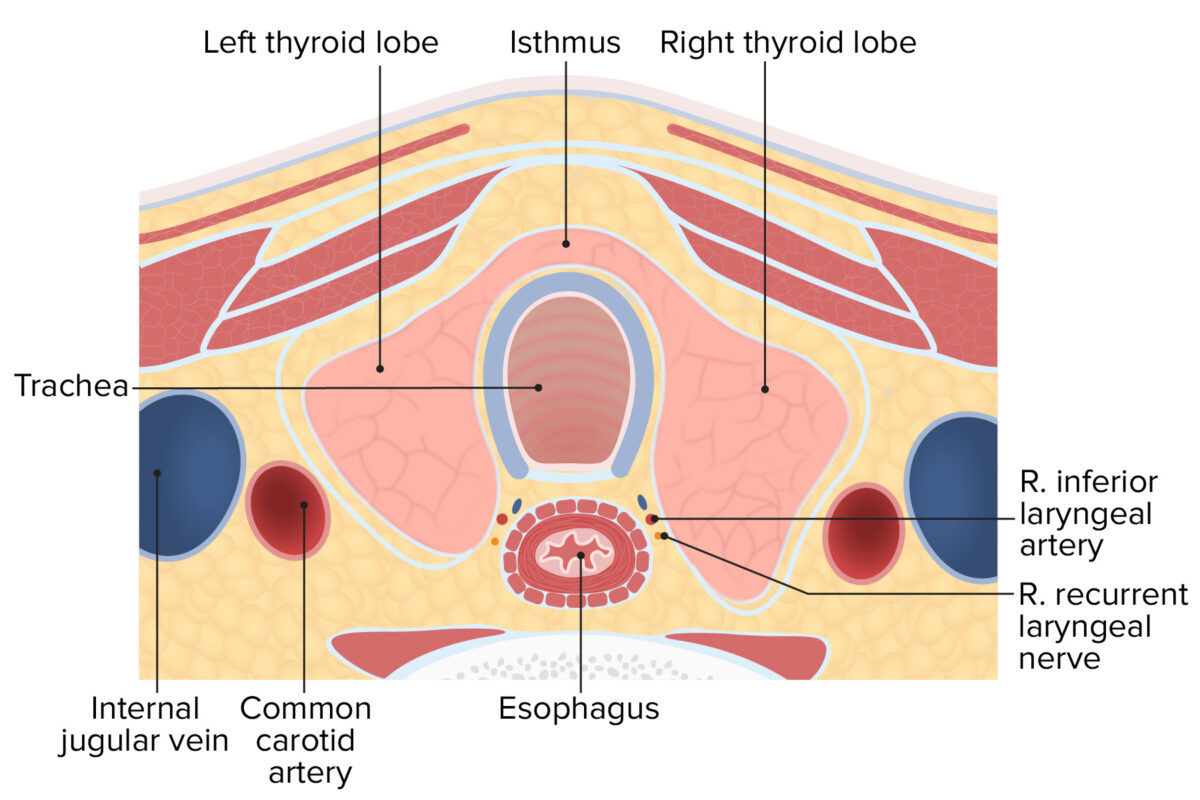
Cross-section of the neck displaying the lobules and isthmus of the thyroid gland
Image by Lecturio.Thyroid follicles are the structural and functional units of the thyroid glands. Thyroid follicles are composed of a simple epithelial layer that encloses a colloid-filled cavity.
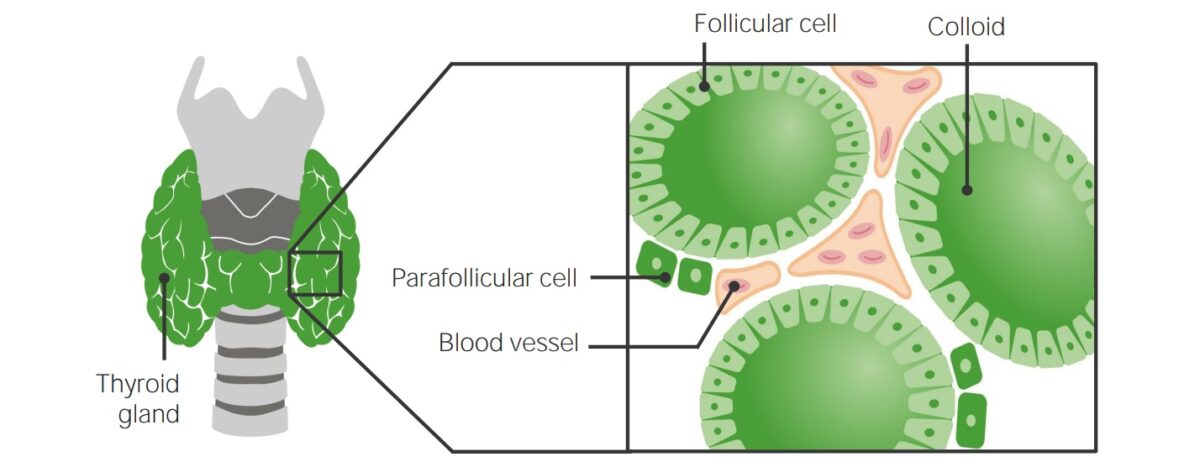
Histologic structure of the thyroid gland
Image by Lecturio.Also known as clear, light, or parafollicular cells.
