The process of bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types formation is called ossification. The 2 types of ossification are intramembranous ossification, in which bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types is developed directly from mesenchyme cells, and endochondral ossification Endochondral ossification A hyaline cartilage model is created from mesenchyme, then replaced with bone. Development of the Limbs, in which a hyaline cartilage Hyaline cartilage A type of cartilage characterized by a homogeneous amorphous matrix containing predominantly type II collagen and ground substance. Hyaline cartilage is found in articular cartilage; costal cartilage; laryngeal cartilages; and the nasal septum. Cartilage: Histology model is created 1st and then later replaced with bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types. Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types continues to grow into early adulthood at the epiphyseal plates, where chondrocytes Chondrocytes Polymorphic cells that form cartilage. Cartilage: Histology continue to divide, die, and be replaced with mineralized bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types. Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types mineralization occurs because the osteoblasts allow high levels of calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes and phosphate Phosphate Inorganic salts of phosphoric acid. Electrolytes to accumulate above critical threshold Threshold Minimum voltage necessary to generate an action potential (an all-or-none response) Skeletal Muscle Contraction levels within bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types.
Last updated: Mar 27, 2025
The formation of bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types is called ossification or osteogenesis.
The 2 primary types of ossification are:
The 2 primary types of bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types are compact bone Compact bone A smooth, solid outer layer of osseous tissue. Bones: Structure and Types and spongy bone Spongy bone A type of osseous tissue which makes up the inner part of bone. It has a spongy, honeycomb-like structure with struts or trabecula and contains the bone marrow. It has higher rate of bone remodeling turnover than cortical bone. Bones: Structure and Types.
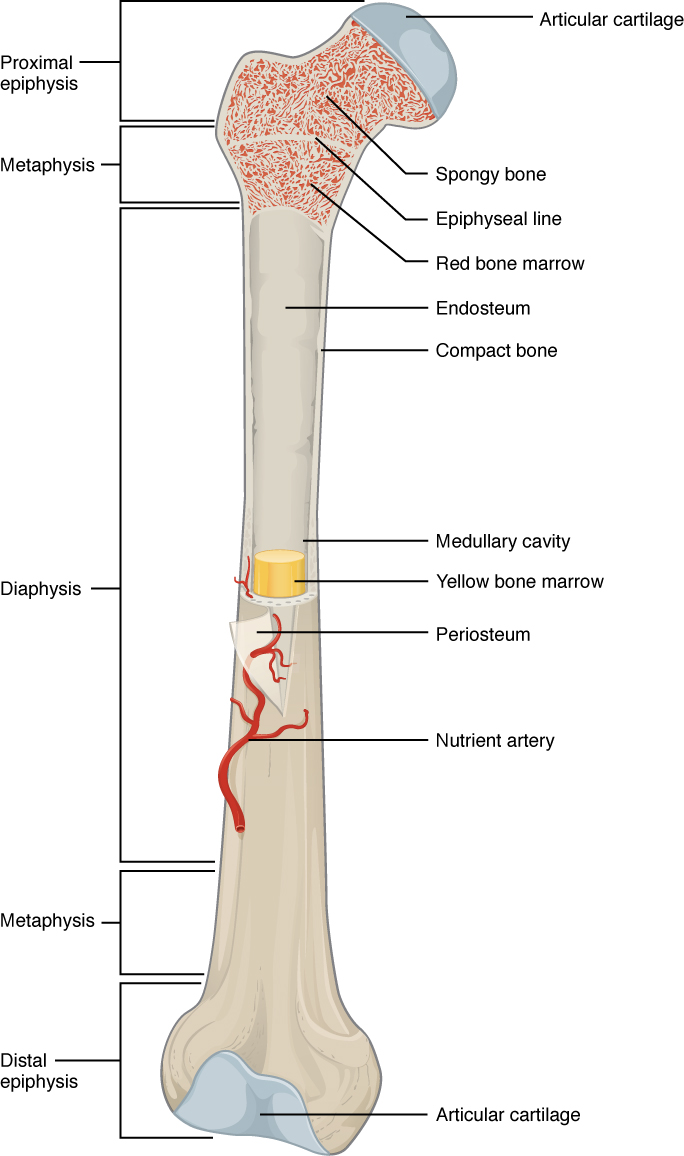
Structure of a long bone, here the femur, which is the primary bone in the thigh.
