Respiratory failure is a syndrome that develops when the respiratory system is unable to maintain oxygenation and/or ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing. Respiratory failure may be acute or chronic and is classified as hypoxemic, hypercapnic, or a combination of the two. A number of etiologies exist, including diseases of the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy, cardiovascular, and nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with respiratory failure may present with dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, tachypnea Tachypnea Increased respiratory rate. Pulmonary Examination, and altered mental status Altered Mental Status Sepsis in Children. The diagnosis is made through measurement of arterial blood gas Arterial blood gas Respiratory Alkalosis and supplemented with laboratory and imaging studies to elicit an etiology. Management involves treating the underlying cause, supplemental oxygen administration, and mechanical ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing for severe cases.
Last updated: May 17, 2024
Respiratory failure is a syndrome that develops when the respiratory system is unable to maintain oxygenation and/or ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing.
Respiratory failure may be classified based on:
The time course:
The underlying issue:
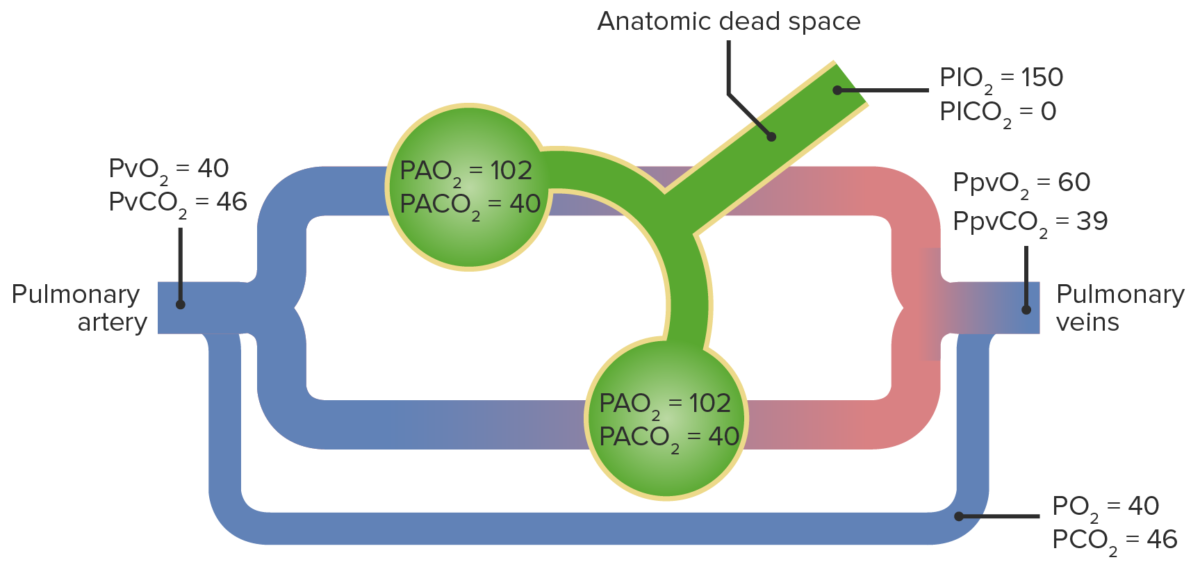
Diagram of a right-to-left shunt resulting in hypoxemia:
A cardiac or pulmonary issue causes deoxygenated blood to skip gas exchange. When this later mixes with oxygenated blood, the arterial pressure of O2 is reduced.
PA: alveolar partial pressure
PI: inspired partial pressure
Pv: venous partial pressure
Ppv: pulmonary venous partial pressure
A mismatch between ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing and perfusion occurs from a disease process resulting in either:
Note: 100% oxygen 100% Oxygen Cluster Headaches administration can correct oxygenation in V/Q mismatch.
