Hypothyroidism is a condition characterized by a deficiency of thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types. Iodine Iodine A nonmetallic element of the halogen group that is represented by the atomic symbol I, atomic number 53, and atomic weight of 126. 90. It is a nutritionally essential element, especially important in thyroid hormone synthesis. In solution, it has anti-infective properties and is used topically. Thyroid Hormones deficiency is the most common cause worldwide, but Hashimoto's disease ( autoimmune thyroiditis Autoimmune thyroiditis Inflammatory disease of the thyroid gland due to autoimmune responses leading to lymphocytic infiltration of the gland. It is characterized by the presence of circulating thyroid antigen-specific T-cells and thyroid autoantibodies. The clinical signs can range from hypothyroidism to thyrotoxicosis depending on the type of autoimmune thyroiditis. Thyroiditis) is the leading cause in non–iodine-deficient regions. Primary hypothyroidism occurs with thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland disorders, while the central type arises from pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types and hypothalamic conditions. Thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types are integral in metabolic processes and in the development of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and other organs. Congenital Congenital Chorioretinitis hypothyroidism can result in significant mental disability Disability Determination of the degree of a physical, mental, or emotional handicap. The diagnosis is applied to legal qualification for benefits and income under disability insurance and to eligibility for social security and workman's compensation benefits. ABCDE Assessment due to the loss of thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types. The features of acquired hypothyroidism also reflect the effects of slowed organ function, such as fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia, bradycardia Bradycardia Bradyarrhythmia is a rhythm in which the heart rate is less than 60/min. Bradyarrhythmia can be physiologic, without symptoms or hemodynamic change. Pathologic bradyarrhythmia results in reduced cardiac output and hemodynamic instability causing syncope, dizziness, or dyspnea. Bradyarrhythmias, cold intolerance, and exertional dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea. Diagnosis is by thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy function testing. Elevated thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy stimulating hormone and low free thyroxine Thyroxine The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroid Hormones (T4) levels are noted. Treatment is with synthetic T4.
Last updated: May 17, 2024
Hypothyroidism is an endocrine disorder resulting from thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormone deficiency.
By onset:
By organs affected with disease:
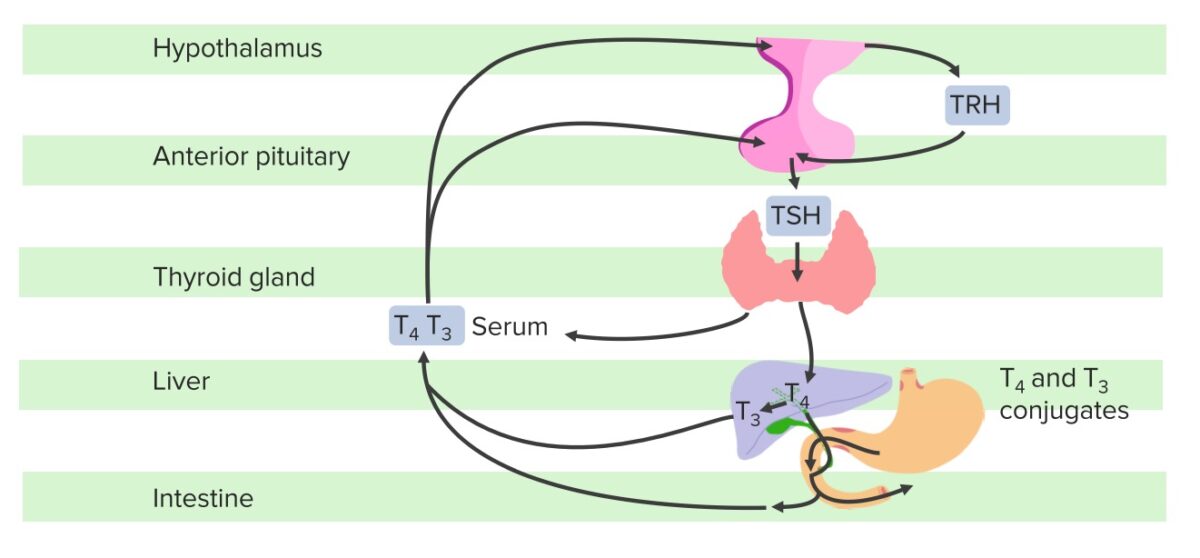
Schematic diagram of the hypothalamic–pituitary–thyroid axis:
The hypothalamus produces TRH, which stimulates the pituitary gland to synthesize and secrete TSH, which then stimulates the synthesis and secretion of T3 and T4 by the thyroid gland. T4 is converted to T3 in the liver and other tissues. A fraction of T4 and T3 is conjugated with glucuronide and sulfate in the liver, excreted in the bile, and partially hydrolyzed in the intestine; some of this fraction in the intestine may be reabsorbed. If the hypothalamus senses low FT3 and FT4, there will be an increase in TRH and subsequently, TSH; conversely, in this negative feedback loop, T3 and T4 inhibit the release of TSH from the hypothalamus and the pituitary once normal levels are achieved.
