Hyponatremia is defined as a decreased serum sodium (sNa+) concentration less than 135 mEq/L. Serum sodium is the greatest contributor to plasma osmolality Plasma osmolality Volume Depletion and Dehydration, which is very tightly controlled via antidiuretic hormone Antidiuretic hormone Antidiuretic hormones released by the neurohypophysis of all vertebrates (structure varies with species) to regulate water balance and osmolarity. In general, vasopressin is a nonapeptide consisting of a six-amino-acid ring with a cysteine 1 to cysteine 6 disulfide bridge or an octapeptide containing a cystine. All mammals have arginine vasopressin except the pig with a lysine at position 8. Vasopressin, a vasoconstrictor, acts on the kidney collecting ducts to increase water reabsorption, increase blood volume and blood pressure. Hypernatremia (ADH) release from the posterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types and by the thirst mechanism. The basic pathophysiology of all etiologies of hyponatremia is an abnormal increase in total body water Total body water Body Fluid Compartments ( TBW TBW Body Fluid Compartments), which dilutes the total body sodium (TBNa+) concentration. The clinical presentation varies greatly, from asymptomatic to subtle cognitive deficits, seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures, and death. Management is guided by etiology, acuity, and duration of symptoms, usually involving oral fluid restriction or administration of IV fluids IV fluids Intravenous fluids are one of the most common interventions administered in medicine to approximate physiologic bodily fluids. Intravenous fluids are divided into 2 categories: crystalloid and colloid solutions. Intravenous fluids have a wide variety of indications, including intravascular volume expansion, electrolyte manipulation, and maintenance fluids. Intravenous Fluids that contain Na. Sodium must be replaced slowly, as overly rapid correction of hyponatremia can lead to irreversible neurologic complications and death, known as the osmotic demyelination Demyelination Multiple Sclerosis syndrome (ODS).
Last updated: Jun 21, 2025
The etiology of hyponatremia is determined by knowing the volume status Volume Status ACES and RUSH: Resuscitation Ultrasound Protocols, as well as the serum and urine osmolality Osmolality Plasma osmolality refers to the combined concentration of all solutes in the blood. Renal Sodium and Water Regulation.
Hypovolemic:
Euvolemic Euvolemic Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH):
Hypervolemic:
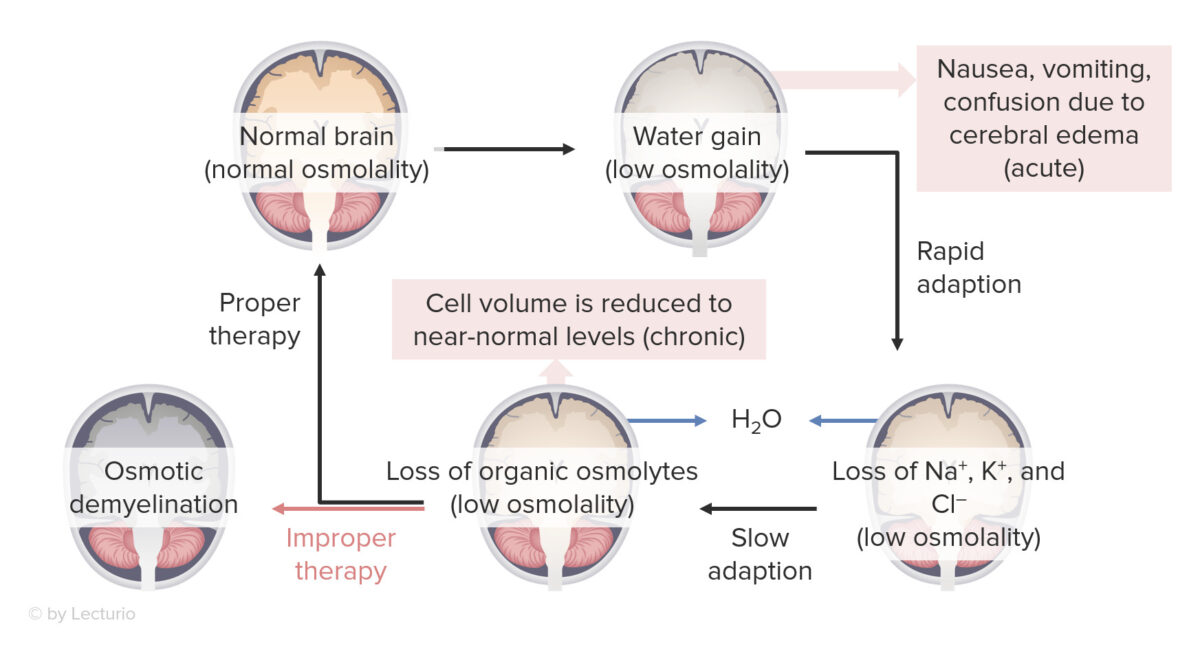
Effects of hyponatremia on the brain:
Osmotic demyelination syndrome can occur with overly rapid correction of severe hyponatremia (≤ 120 mEq/L).
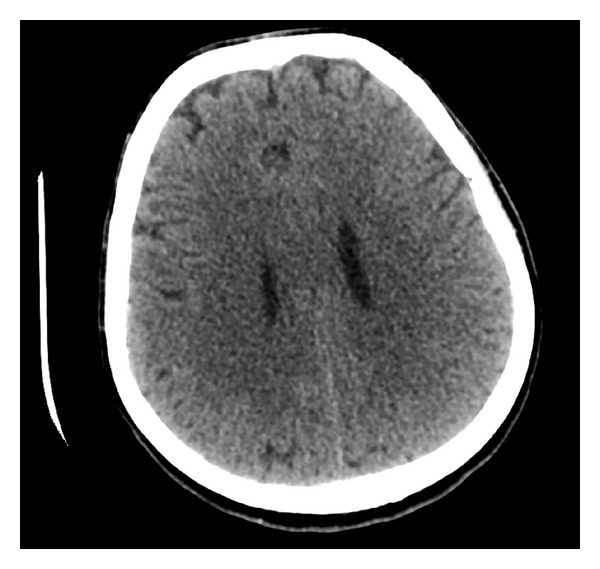
Supratentorial cerebral edema:
CT scan of a marathon runner with acute hyponatremia showing diffuse supratentorial cerebral edema
The 3 most important tests that need to be completed are:
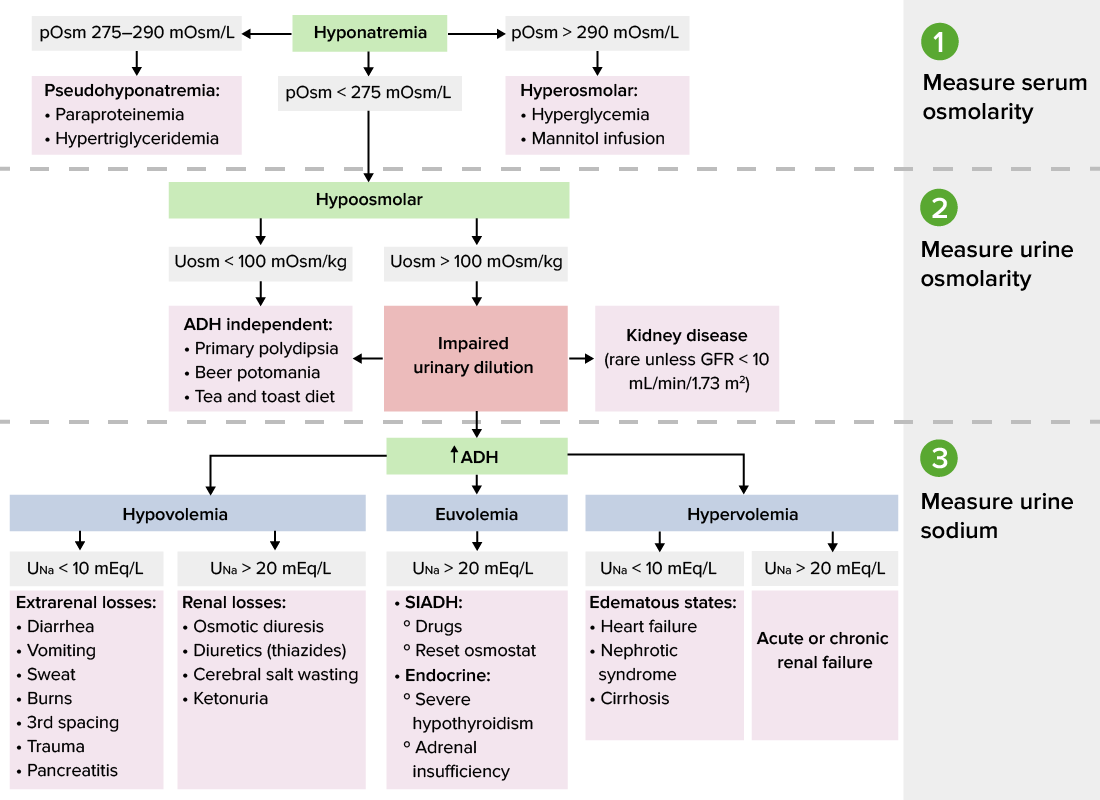
Diagnostic algorithm for hyponatremia
Image by Lecturio.Urinary sodium must be interpreted in the context of volume status Volume Status ACES and RUSH: Resuscitation Ultrasound Protocols.
Acuity and severity of symptoms are the primary determinants of this, and the aggressiveness and urgency of treatment will vary according to the risk assessment Risk assessment The qualitative or quantitative estimation of the likelihood of adverse effects that may result from exposure to specified health hazards or from the absence of beneficial influences. Preoperative Care.
Acuity:
Symptom severity:
Specific risk factors for ODS:
Involves giving 3% NaCl ( hypertonic Hypertonic Solutions that have a greater osmotic pressure than a reference solution such as blood, plasma, or interstitial fluid. Renal Sodium and Water Regulation saline) in order to increase the sNa+ by 6 mEq/L within several hours.
Severe (sNa+ < 125 mEq/L):
Moderate (sNa+ 125–130):
Mild (sNa+ > 130):