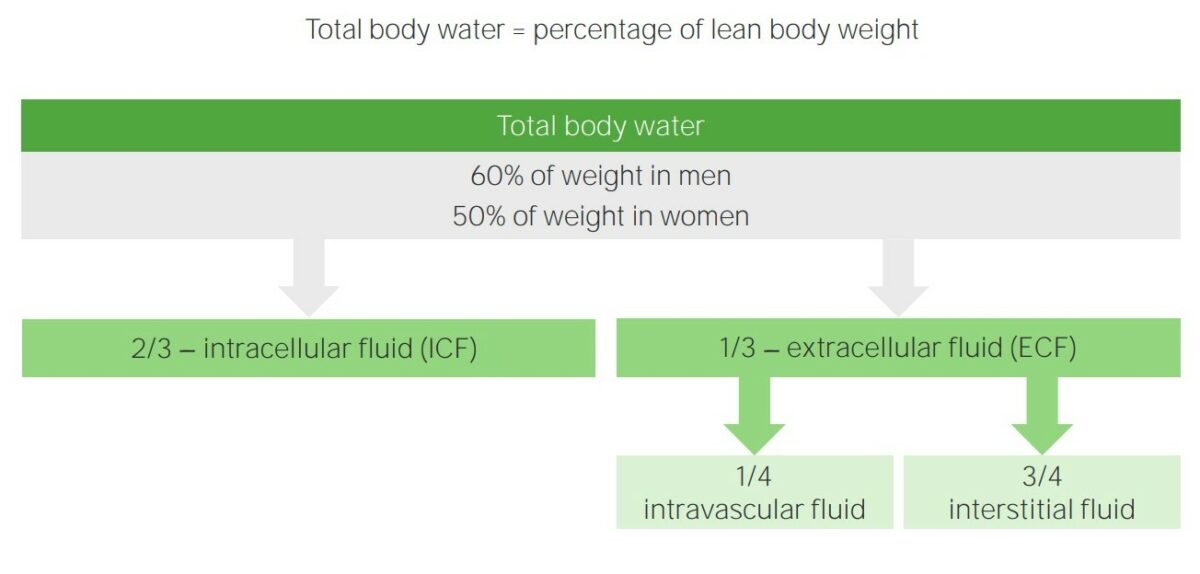
The adult human body is made up of 60% water and is divided into extracellular and intracellular fluid compartments. Extracellular fluid is present outside the cells and makes up ⅓ of the total body water. Intracellular fluid is present inside the cells and makes up ⅔ of the total body water. Intracellular and extracellular fluids are separated into compartments by semipermeable membranes, and the transport of fluid and ions is maintained by channels Channels The Cell: Cell Membrane in the cell membrane Cell Membrane A cell membrane (also known as the plasma membrane or plasmalemma) is a biological membrane that separates the cell contents from the outside environment. A cell membrane is composed of a phospholipid bilayer and proteins that function to protect cellular DNA and mediate the exchange of ions and molecules. The Cell: Cell Membrane. Each compartment contains different concentrations of ions and osmolar molecules. The relative charge and osmolarity Osmolarity The concentration of osmotically active particles in solution expressed in terms of osmoles of solute per liter of solution. Osmolality is expressed in terms of osmoles of solute per kilogram of solvent. Hypernatremia are maintained rigorously by the transport of water and substances between compartments. Hypernatremia Hypernatremia Hypernatremia is an elevated serum sodium concentration > 145 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled by the hypothalamus via the thirst mechanism and antidiuretic hormone (ADH) release. Hypernatremia occurs either from a lack of access to water or an excessive intake of sodium. Hypernatremia, hyponatremia Hyponatremia Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled via antidiuretic hormone (ADH) release from the hypothalamus and by the thirst mechanism. Hyponatremia, and edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema are the clinical conditions arising from disturbances in the maintenance of osmolarity Osmolarity The concentration of osmotically active particles in solution expressed in terms of osmoles of solute per liter of solution. Osmolality is expressed in terms of osmoles of solute per kilogram of solvent. Hypernatremia of the body fluid compartments.
Last updated: May 17, 2024
Water in the adult human body makes up approximately 60% of the total body weight. The fluid is distributed in various organs, organ systems, and tissues. The sum of the water in these tissues is known as total body water.