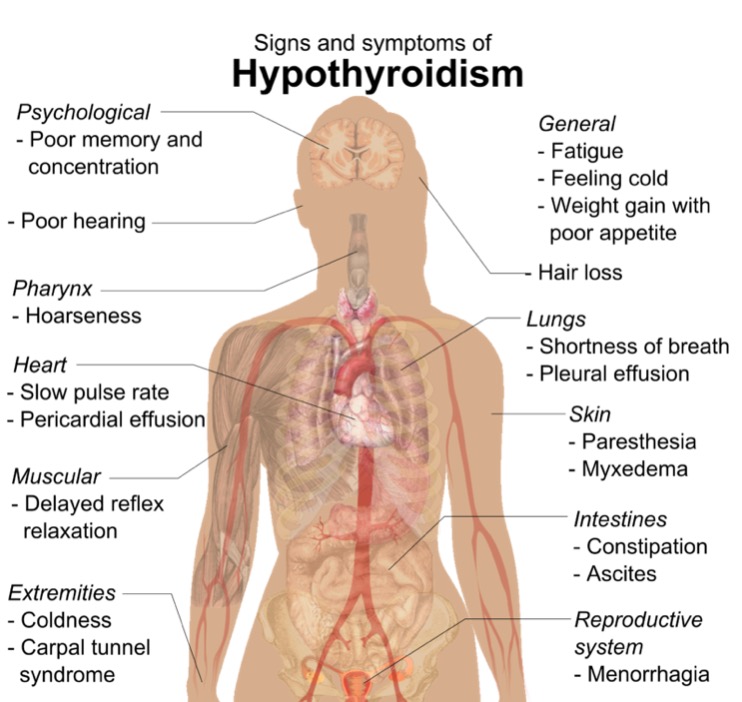
Diagram of the most common signs and symptoms of hypothyroidism
Image: “Symptoms and signs of hypothyroidism” by Mikael Häggström. License: CC0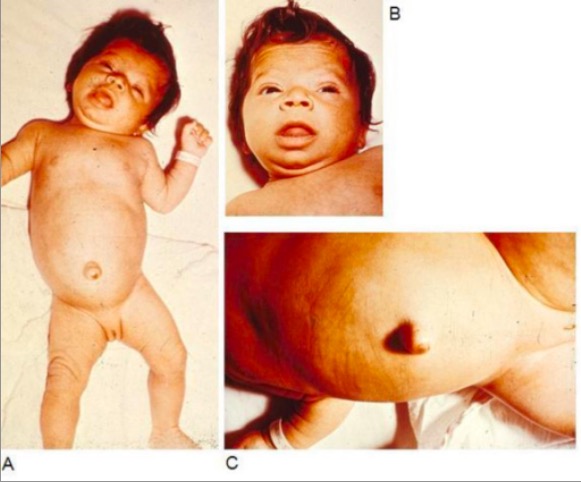
Infant with congenital hypothyroidism displaying typical signs and symptoms, such as hypotonia (A), myxedematous facies and macroglossia (B), and an umbilical hernia (C)
Image: “Infant with congenital hypothyroidism” by Department of Pediatrics, Division of Endocrinology, Oregon Health & Science University, 707 SW Gaines Street, Portland, OR, USA. License: CC BY 2.0Common signs and symptoms:
In the elderly:
Myxedema Myxedema A condition characterized by a dry, waxy type of swelling (edema) with abnormal deposits of mucopolysaccharides in the skin and other tissues. It is caused by a deficiency of thyroid hormones. The skin becomes puffy around the eyes and on the cheeks. The face is dull and expressionless with thickened nose and lips. Edema coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma:

A man with myxedema due to hypothyroidism:
Note the expressionless face, periorbital puffiness, pallor, peripheral edema, and massive ascites. Because it is curable, myxedema should be considered in every patient with conspicuous ascites, except perhaps those with widespread or terminal malignancy. The patient shown received thyroid replacement therapy, and all of his physical abnormalities resolved. If ascites persists after treatment, a coexisting cause should be sought.
Mandatory screening Screening Preoperative Care in all newborns:
Imaging:
Early diagnosis and treatment can prevent long-term mental disability Disability Determination of the degree of a physical, mental, or emotional handicap. The diagnosis is applied to legal qualification for benefits and income under disability insurance and to eligibility for social security and workman’s compensation benefits. ABCDE Assessment.
Thyroid function tests Thyroid Function Tests Blood tests used to evaluate the functioning of the thyroid gland. Ion Channel Myopathy:
Antibody testing:
Imaging studies:
Additional workup: