Rickets and osteomalacia are disorders of decreased bone mineralization Bone mineralization Calcium (Ca2+) and phosphate (PO43–) combine to form hydroxyapatite crystals on the bone matrix. Bones: Development and Ossification. Rickets affects the cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology of the epiphyseal growth plates Growth Plates The area between the epiphysis and the diaphysis within which bone growth occurs. Osteosarcoma in children, while osteomalacia affects the sites of bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types turnover in children and adults. Although most cases of rickets and osteomalacia are due to vitamin D deficiency Vitamin D Deficiency A nutritional condition produced by a deficiency of vitamin D in the diet, insufficient production of vitamin D in the skin, inadequate absorption of vitamin D from the diet, or abnormal conversion of vitamin D to its bioactive metabolites. It is manifested clinically as rickets in children and osteomalacia in adults. Fat-soluble Vitamins and their Deficiencies, other genetic and nutritional disorders as well as medications can cause these disorders. Rickets commonly presents with skeletal deformities and growth abnormalities, while osteomalacia can present with bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, difficulty with ambulation and pathologic fractures. Diagnosis is made based on a combination of clinical findings, laboratory tests and imaging. Treatment includes vitamin D Vitamin D A vitamin that includes both cholecalciferols and ergocalciferols, which have the common effect of preventing or curing rickets in animals. It can also be viewed as a hormone since it can be formed in skin by action of ultraviolet rays upon the precursors, 7-dehydrocholesterol and ergosterol, and acts on vitamin D receptors to regulate calcium in opposition to parathyroid hormone. Fat-soluble Vitamins and their Deficiencies, calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes, and phosphorus supplementation.
Last updated: May 13, 2024
Rickets and osteomalacia are disorders of decreased bone mineralization Bone mineralization Calcium (Ca2+) and phosphate (PO43–) combine to form hydroxyapatite crystals on the bone matrix. Bones: Development and Ossification. Rickets affects the cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology of the epiphyseal growth plates Growth Plates The area between the epiphysis and the diaphysis within which bone growth occurs. Osteosarcoma in children, while osteomalacia affects the sites of bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types turnover in children and adults.
Rickets:
Osteomalacia:
Rickets and osteomalacia can be caused by deficiencies in vitamin D Vitamin D A vitamin that includes both cholecalciferols and ergocalciferols, which have the common effect of preventing or curing rickets in animals. It can also be viewed as a hormone since it can be formed in skin by action of ultraviolet rays upon the precursors, 7-dehydrocholesterol and ergosterol, and acts on vitamin D receptors to regulate calcium in opposition to parathyroid hormone. Fat-soluble Vitamins and their Deficiencies, calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes, or phosphorus, or by abnormalities in bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types matrix deposition.
Vitamin D-related (most common):
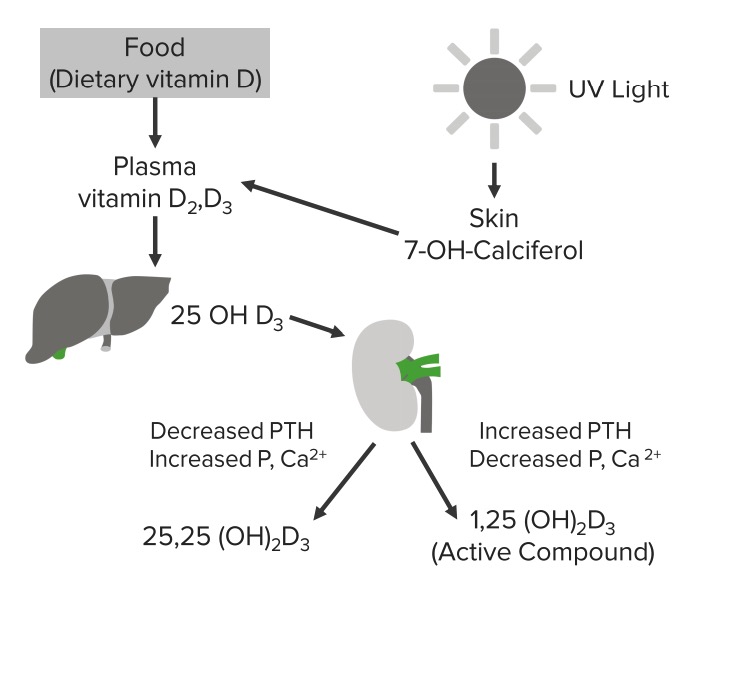
Schematic diagram depicting the vitamin D cycle
Image by Lecturio.Hypophosphatemia Hypophosphatemia A condition of an abnormally low level of phosphates in the blood. Bartter Syndrome related:
Inhibitors of mineralization:
Miscellaneous:
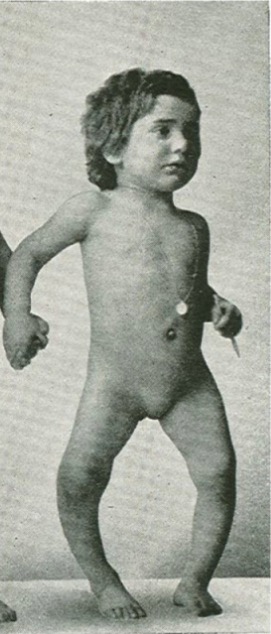
Child with rickets presents with the characteristic bowing of the long bones of the lower limbs (Genu varum).