The total body water is distributed primarily between 2 compartments, namely, extracellular fluid (ECF) and intracellular fluid (ICF) compartments.
Body fluid compartments
Image by Lecturio.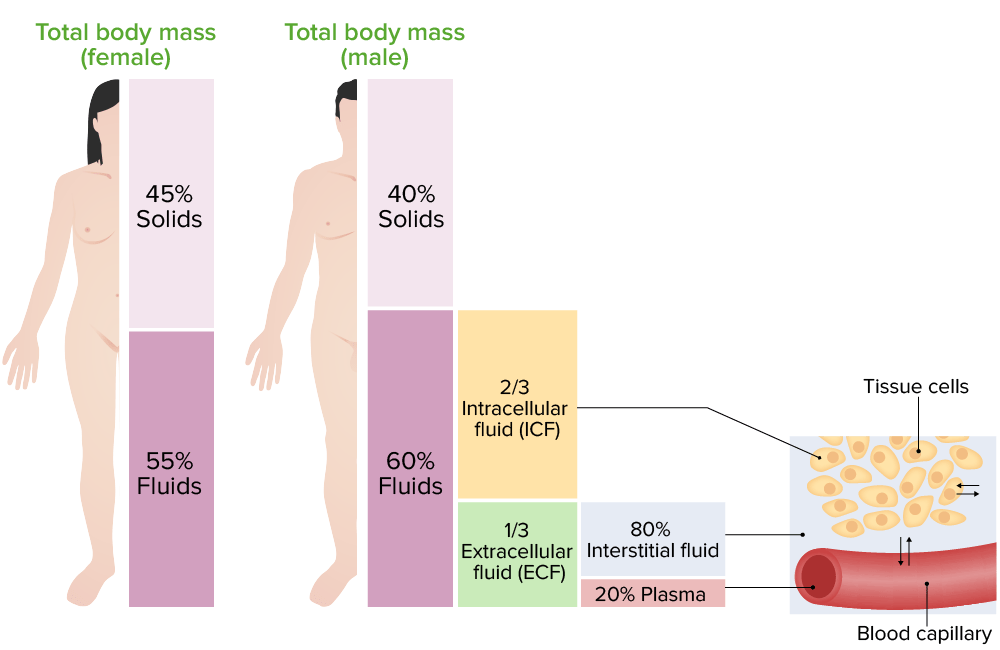
Distribution of body fluids:
On the left is an image showing the percentage of distribution of body fluids in males and females, in different compartments. On the right is an image representing the exchange of water among body fluid compartments.
Compartment volumes can be measured by determining the volume of distribution of an indicator substance. A known amount of an indicator is added to a compartment, and the indicator concentration in that compartment is measured after allowing sufficient time for uniform distribution throughout the compartment. The compartment volume is calculated as follows:
Volume = amount of the indicator / concentration of the indicator
| Volume | Indicators |
|---|---|
| Total body water | 3H2O, 2H2O, antipyrine |
| Extracellular fluid | 22Na, 125I-iothalamate, thiosulfate, inulin Inulin A starch found in the tubers and roots of many plants. Since it is hydrolyzable to fructose, it is classified as a fructosan. It has been used in physiologic investigation for determination of the rate of glomerular function. Glomerular Filtration |
| Intracellular fluid | Calculated as: (total body water — extracellular fluid volume) |
| Plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products volume | 125I-albumin, Evans blue dye (T-1824) |