Image: “A typical long bone shows the gross anatomical characteristics of bone” by OpenStax College. License: CC BY 4.0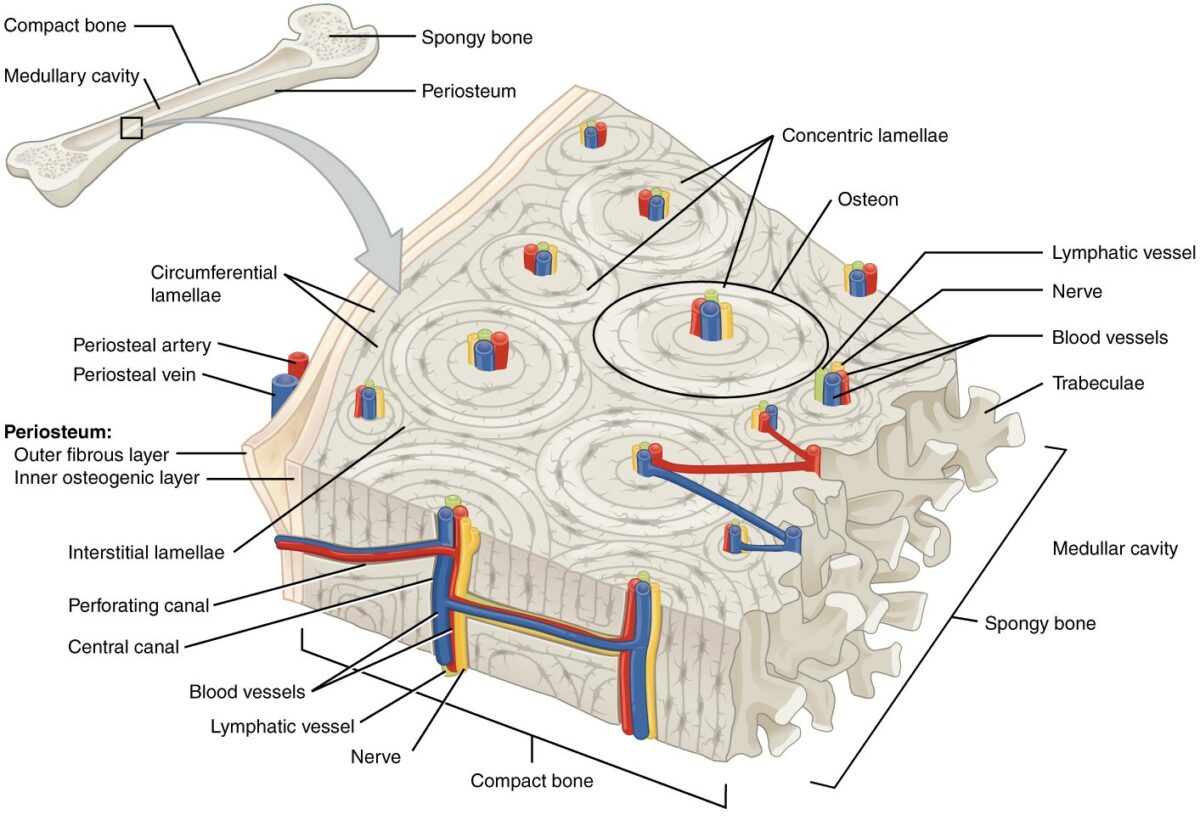
Microscopic structure of compact bone
Image: “This cross-sectional view of compact bone shows the basic structural unit, the osteon” by OpenStax College. License: CC BY 4.0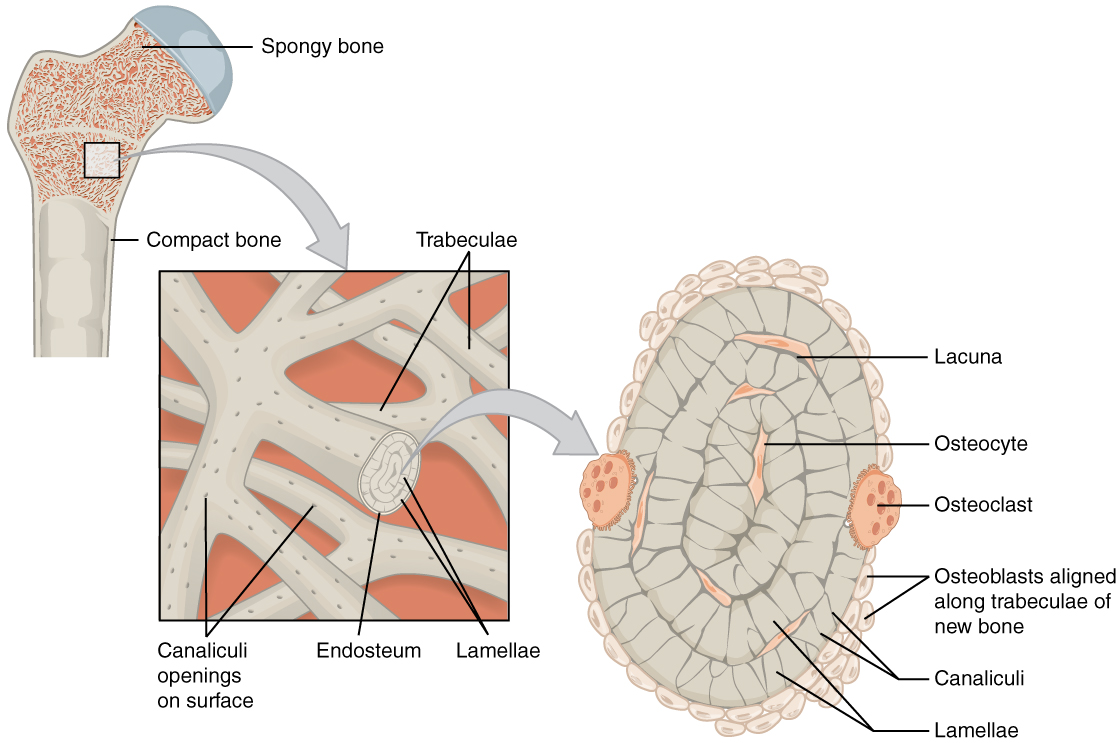
Microscopic structure of spongy bone