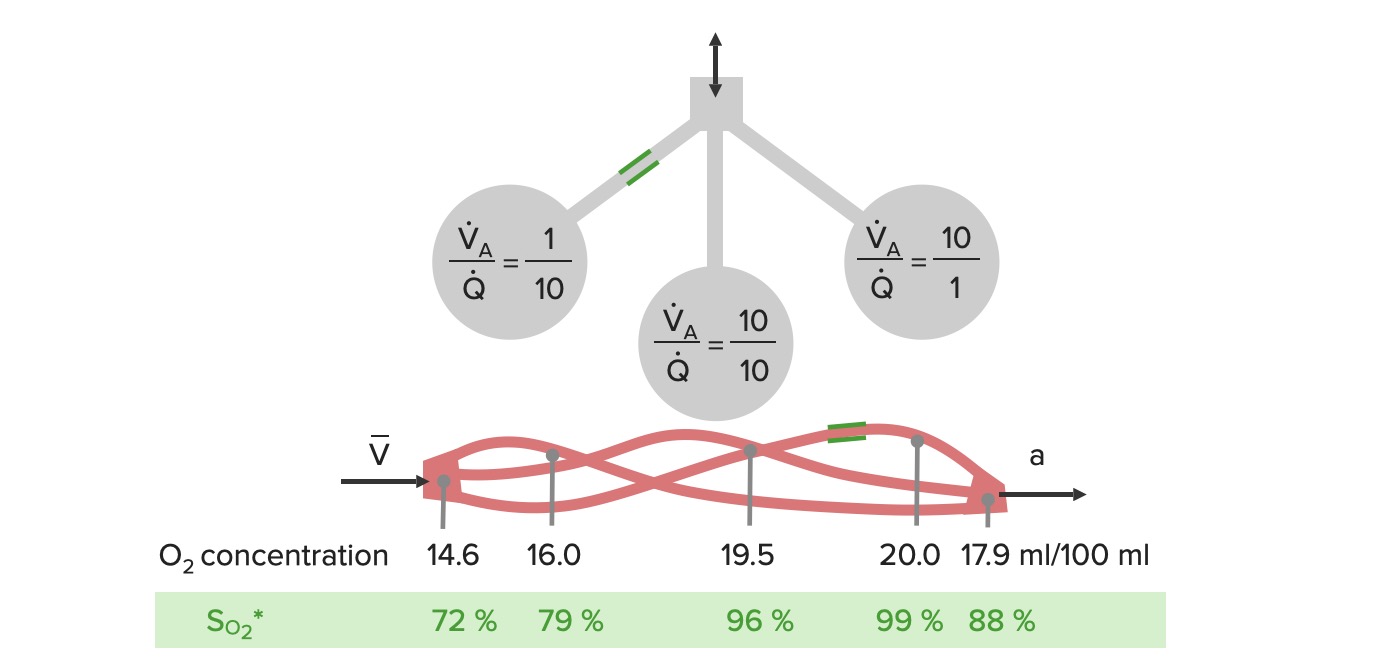
Diagrammatic examples of ventilation (V) to perfusion (Q) mismatch:
The left side of the diagram shows an example of low ventilation to an alveolus and normal perfusion, resulting in an oxygen saturation of 79% (low V/Q ratio).
In the middle, perfusion and ventilation are matched, which allows appropriate oxygenation of the blood.
On the right, there is normal ventilation, but low perfusion (high V/Q ratio), which provides more complete oxygenation, but there is less blood flow.
When the blood from these vessels combine, the oxygenation from the middle and right alveoli is not enough to compensate for the poor ventilation of the left alveolus.

Cyanosis on a patient’s face due to hypoxemia
Image: “Clinical signs of chronic hypoxaemia” by Maximilian Patzig et al. License: CC BY 4.0, edited by Lecturio.An arterial blood gas Arterial blood gas Respiratory Alkalosis (ABG) analysis is required in the diagnosis of respiratory failure. It measures and calculates components in arterial blood:
The following parameters are used to define hypoxemic and hypercapnic respiratory failure:
Hypoxemic respiratory failure:
Hypercapnic respiratory failure:
Once hypoxemic respiratory failure is established, the alveolar–arterial (A-a) gradient can be used to help in understanding the potential underlying etiology.
The following can be done to evaluate potential causes of respiratory failure. The workup should be tailored to the patient’s presentation and clinical suspicion.
Laboratory evaluation:
Pulmonary function tests:
Imaging:
Management of respiratory failure is supportive and focuses on maintaining adequate oxygenation and ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing until the underlying condition can be treated.