| Blood volume | 51Cr-labeled RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology, or calculated as: (blood volume = plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products volume / (1 − hematocrit Hematocrit The volume of packed red blood cells in a blood specimen. The volume is measured by centrifugation in a tube with graduated markings, or with automated blood cell counters. It is an indicator of erythrocyte status in disease. For example, anemia shows a low value; polycythemia, a high value. Neonatal Polycythemia)) |
| Interstitial fluid | Calculated as: (extracellular fluid volume − plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products volume) |
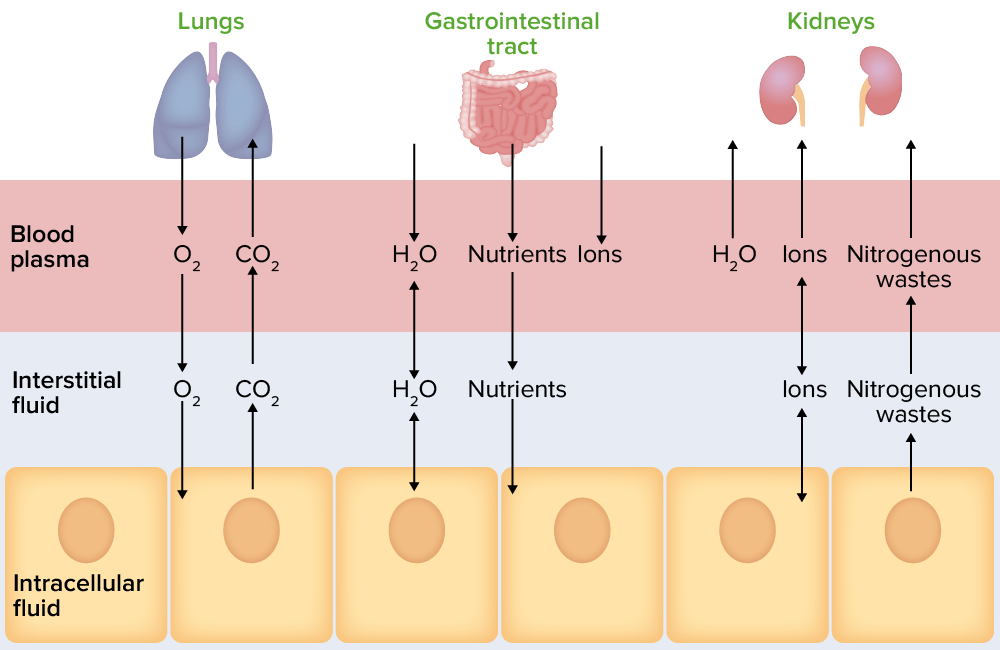
Illustration representing the movement of body fluids between compartments
Image by Lecturio.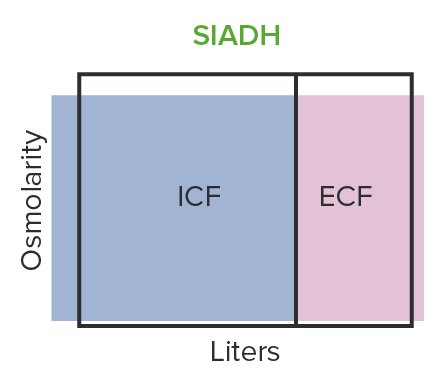
SIADH causes hypo-osmotic volume expansion:
The body retains too much water and produces excess antidiuretic hormone.
ICF: intracellular fluid
ECF: extracellular fluid
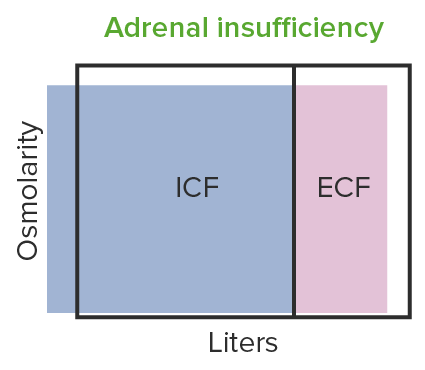
Hypo-osmotic volume contraction seen in adrenal insufficiency:
Low aldosterone leads to a decrease in tubular absorption of sodium, resulting in hypo-osmotic volume contraction.
ICF: intracellular fluid
ECF: extracellular fluid
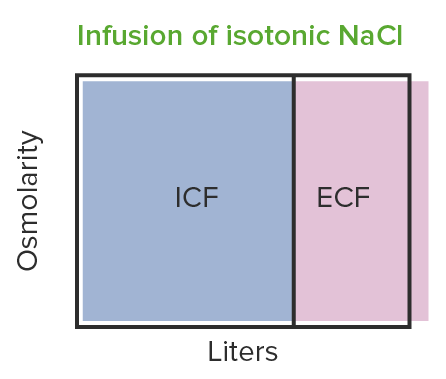
Infusion of isotonic NaCl results in iso-osmotic volume expansion:
Changes are observed in ECF (i.e. increase in volume), but the osmolarity remains the same.