Image: “Spongy bone is composed of trabeculae that contain the osteocytes. Red marrow fills the spaces in some bones.” by OpenStax College. License: CC BY 4.0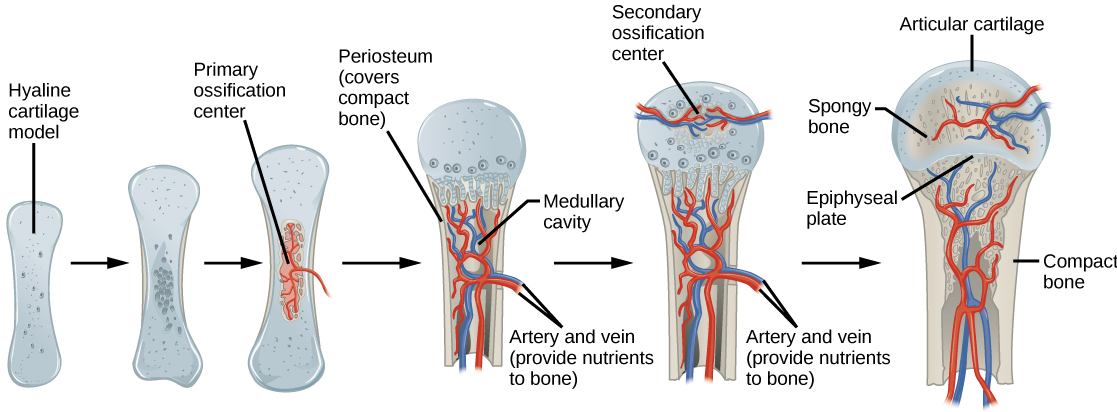
Process of endochondral ossification
Image: “Process of endochondral ossification” by CNX OpenStax. License: CC BY 4.0Intramembranous ossification is a direct conversion of mesenchymal cells into osseous tissue Osseous tissue Bones: Structure and Types.