General principles:
Options:
Noninvasive positive-pressure ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing provides ventilatory support without placing an artificial airway Airway ABCDE Assessment.
Indications:
Best suited for:
Options:
Indications:
General principles:
Parameters:
Extracorporeal membrane oxygenation is an advanced therapy utilizing prolonged cardiopulmonary bypass to oxygenate blood and remove CO₂.
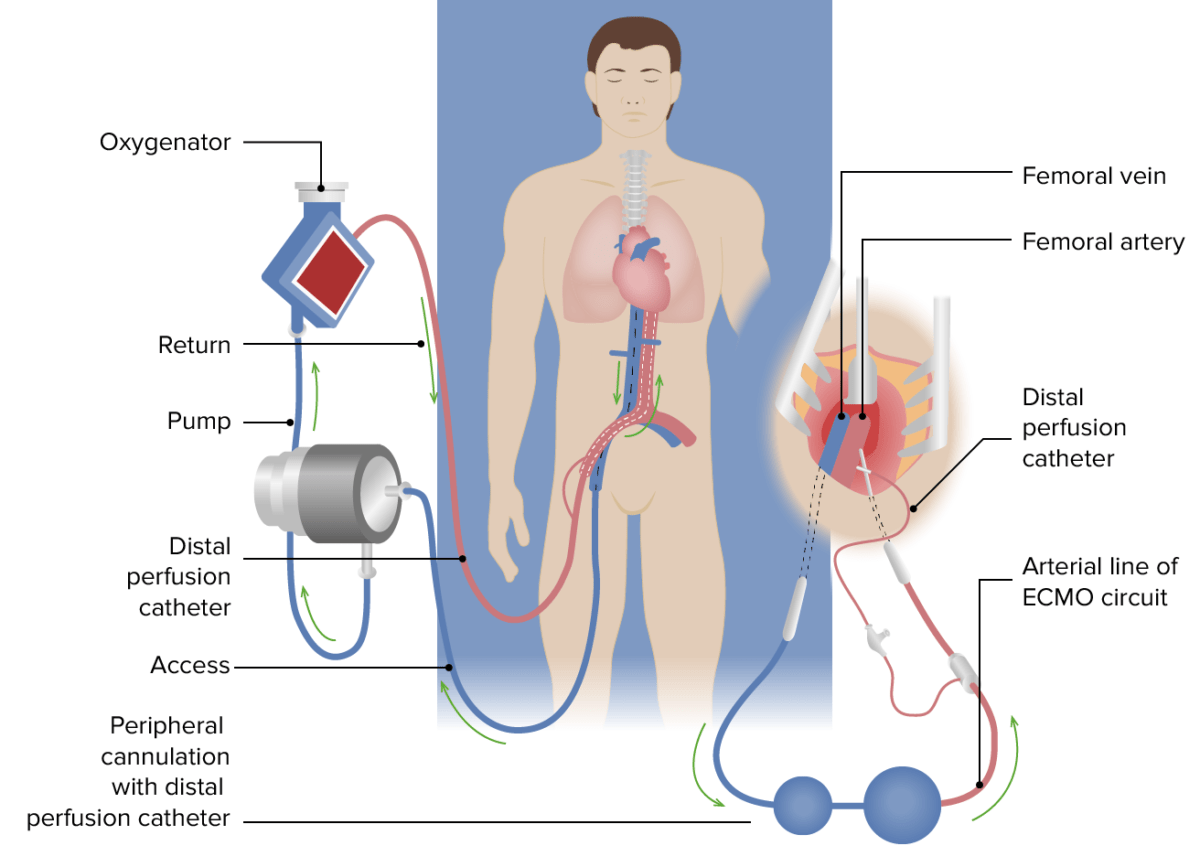
Venovenous ECMO for respiratory failure:
Venous blood (blue) is drained, via a cannula positioned at the inferior vena cava, to the right atrial junction and passes through the extracorporeal membrane, where oxygenation and CO2 removal occurs. The now oxygenated blood (red) is returned via a return cannula positioned in the common iliac artery or the descending aorta. The distal perfusion catheter, applied after ECMO support is established, is inserted into the superficial femoral artery distal to the insertion point of the femoral return cannula and supplies oxygenated blood to the distal limb to prevent distal limb ischemia.