Image: “Sister” by Vitamin D, Skin and Bone Research Laboratory, Section of Endocrinology, Nutrition, and Diabetes, Department of Medicine, Boston University Medical Center, 85 East Newton Street, M-1013, Boston, MA 02118, USA. License: CC BY 3.0, cropped by Lecturio.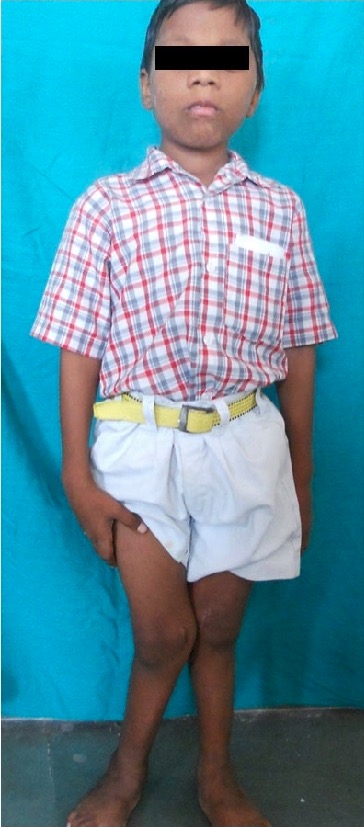
Genu valgum deformity of rickets
Image: “Showing genu valgum” by Department of Pedodontics and Preventive Dentistry, Sharad Pawar Dental College, Sawangi (M), Mahartashtra State, Wardha 442102, India. License: CC BY 4.0
Rickets:
Note the bowed legs and enlarged right wrist. Nutritional rickets is a condition in which children’s bones are too soft and do not develop properly due to a deficiency of vitamin D.
History:
Physical exam: skeletal deformities typical of rickets
Laboratory tests:
X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests imaging:

X-ray of the right tibia and fibula of a patient with osteomalacia:
Note the multiple pseudofractures (or “Looser zones”) and the buckle-type fracture of the tibia (arrow).

Wrist X-ray of a child with rickets shows metaphyseal cupping.
Image: “Radiological appearance” by Atatürk University, Faculty of Medicine, Department of Pediatric Endocrinology, Erzurum, Turkey. License: CC BY 2.5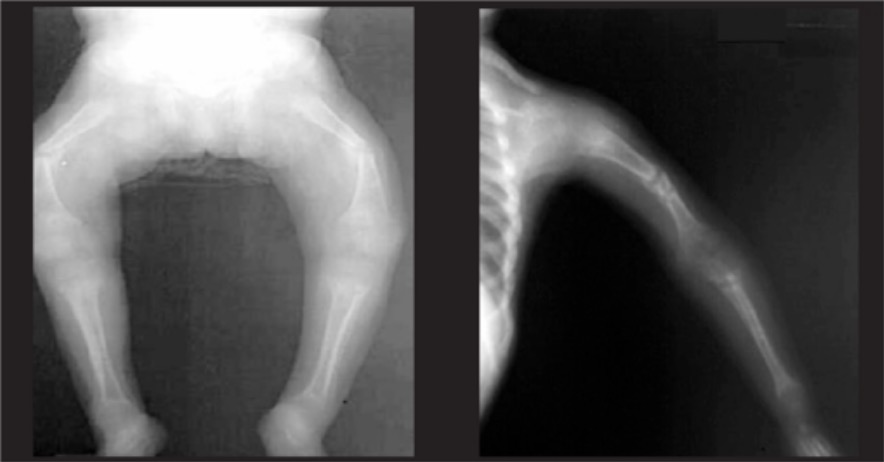
Anteroposterior X-ray of the limbs of a child with rickets shows bowing of the long bones.
Image: “Radiological findings in nutritional rickets (NR)” by Atatürk University, Faculty of Medicine, Department of Pediatric Endocrinology, Erzurum, Turkey. License: CC BY 2.5