These bones have a middle layer of spongy bone Spongy bone A type of osseous tissue which makes up the inner part of bone. It has a spongy, honeycomb-like structure with struts or trabecula and contains the bone marrow. It has higher rate of bone remodeling turnover than cortical bone. Bones: Structure and Types sandwiched between layers of compact bone Compact bone A smooth, solid outer layer of osseous tissue. Bones: Structure and Types:
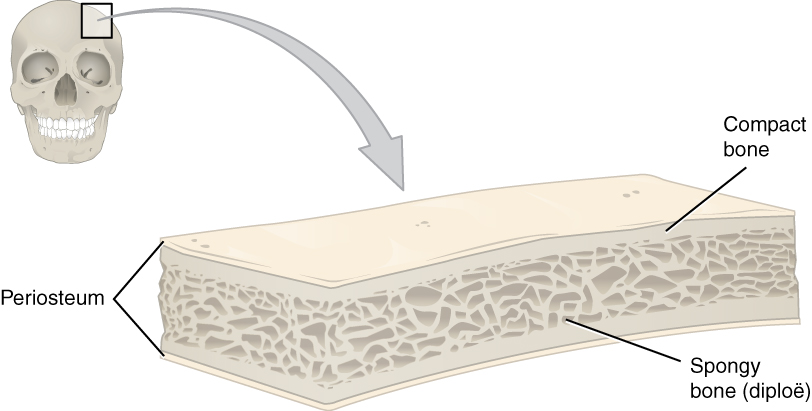
Structure of a flat bone
Image: “This cross-section of a flat bone shows the spongy bone (diploë) lined on either side by a layer of compact bone” by OpenStax College. License: CC BY 4.0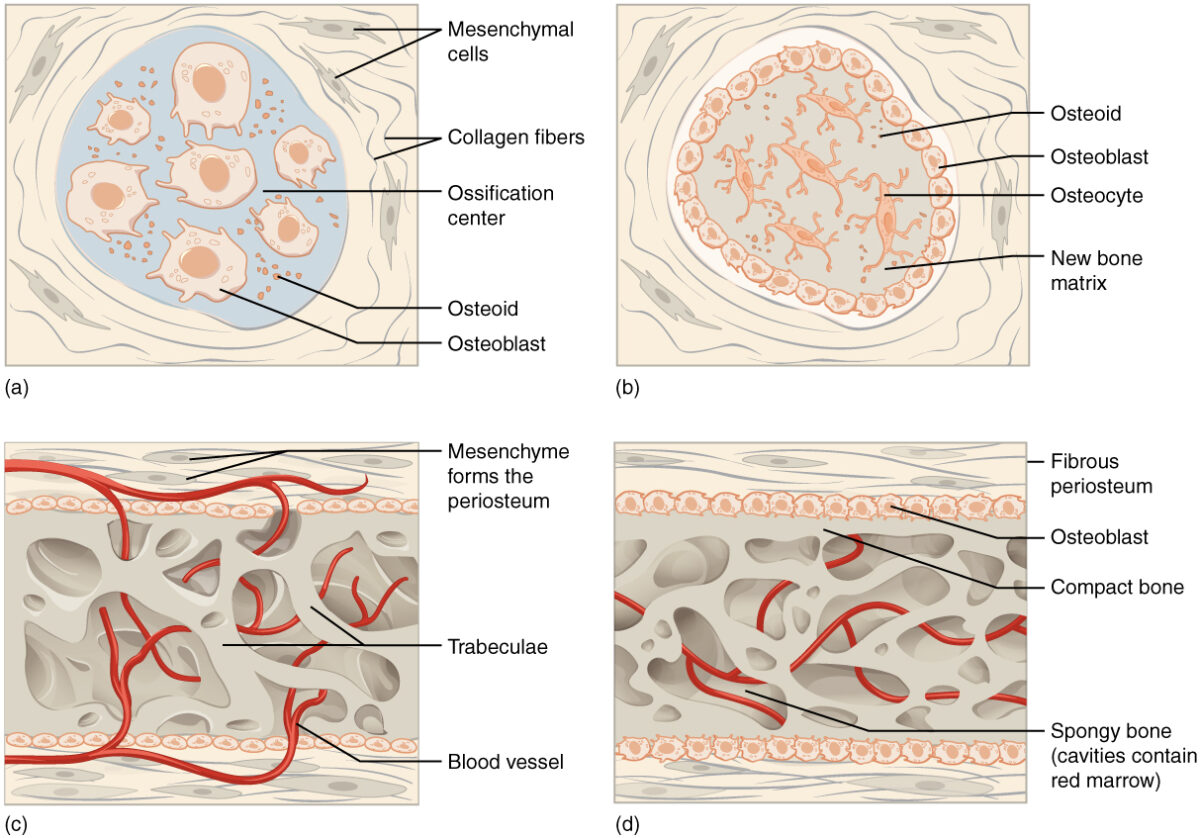
Process of intramembranous ossification
Image: “Intramembranous ossification follows four steps. (a) Mesenchymal cells group into clusters, and ossification centers form. (b) Secreted osteoid traps osteoblasts, which then become osteocytes. (c) Trabecular matrix and periosteum form. (d) Compact bone develops superficial to the trabecular bone, and crowded blood vessels condense into red marrow.” by OpenStax College. License: CC BY 4.0The epiphyseal plates are found in the metaphysis Metaphysis Bones: Structure and Types of long bones Long bones Length greater than width. Bones: Structure and Types, the transitional region between the diaphysis Diaphysis The shaft of long bones. Bones: Structure and Types (shaft) and epiphysis Epiphysis The head of a long bone that is separated from the shaft by the epiphyseal plate until bone growth stops. At that time, the plate disappears and the head and shaft are united. Bones: Structure and Types (ends). There are 5 distinct histologic zones:
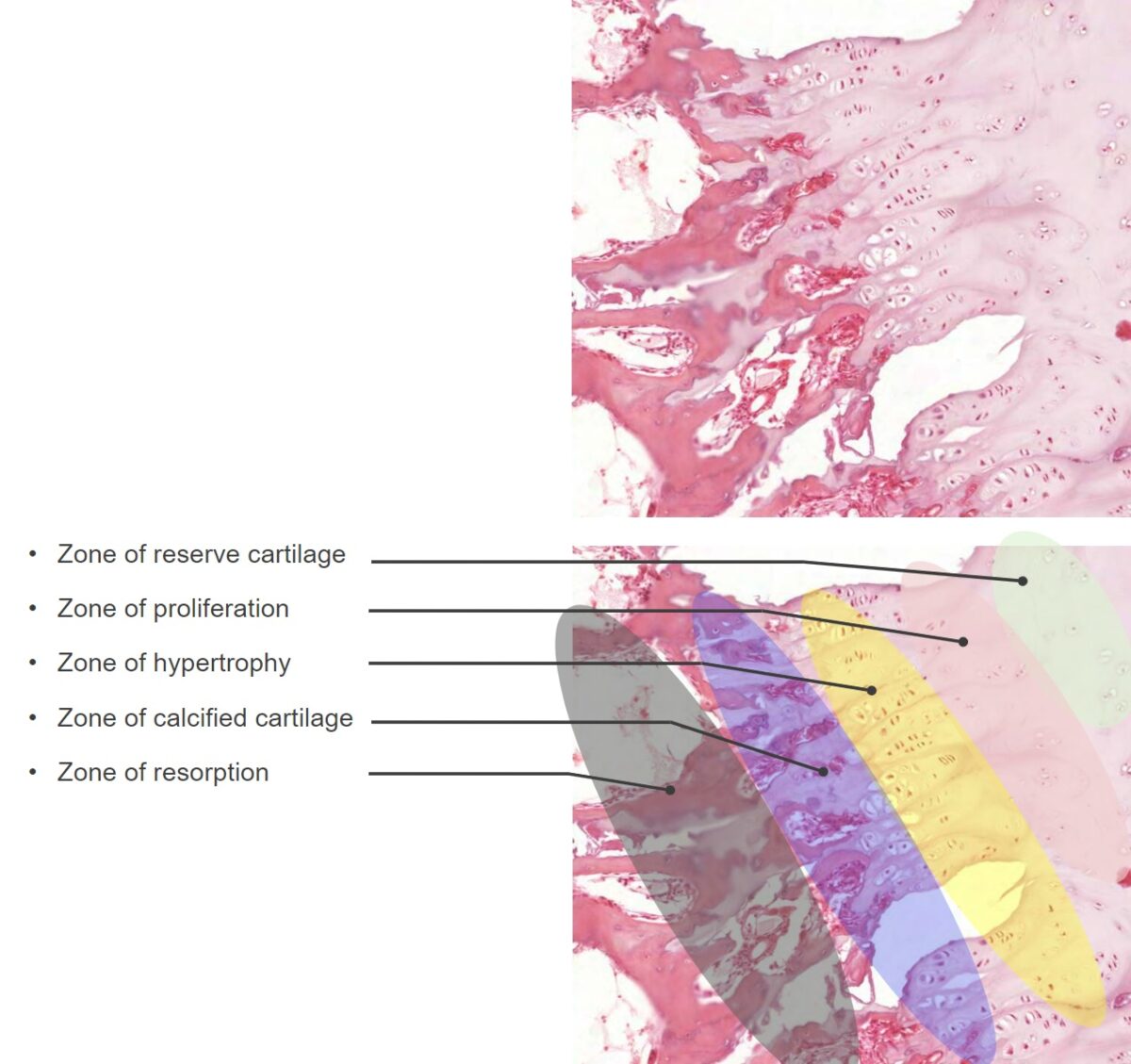
Histologic zones of the epiphyseal plates
Image by Lecturio.
Rickets
Image: “X-rays of both lower limbs showing severe bowing of the legs and diffuse osteopenia. It also shows dense transverse lines in the tibia suggestive of looser’s zones indicative of rickets” by Al-Sharafi BA et al. License: CC BY 4.0