ICF: intracellular fluid
ECF: extracellular fluid
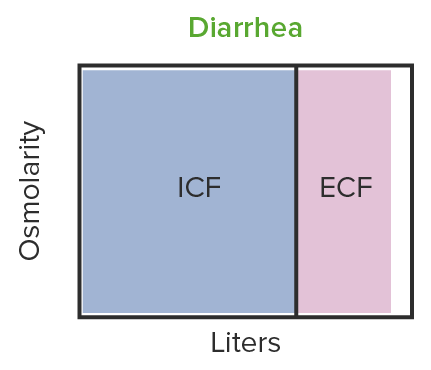
Iso-osmotic volume contraction is observed in diarrhea:
Fluid in diarrhea has the same osmolarity as extracellular fluid. The volume of ECF decreases, but not the osmolarity.
ICF: intracellular fluid
ECF: extracellular fluid
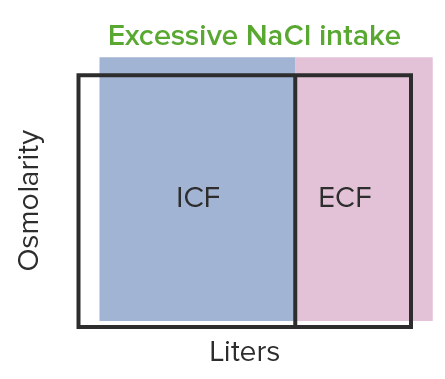
Hyper-osmotic volume expansion is seen in increased NaCl intake:
An increase in the sodium level causes retention of fluid.
ICF: intracellular fluid
ECF: extracellular fluid
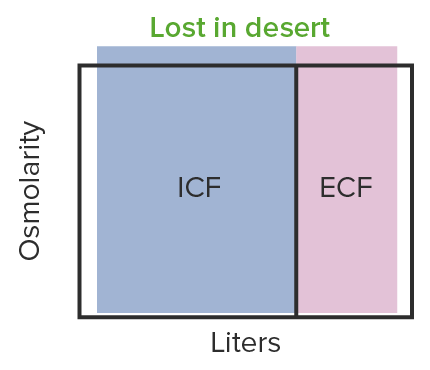
Hyper-osmotic volume contraction observed in dehydration causes hypotension:
The hypotension can reach a dangerously low level, depriving the organs of oxygen.
ICF: intracellular fluid
ECF: extracellular fluid
| Plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products | Interstitial fluid | Intracellular fluid | |
|---|---|---|---|
| (mOsm/L) | (mOsm/L) | (mOsm/L) | |
| Na+ | 142 | 139 | 14 |
| K+ | 4.2 | 4.0 | 140 |
| Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts)2+ | 1.3 | 1.2 | 0 |
| Mg2+ | 0.8 | 0.7 | 20 |
| Chloride Chloride Inorganic compounds derived from hydrochloric acid that contain the Cl- ion. Electrolytes (Cl–) | 106 | 108 | 4 |
| HCO3– | 24 | 28.3 | 10 |
| HPO42–, H2PO4– | 2 | 2 | 11 |
| SO42– | 0.5 | 0.5 | 1 |
| Phosphocreatine | 45 | ||
| Carnosine | 14 | ||
| Amino acids Amino acids Organic compounds that generally contain an amino (-NH2) and a carboxyl (-COOH) group. Twenty alpha-amino acids are the subunits which are polymerized to form proteins. Basics of Amino Acids | 2 | 2 | 8 |
| Creatinine | 0.2 | 0.2 | 9 |
| Lactate | 1.2 | 1.2 | 1.5 |
| ATP | 5 | ||
| Hexose monophosphate | 3.7 | ||
| Glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance | 5.6 | 5.6 | |
| Proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis | 1.2 | 0.2 | 4 |
| Urea Urea A compound formed in the liver from ammonia produced by the deamination of amino acids. It is the principal end product of protein catabolism and constitutes about one half of the total urinary solids. Urea Cycle | 4 | 1 | 4 |
| Others | 4.8 | 3.9 | 10 |
| Total mOsm/L | 299.8 | 300.8 | 301.2 |
| Corrected osmolar activity | 282.0 | 281.0 | 281.0 |