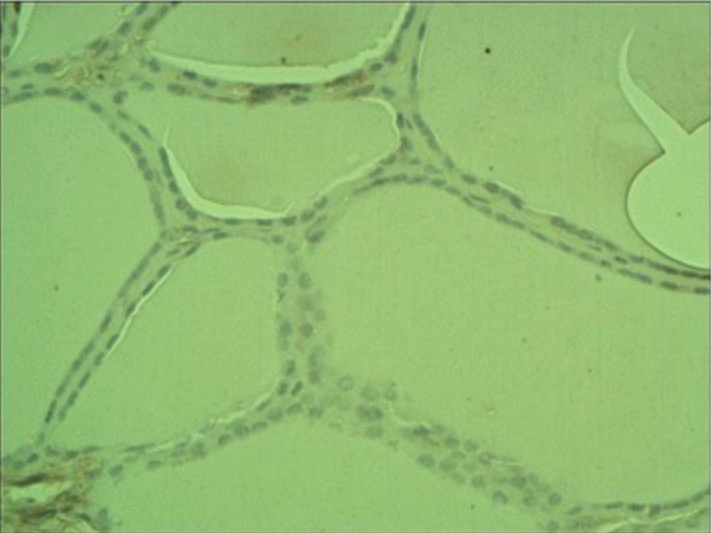
Non-neoplastic thyroid epithelium
Image: “Non-neoplastic thyroid epithelium” by Department of Immunoendocrinology, Chair of Endocrinology, Medical University of Lodz, Lodz, Poland. License: CC BY 4.0Multiple anastomoses are present, both ipsilaterally and contralaterally.
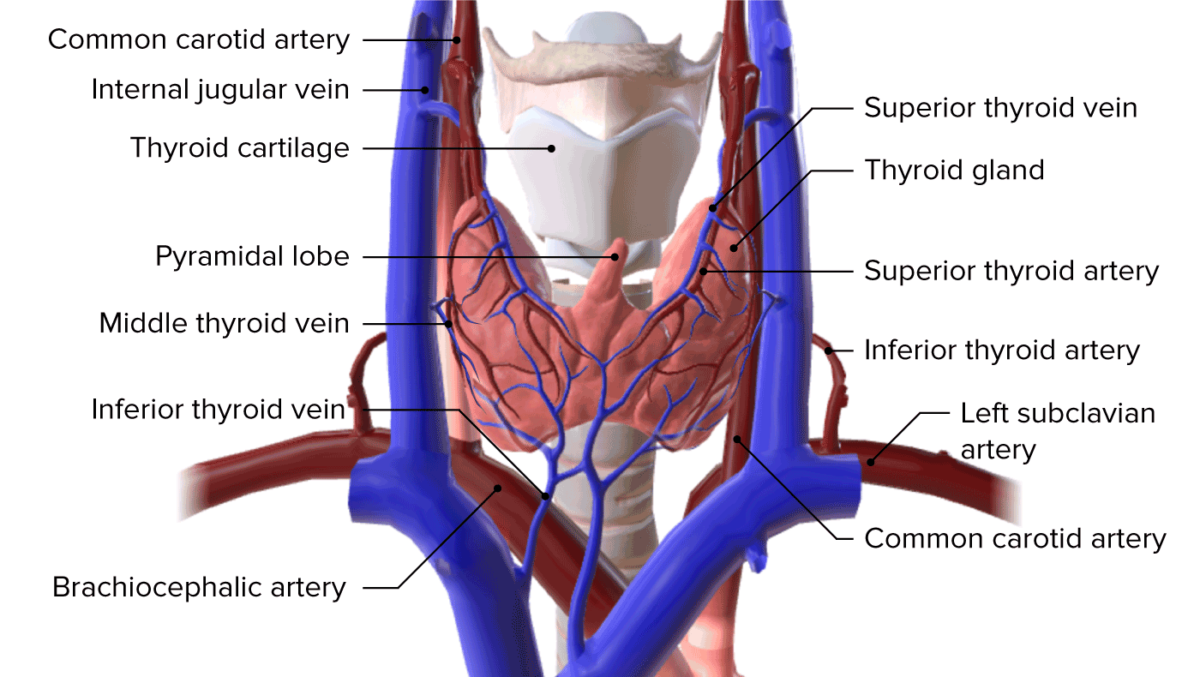
Blood supply to the thyroid gland
Image by BioDigital, edited by LecturioThe thyroid gland drains into multiple different lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy including:
The thyroid gland is primarily innervated by the ANS ANS The ans is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ans consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy.
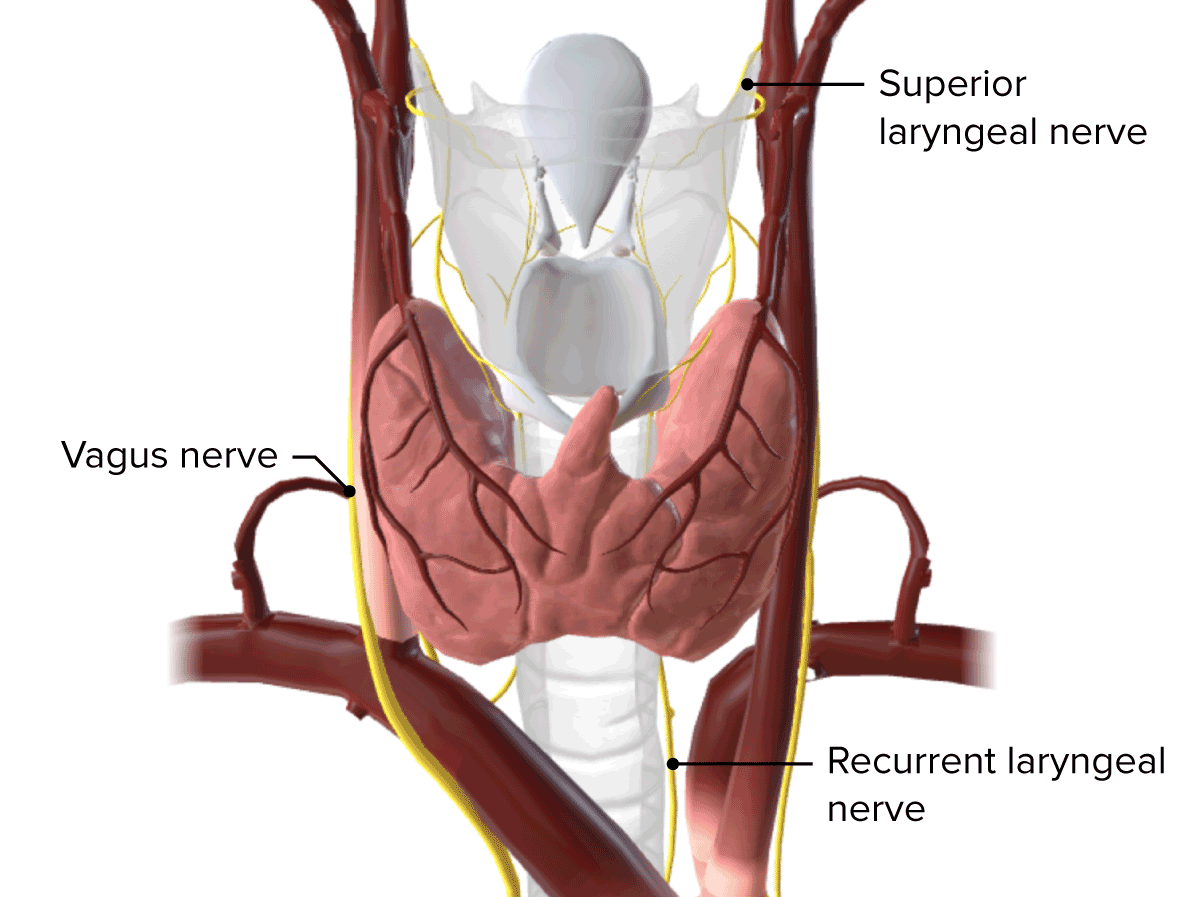
Innervation of the thyroid gland
Image by BioDigital, edited by LecturioThyroid cancer Thyroid cancer Thyroid cancer is a malignancy arising from the thyroid gland cells: thyroid follicular cells (papillary, follicular, and anaplastic carcinomas) and calcitonin-producing C cells (medullary carcinomas). Rare cancers are derived from the lymphocytes (lymphoma) and/or stromal and vascular elements (sarcoma). Thyroid Cancer: an uncommon cancer that can be managed well if detected early. Thyroid cancer Thyroid cancer Thyroid cancer is a malignancy arising from the thyroid gland cells: thyroid follicular cells (papillary, follicular, and anaplastic carcinomas) and calcitonin-producing C cells (medullary carcinomas). Rare cancers are derived from the lymphocytes (lymphoma) and/or stromal and vascular elements (sarcoma). Thyroid Cancer arises from either the follicular or parafollicular cells within the thyroid gland. There are several subtypes of thyroid cancer Thyroid cancer Thyroid cancer is a malignancy arising from the thyroid gland cells: thyroid follicular cells (papillary, follicular, and anaplastic carcinomas) and calcitonin-producing C cells (medullary carcinomas). Rare cancers are derived from the lymphocytes (lymphoma) and/or stromal and vascular elements (sarcoma). Thyroid Cancer depending on the cell of origin and the mutations that occur: mutated follicular cells can lead to papillary, follicular, and anaplastic carcinomas, whereas calcitonin-producing C cell mutations can result in medullary carcinomas.